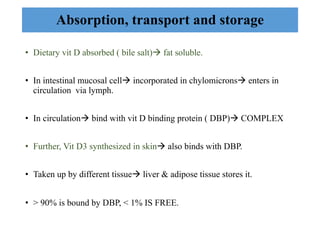
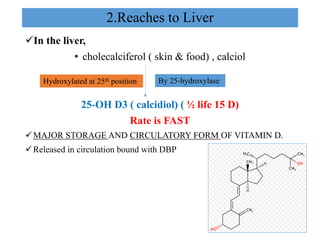
Vitamin D can be obtained through dietary sources like fish, eggs, and fortified foods, but it is also synthesized in the skin upon exposure to sunlight, making it both a vitamin and a hormone. Vitamin D is absorbed in the small intestine and transported through the bloodstream bound to vitamin D binding protein. In the liver and kidneys, vitamin D undergoes hydroxylation reactions to produce calcidiol and the active form calcitriol, which regulates calcium and phosphate levels in the blood by increasing their absorption in the intestine and mobilization from bone.