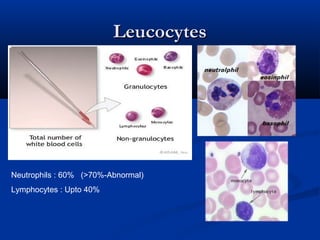
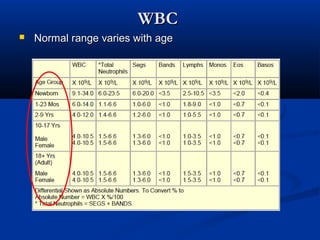
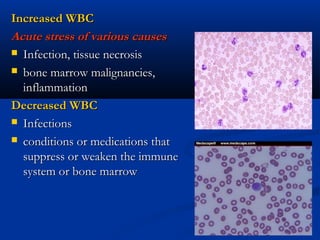
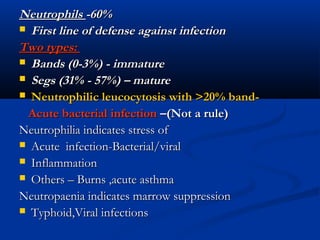
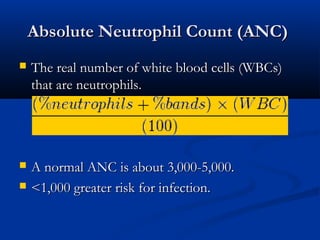
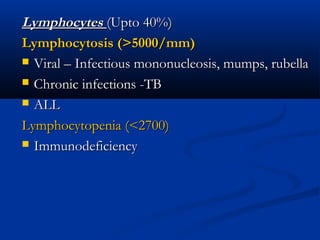
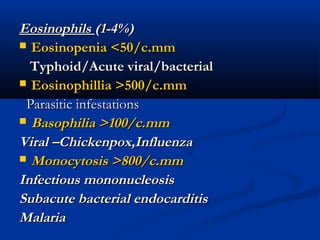
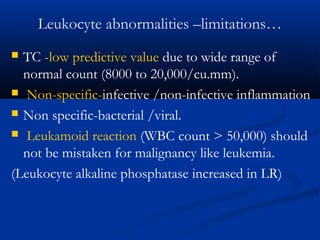
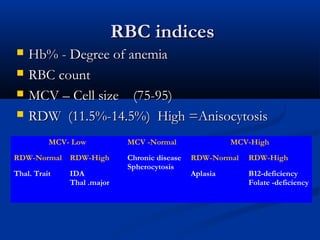
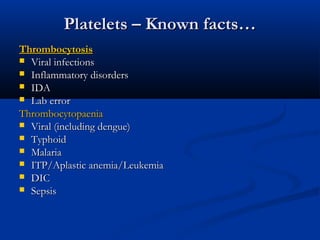
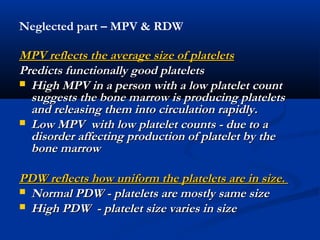
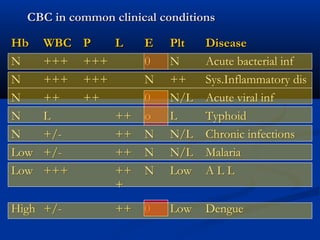
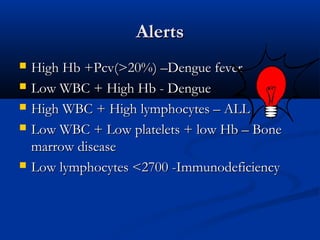
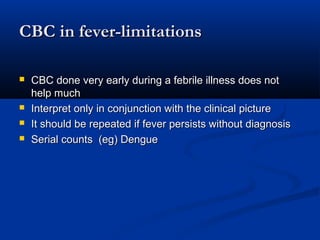
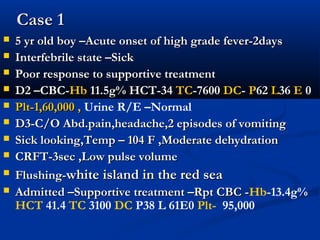
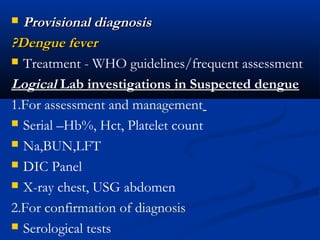
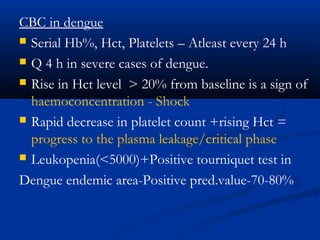
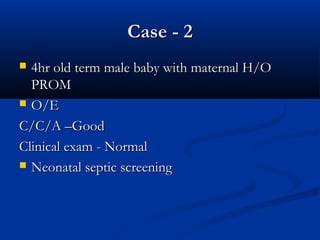
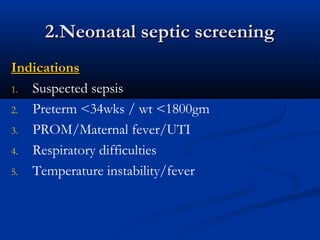
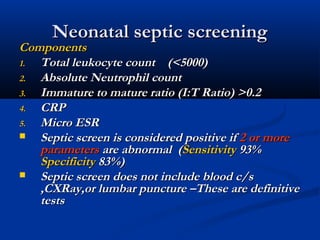
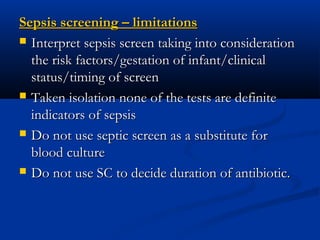
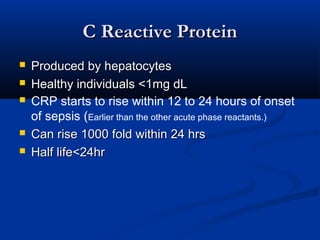
This document discusses common laboratory investigations in pediatric practice, with a focus on the complete blood count (CBC). It provides details on the normal ranges and clinical significance of various CBC components, including white blood cell count and differentials, red blood cell indices, platelet count, and peripheral smear findings. A case example of a child with suspected dengue fever is presented, along with how CBC trends can help monitor the condition and guide management. Guidelines for neonatal septic screening are also reviewed.