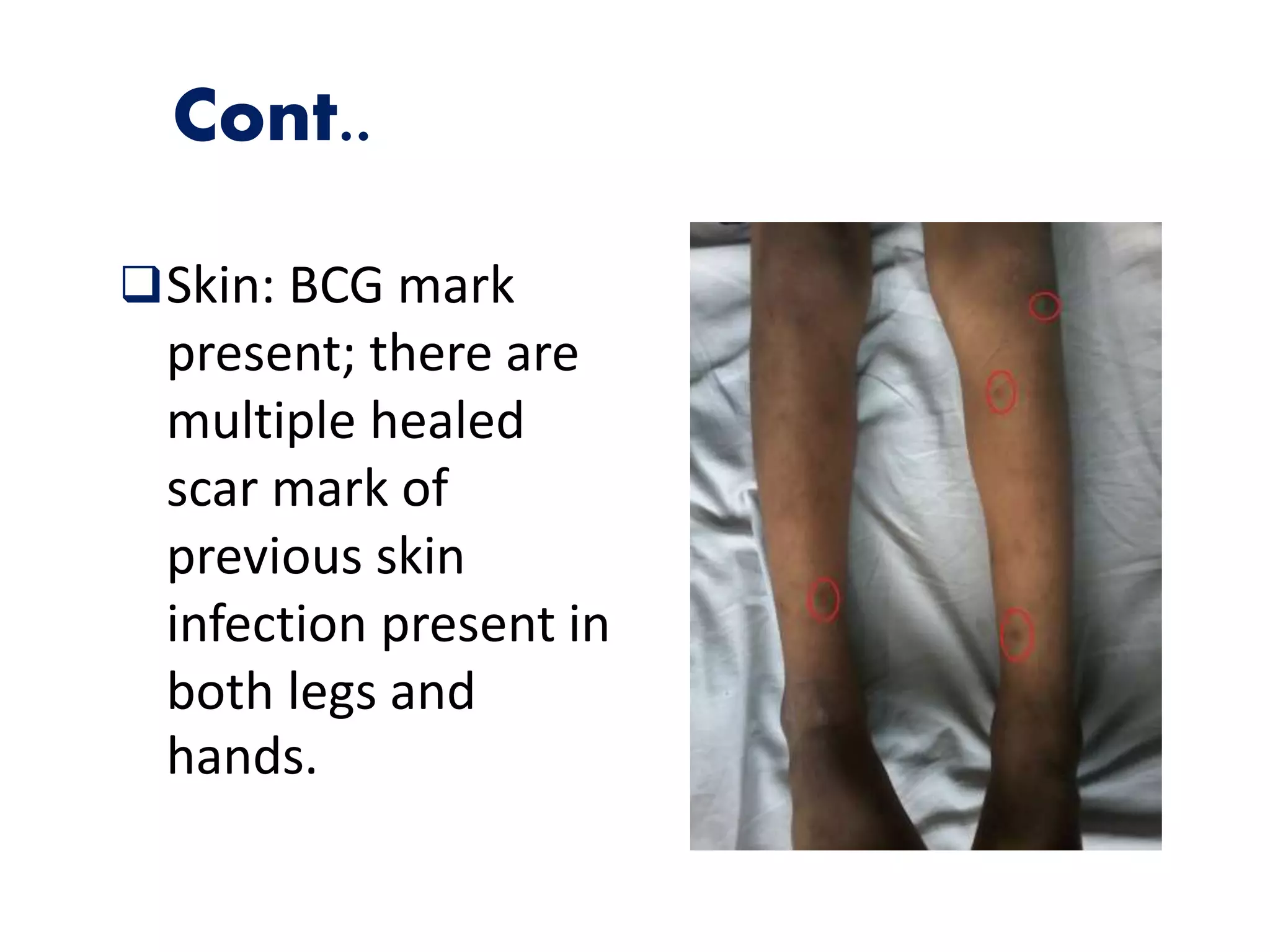
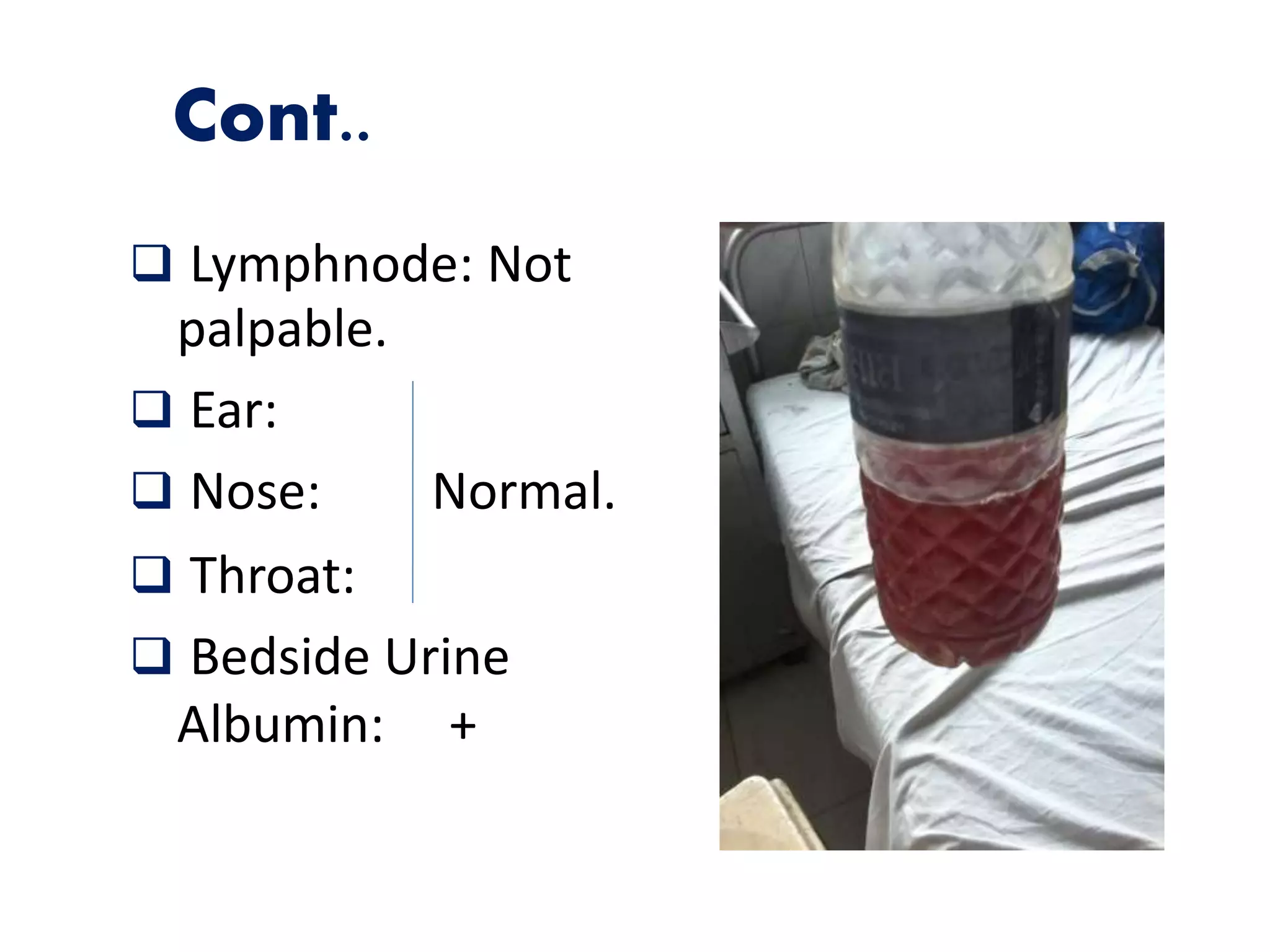
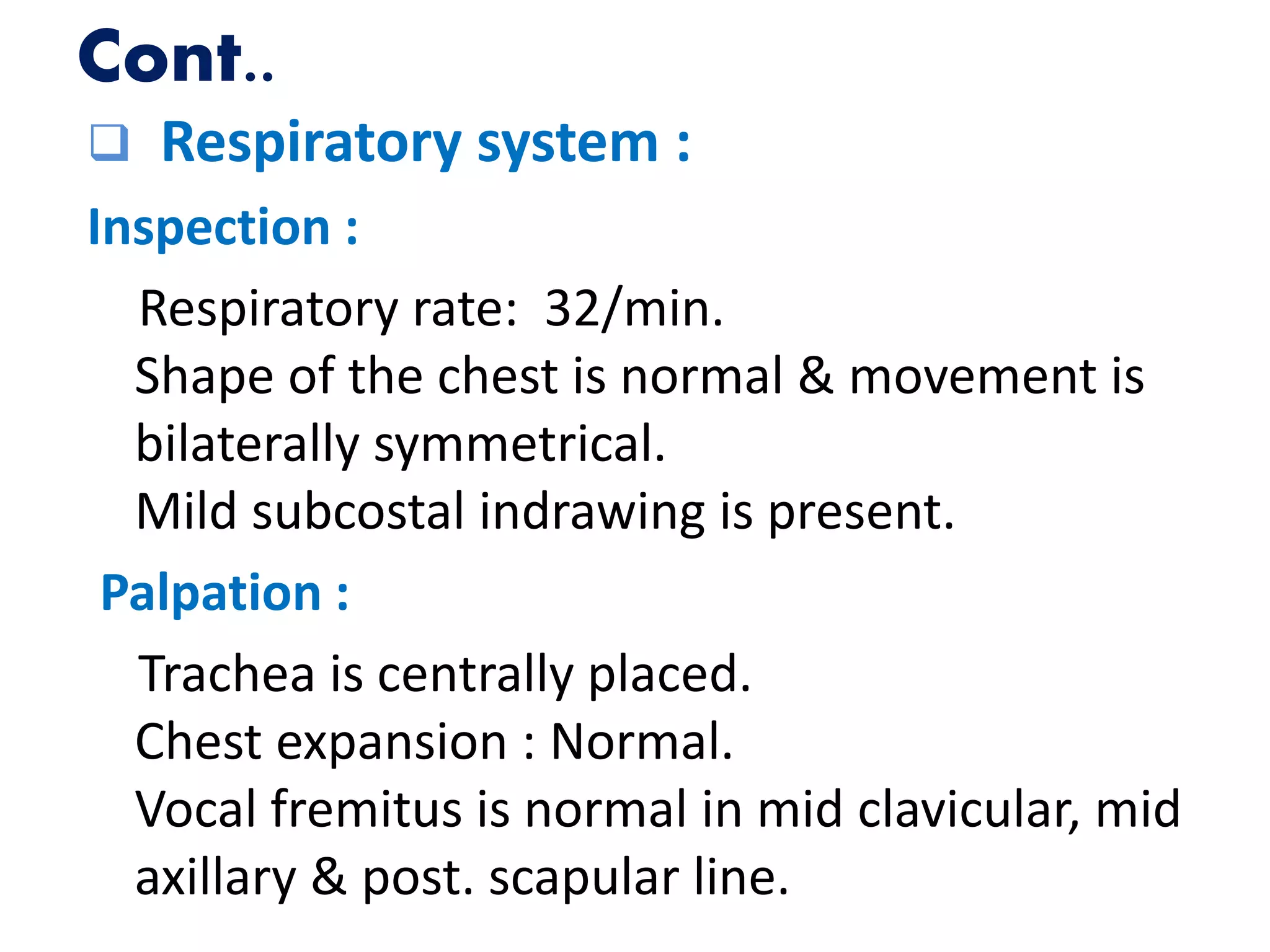
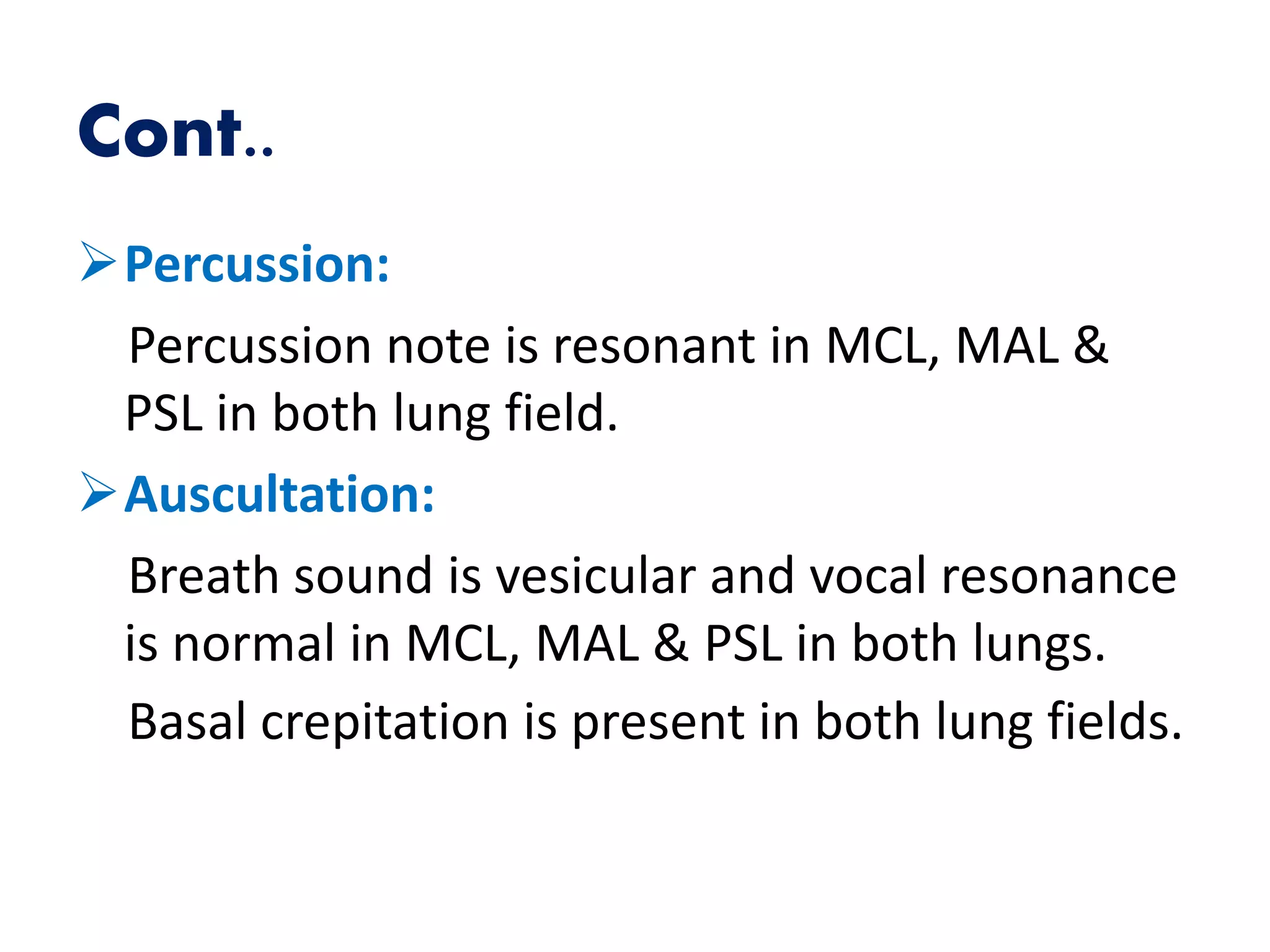
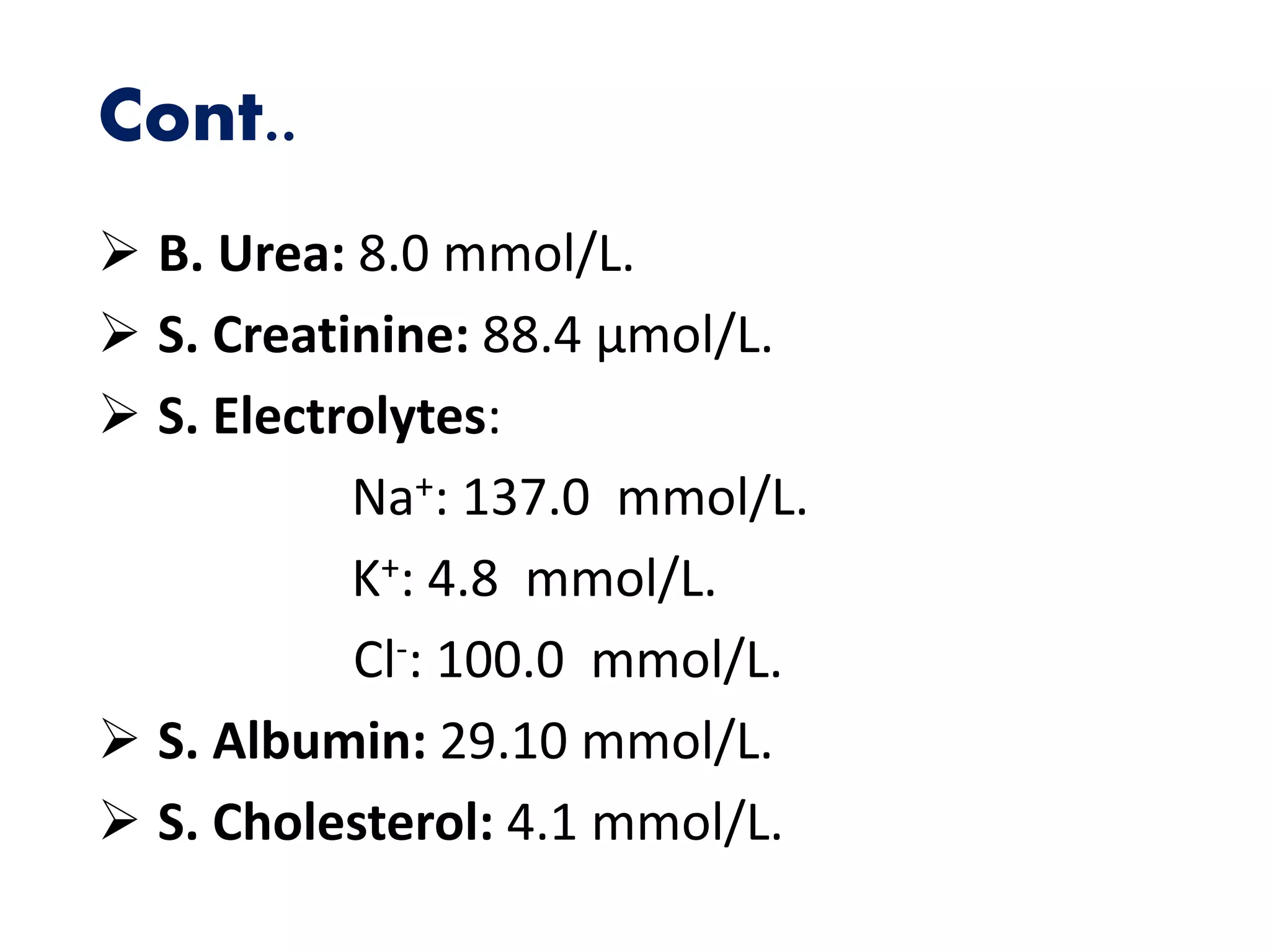
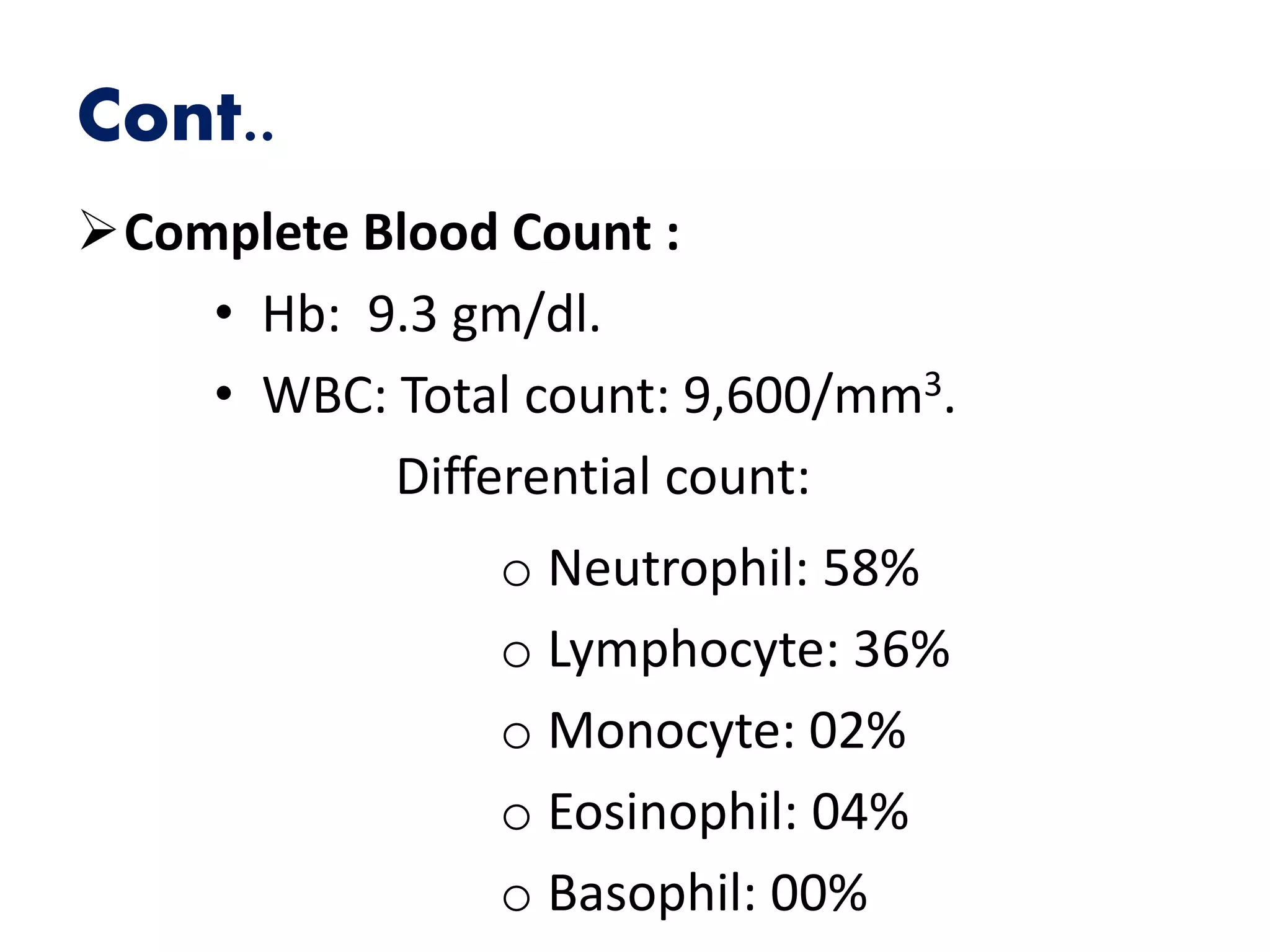
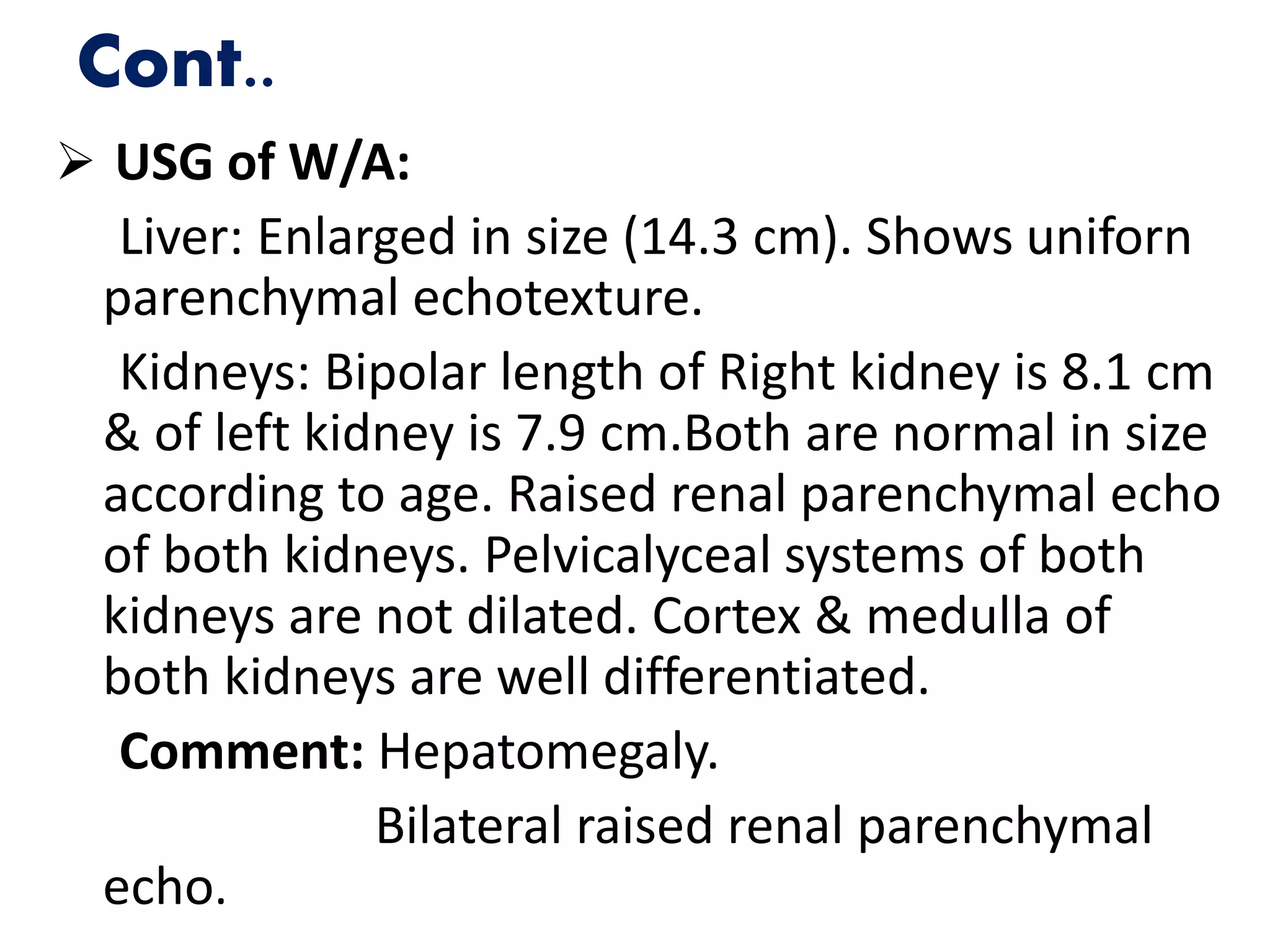
This document summarizes the medical case of a 7-year old boy named Arif who presented with facial swelling for 10 days, passing small amounts of reddish urine for 7 days, and respiratory distress for 1 day. On examination, he was found to have puffy face, ankle edema, tachycardia, and hepatomegaly. Laboratory tests showed hematuria, proteinuria, and low serum albumin. Ultrasound found hepatomegaly and increased renal parenchymal echoes bilaterally. He was diagnosed with acute post-streptococcal glomerulonephritis with heart failure and treated supportively with diuretics, antibiotics, and blood pressure control, showing improvement over his hospital stay