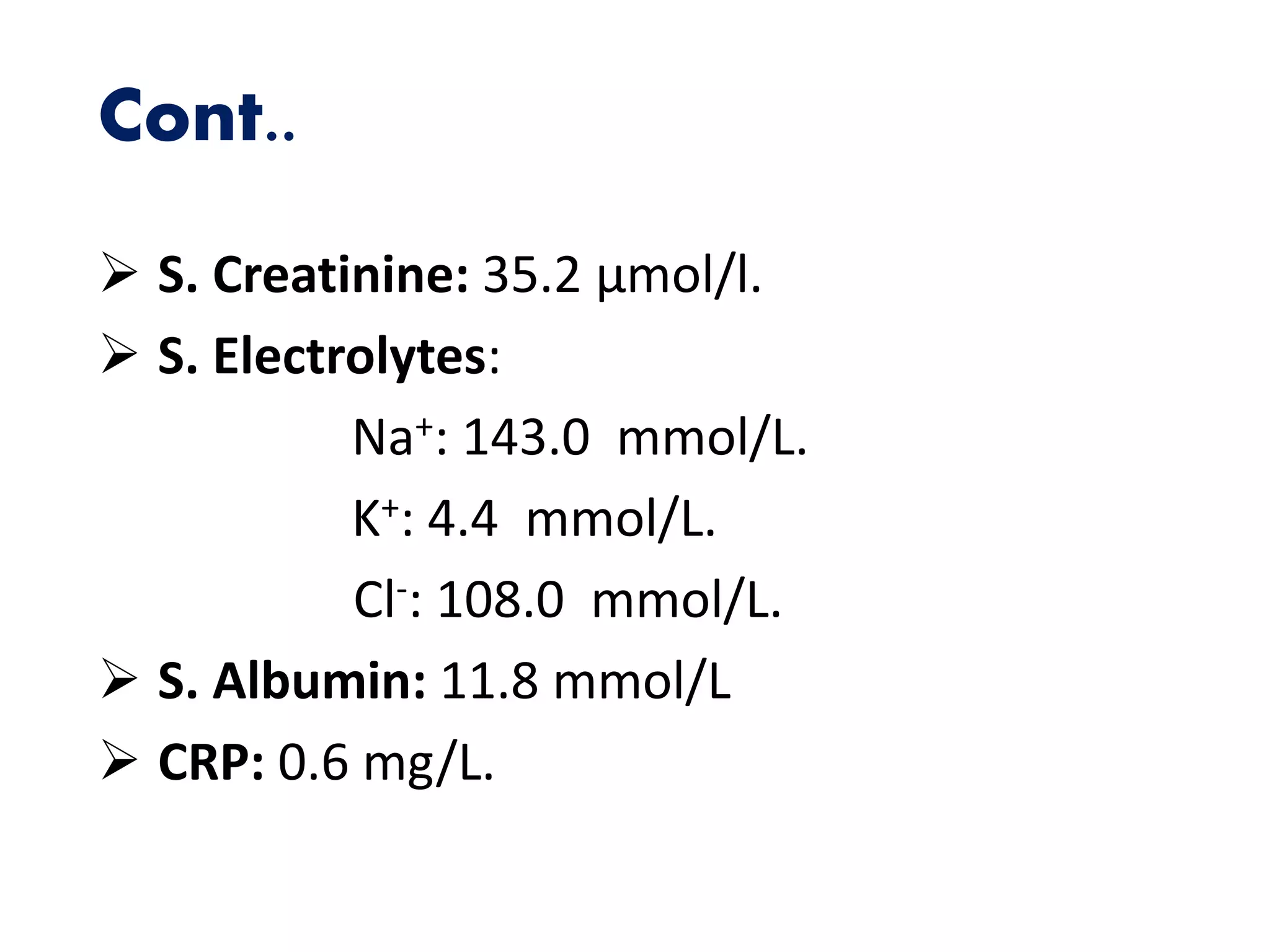
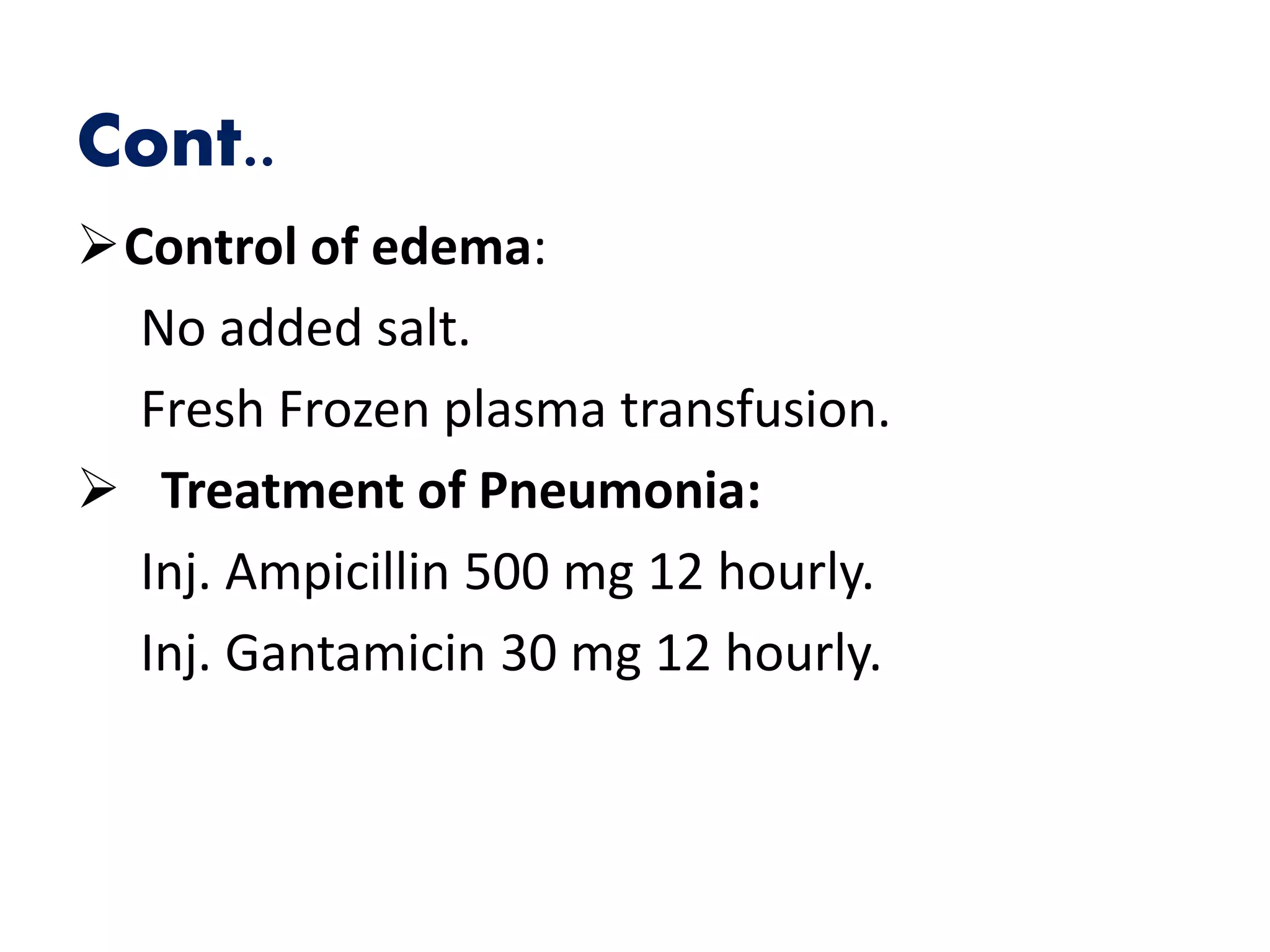
This document summarizes a medical case report for a 3 year 8 month old female patient presenting with proteinuria, oliguria, facial puffiness, and cough for several days. She has a history of similar episodes treated previously with oral prednisolone. On examination, she is found to be edematous with a puffy face and highly positive urine albumin. Labs show normal kidney function and electrolytes. A diagnosis of infrequent relapse nephrotic syndrome with bronchopneumonia is made. Treatment includes a tapering course of oral prednisolone and antibiotics, with close monitoring during admission and follow up visits.