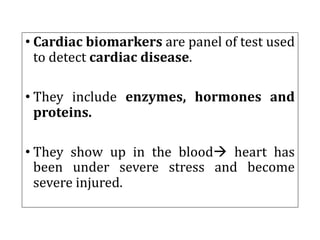
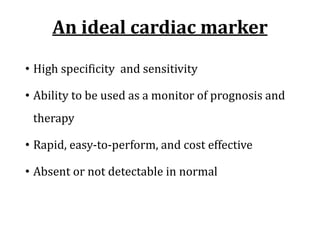
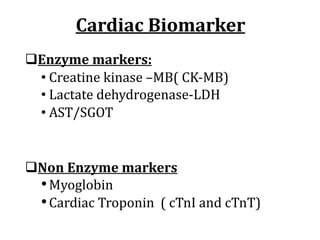
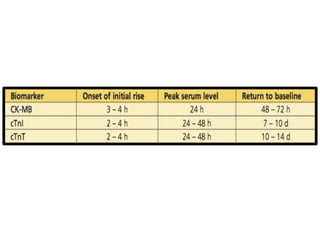
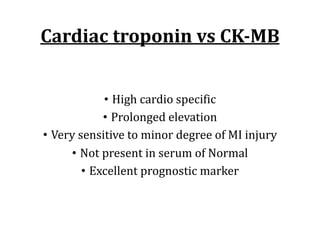
Cardiac markers are biochemical tests used to detect and diagnose cardiac conditions. Common markers include cardiac troponins, CK-MB, myoglobin, and BNP. Cardiac troponins are now the gold standard markers as they are highly specific to the heart and remain elevated for longer than other markers. Newer markers still under study include lipoprotein-associated phospholipase A2 and pregnancy-associated plasma protein A which may help identify unstable coronary plaque. A panel of multiple markers is often used for diagnosis and management of conditions like acute coronary syndrome, myocardial infarction, and congestive heart failure.
![• Acute coronary syndrome: A sudden cardiac
disorders with similar symptoms [ stable,
unstable angina and AMI]
• Angina: chest pain often associated with decreased
oxygen supply( ischemia) to heart muscle.
• Stable: increases with physical exercise or stress and
normalizes at rest
• Unstable: occurs while resting too. Sign for AMI](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-5-320.jpg)
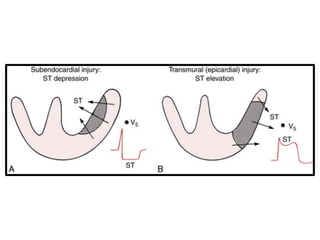
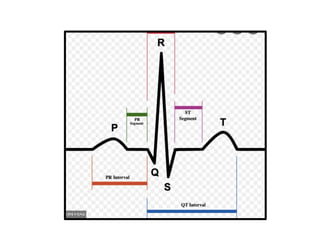
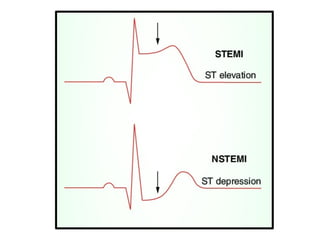
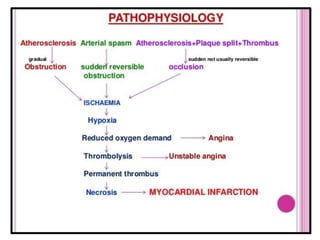
![• Acute myocardial infarction: myocardial
necrosis as a result of interruption of blood supply
to an area of cardiac muscle.
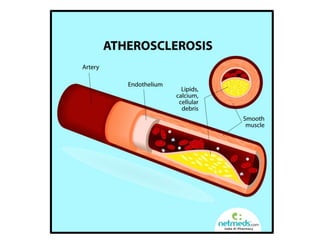
• Mainly caused by atherosclerosis of coronary
artery.
• Also called “heart attack”.
• TWO types STEMI and NSETMI [ based on ECG ]
• STEMI or transmural type: severe injury and ST
segment depression.
• NSETMI or subendocardial type: less severe and No ST
segment elevation. Develop pathologic Q waves](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-6-320.jpg)
![• Cardiac arrythmia: variation in the normal heart
beat or normal rhythm. Normal 60-100 bpm.
• Sinus rhythmà SA node
• Atrial rhythmà atria/atrial fibrillation
• Ventricular rhythmà ventricle
• < 60 bpm or bradycardia
• >100 bpm or tachycardia
• Infective Heart Disease : most common heart
disease caused by infection are:
• rheumatic heart disease[sore throat], infective
endocarditis[brushing], and pericarditis.](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-11-320.jpg)
![Other new/novel markers
[ more study ]
• Glycogen phosphorylase B
• Ischemia modified albumin (IMA)
• Heart type fatty acid binding protein
• Pregnancy-Associated Plasma Protein A
• Lipoprotein-Associated Phospholipase A2
• hsCRP
• Homocysteine level](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-18-320.jpg)
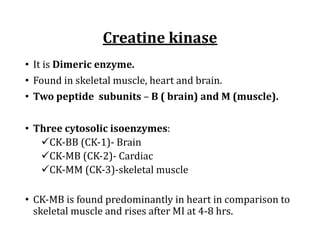
![• CK-MM is present in large amount in skeletal muscle
and also in Cardiac muscle [approx. 80%].
• CK-BB is predominantly present in brain and doesn’t
come into blood unless BBB is damaged.
• Although helpful in diagnosis MI at early stage, less
useful for confirmation in late stage [ normalizes by 3
days].
CK-MM CK-MB
• Skeletal muscle 95-98% Approx. 2-5%
• Cardiac muscle 80-90% 10-20%](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-22-320.jpg)
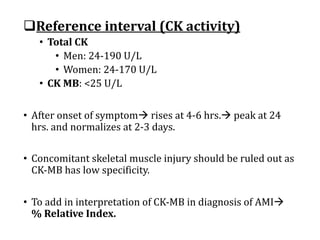
![q Percentage relative index (%RI)
%RI = (CK-MB mass/↑ed total CK ) X 100%
Ratio
• < 3.0 = skeletal muscle injury
• >5.0= indicative of AMI
• 3-5= gray zone [ neither ‘black’ nor ‘white’à still care]
q CK-MB mass is more good indicator than CK-MB activity.](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-25-320.jpg)
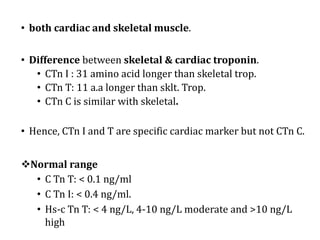
![• Troponin complex is present in the thin filament
of muscle à muscle contraction
• 3 types
• Troponin-C[ binds calcium]
• Troponin-I[ inhibitory unità binds to actin]
• Troponin-T[ binds with tropomyosin]
Cardiac troponin](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-27-320.jpg)
![CTn I vs CTn T
Specific to heart muscle
↓
Initially both were treated equal
↓
By time, False positive in ESRD patient [ CTn T]
↓
CTn t Antibody cross reacts with 0.5-2 % with skeletal
muscle Troponin too.
↓
So, CTnI is used more.](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-33-320.jpg)
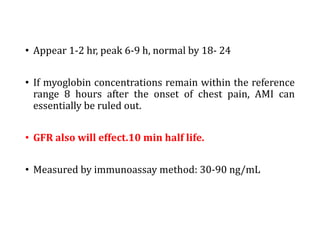
![Myoglobin
• is an oxygen-binding heme protein that is present in both
cardiac and skeletal muscle.
• lacks specificity
• its clinical usefulness à early release from damaged cardiac
or skeletal muscleà Earliest marker.
• Rapid fall [ than CK-MB and troponin]àRapidly cleared by
kidneyà Again increases in Re-ATTACK.](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-34-320.jpg)
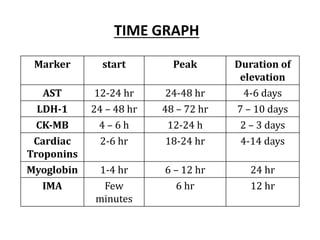
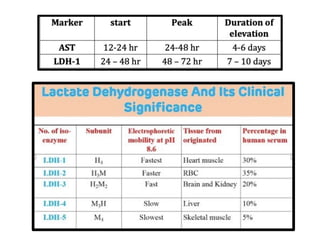
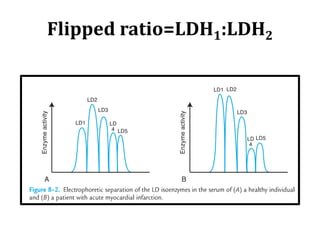
![Biomarkers of older days
qAspartate aminotransferase (AST)
• 12-24 hr ,24-48 hr, 4-6 days.
• Older days
• Not early detection, not specific [ many disease]
• Not used these days
qLactate dehydrogenase [ many isoenzyme]
• Used in older days
• Highly non specific [ many isoenzymes ]
• Rises late but stays for 7-10 days
• Not used these days](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-36-320.jpg)
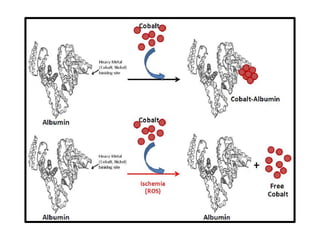
![Ischemia modified albumin
[IMA] [52 to 116 kU/L]](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-39-320.jpg)
![Ischemia modified albumin[IMA]
• It measures changesà occur in albumin in ischemic
condition [ Lack of oxygen]
• Under Ischemia à free radical à confirmational change
albumin à alter its ability to bind transition metals, such as
cupper or cobalt.
• Starts with in few minutes, peak at 6 hr and normal at 12 hr.
• Done by Albumin cobalt binding test](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-40-320.jpg)
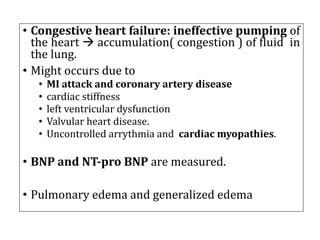
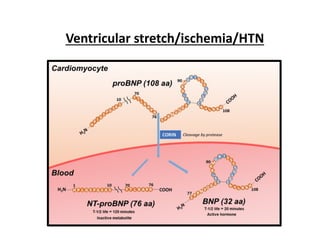
![Congestive heart failure
qNatriuretic peptide: hormone
• Atrial NP à produced by atrial myocytes
• Brain NP à Produced by ventricular myocytes [ isolated
from porcine brain tissue].
• C-type NPà unknown
• Clinically imp: BNP and NT pro BNP.
• Released from cardiac ventricles myocytes in response to
stretch.
CHF likely to occur
• BNP : >100 pg/ml
• NT pro-BNP: >400 pg/ml](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-42-320.jpg)
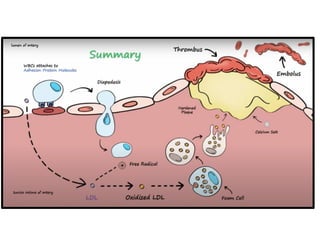
![Pregnancy-Associated Plasma
Protein A [PAPP-A]
• Is a metalloproteinase
• Major contributor for progression of
atherosclerosis à increases plaque formation
• High in unstable plaque in comparison of
stable plaque.
• Still not standardized assay and reference
interval](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-44-320.jpg)
![Lipoprotein-Associated Phospholipase
A2
• LP-PLA2, also known as platelet-activating factor acetyl-
hydrolase
• Synthesized by inflammatory cell [monocyte &
lymphocytes]
• Cleave ox. Lipid à induce lipid fragment
• Which is more atherogenicà Increases endothelial
adhesion.
• Marker for plaque instability.
• Researches has focused to see the role LP-PLA2 in
stroke.](https://image.slidesharecdn.com/cardiacmarkers-220311100558/85/Cardiac-markers-45-320.jpg)