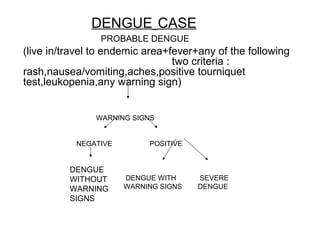
This document discusses dengue in children, including its epidemiology, etiology, pathogenesis, clinical manifestations, management, and differential diagnosis. Some key points:
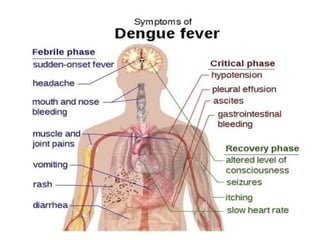
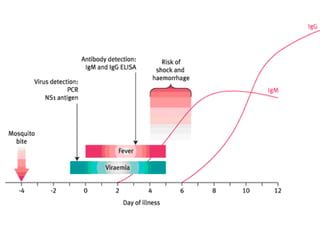
- Dengue is a mosquito-borne viral disease spread by Aedes mosquitoes and endemic in most parts of the world except Europe. It has four serotypes.
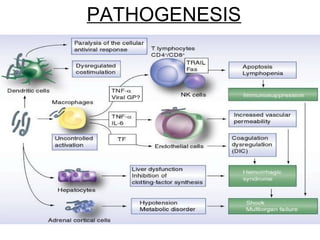
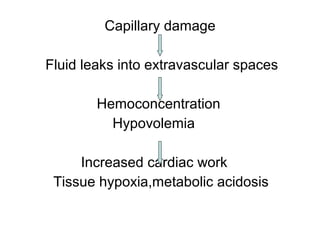
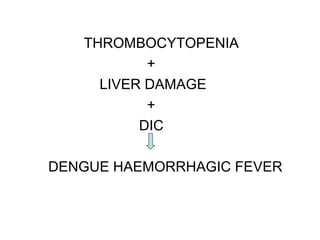
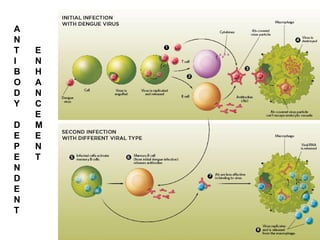
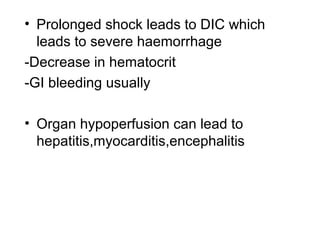
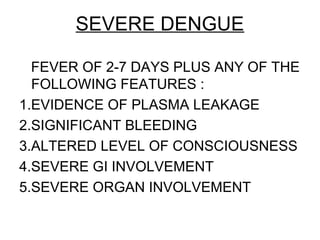
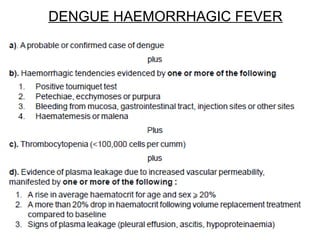
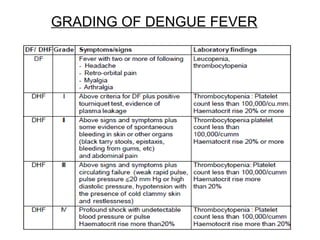
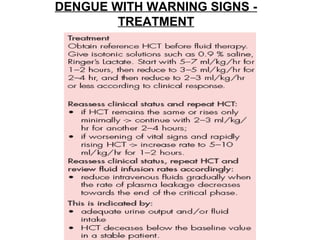
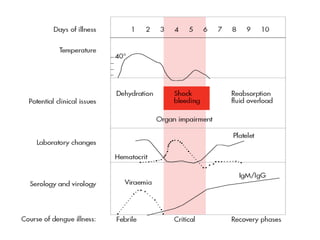
- The virus causes capillary damage and fluid leakage, which can lead to hypovolemia, shock, organ dysfunction, and hemorrhage in severe cases. Secondary infection with a new serotype increases risk.
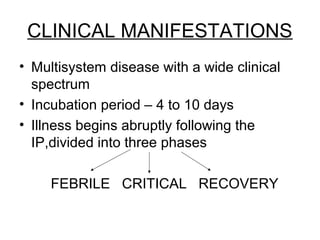
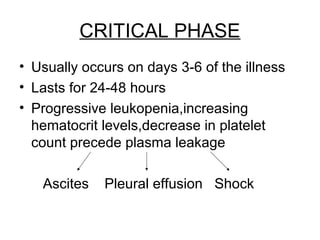
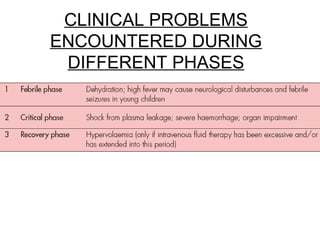
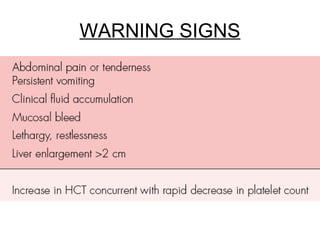
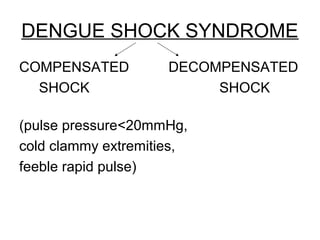
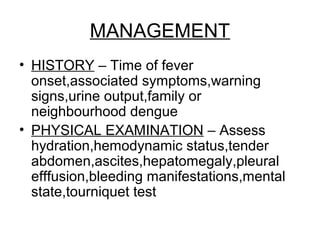
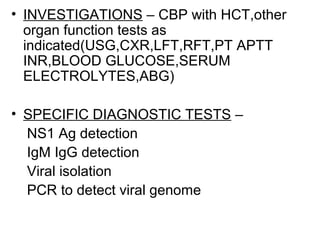
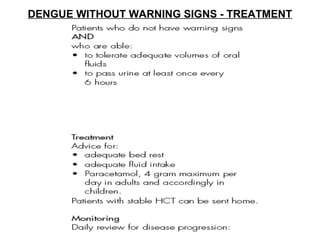
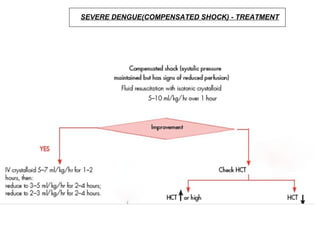
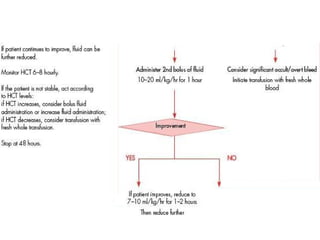
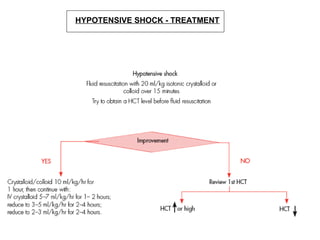
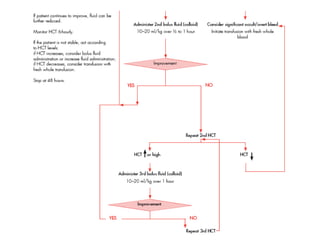
- Clinical phases include fever, critical, and recovery. Warning signs like abdominal pain, vomiting indicate risk of severe disease. Management involves fluid management, monitoring for shock