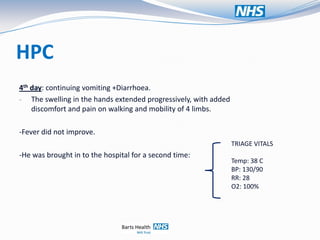
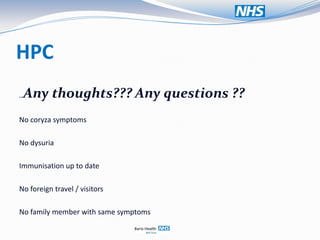
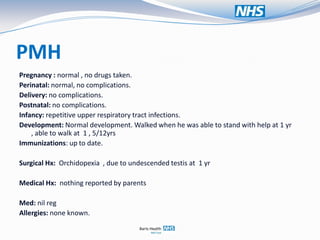
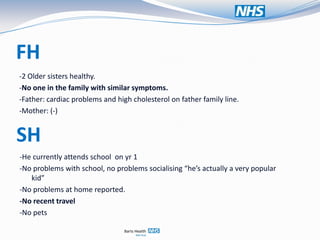
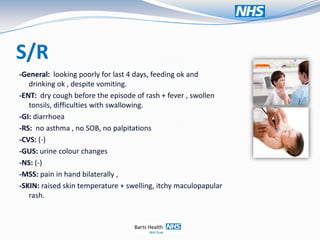
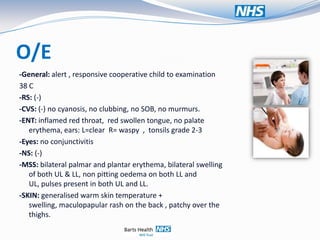
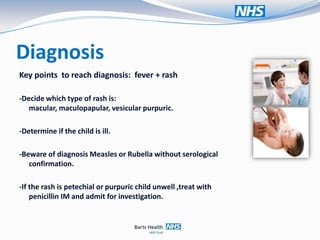
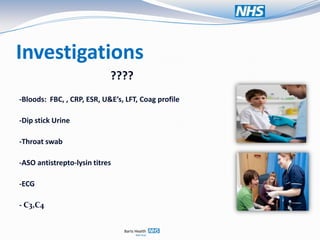
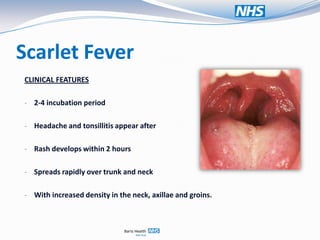
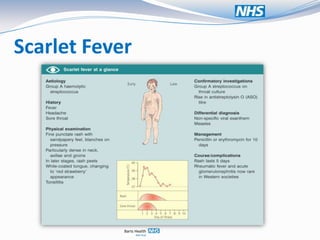
This document presents a case history for a 6-year-old boy, S.K., who presented with a rash and fever. Over 4 days, the rash spread and he developed swelling of the hands, vomiting, diarrhea, and worsening fever. Differential diagnoses included viral exanthems, scarlet fever, toxin-mediated rash, and Kawasaki disease. On examination, he had a maculopapular rash, swollen throat and tonsils, and swelling of the hands and lower limbs. Investigations and management for potential scarlet fever were discussed.