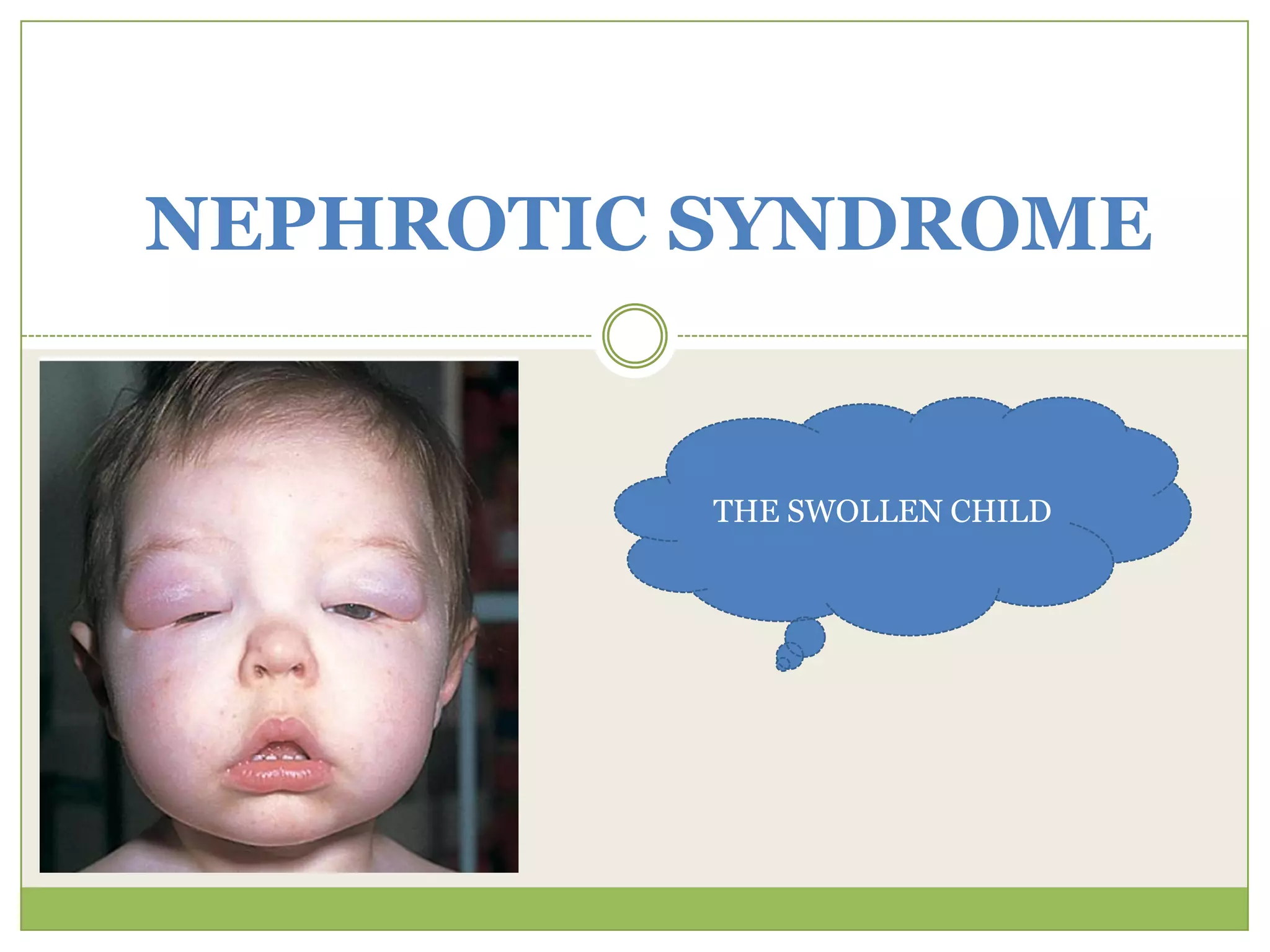
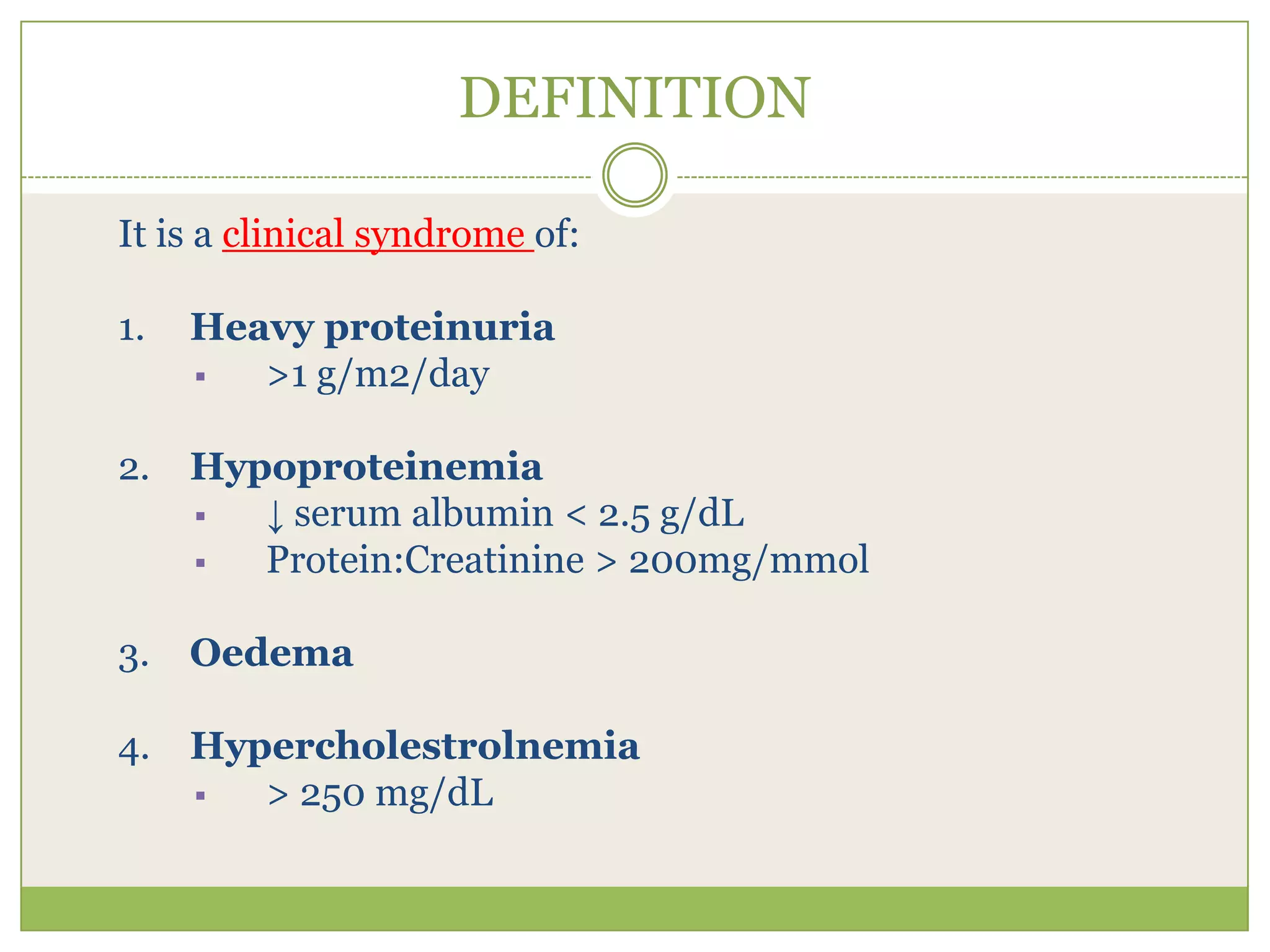
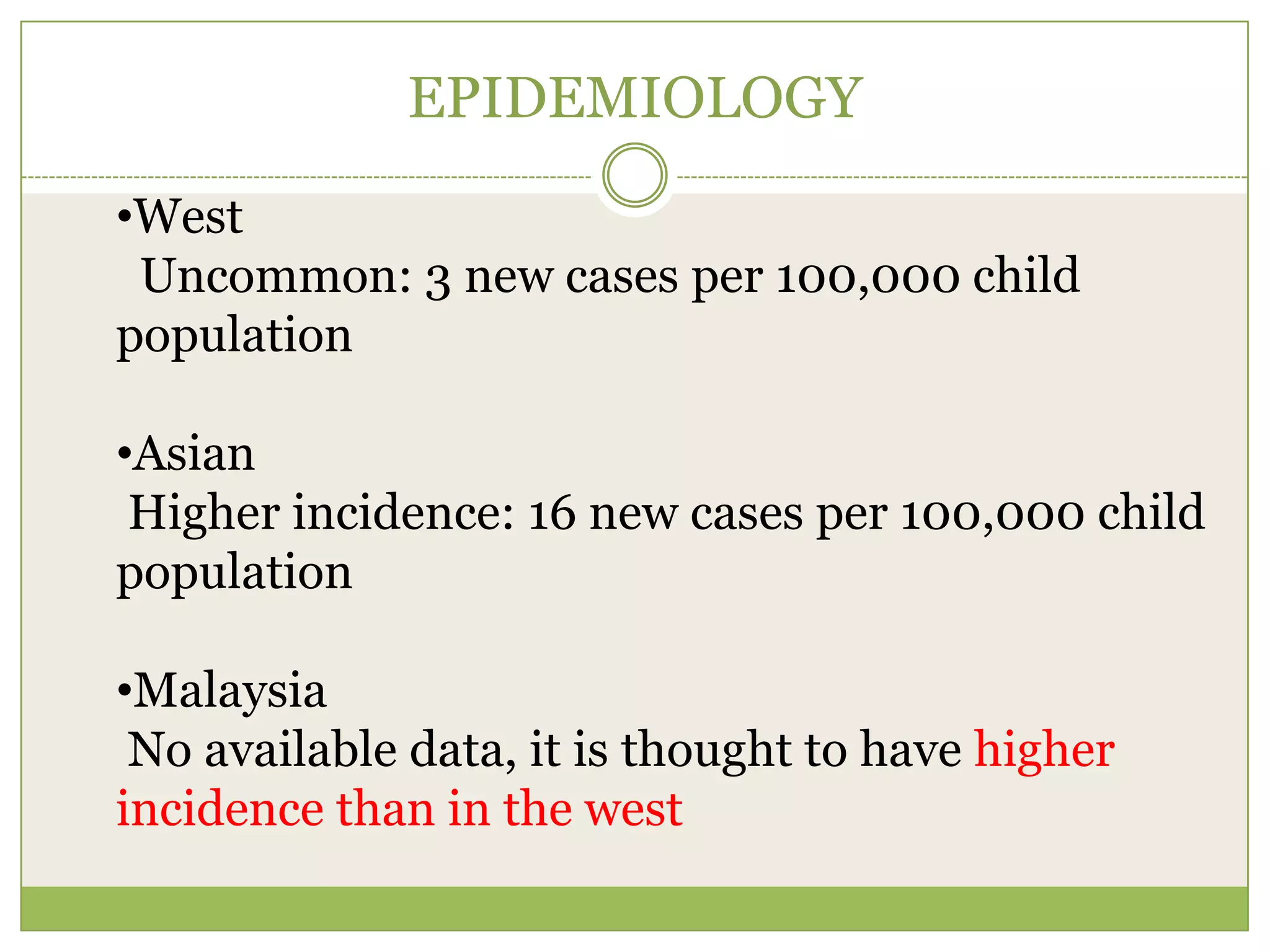
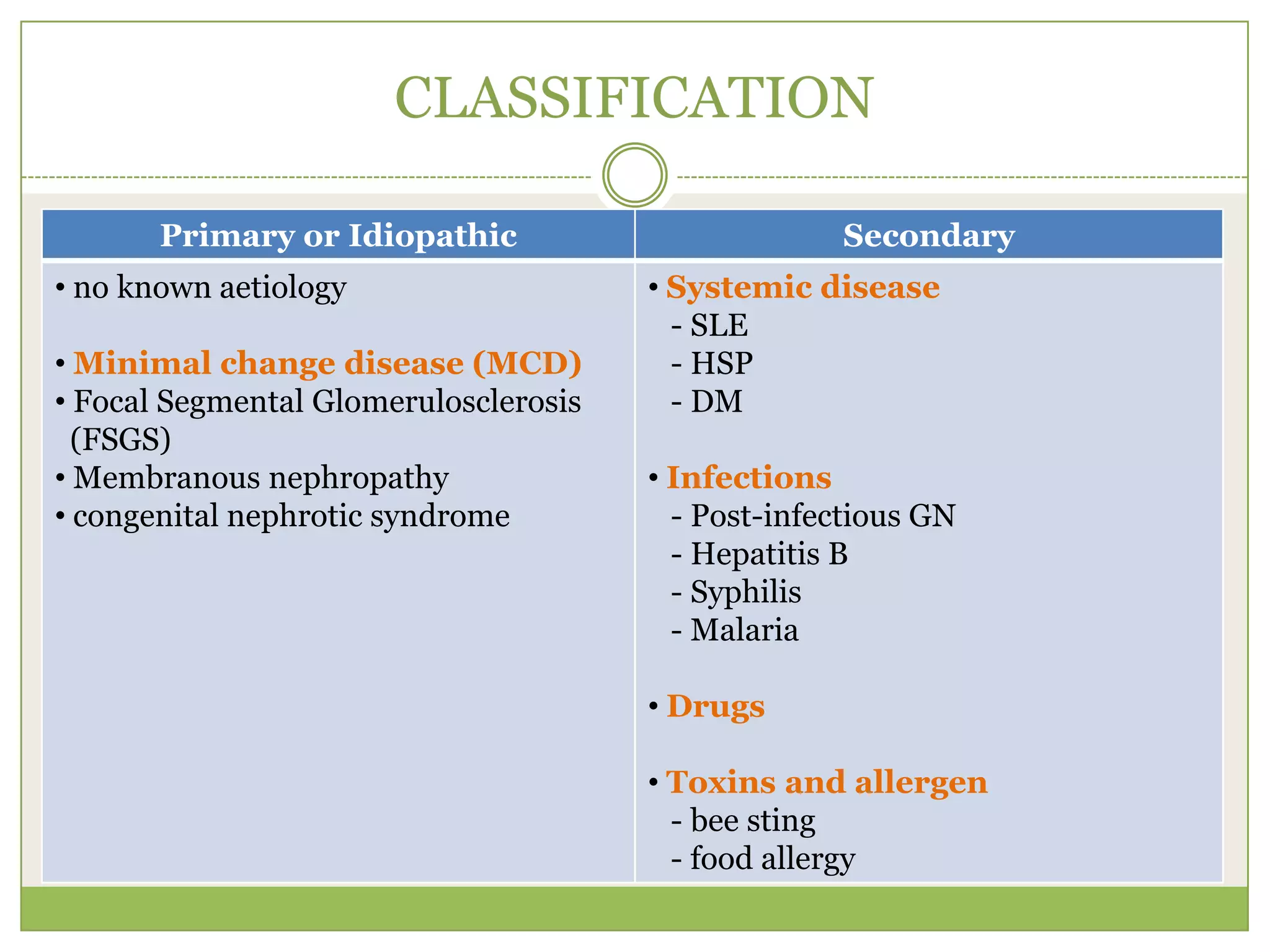
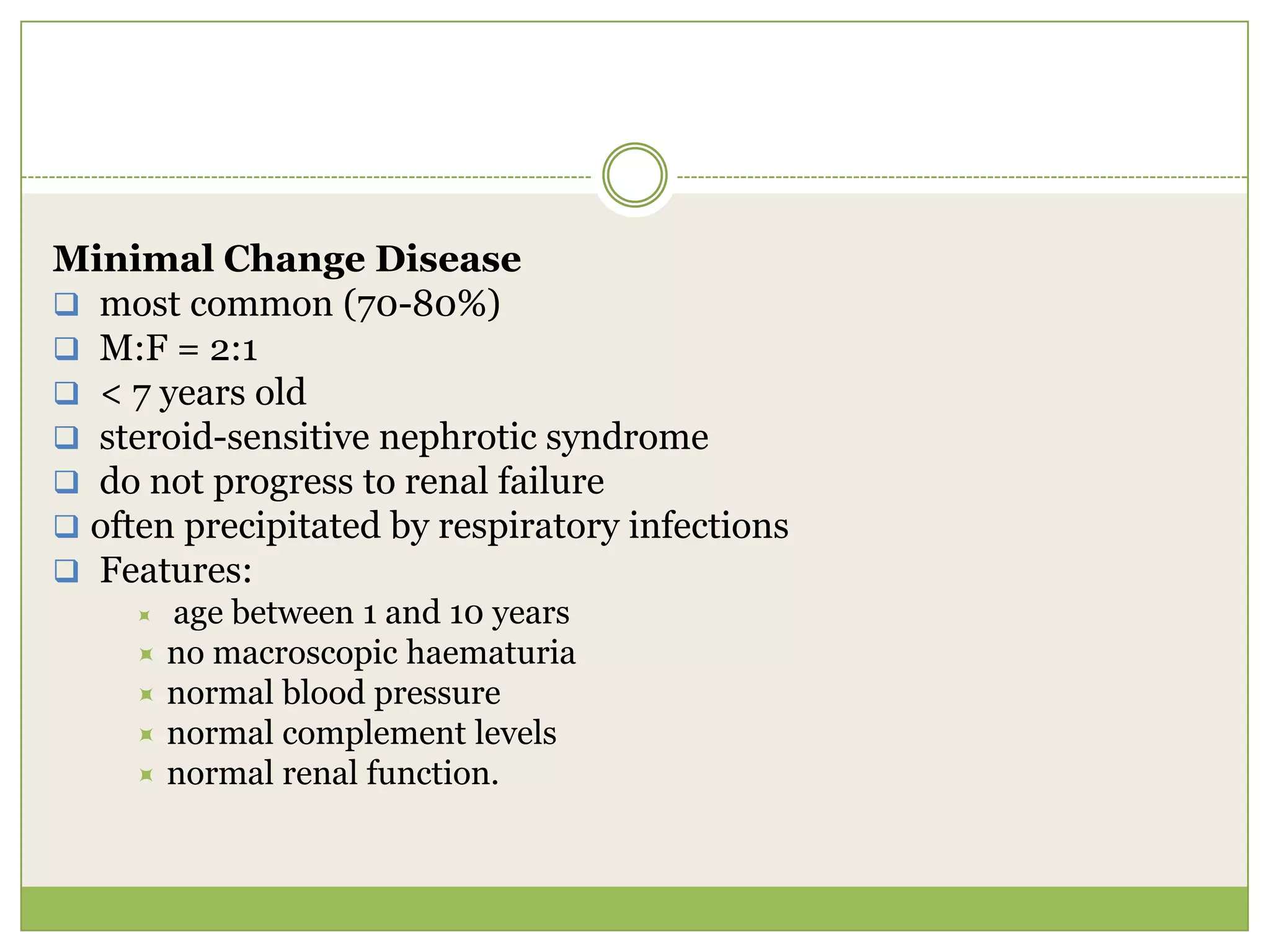
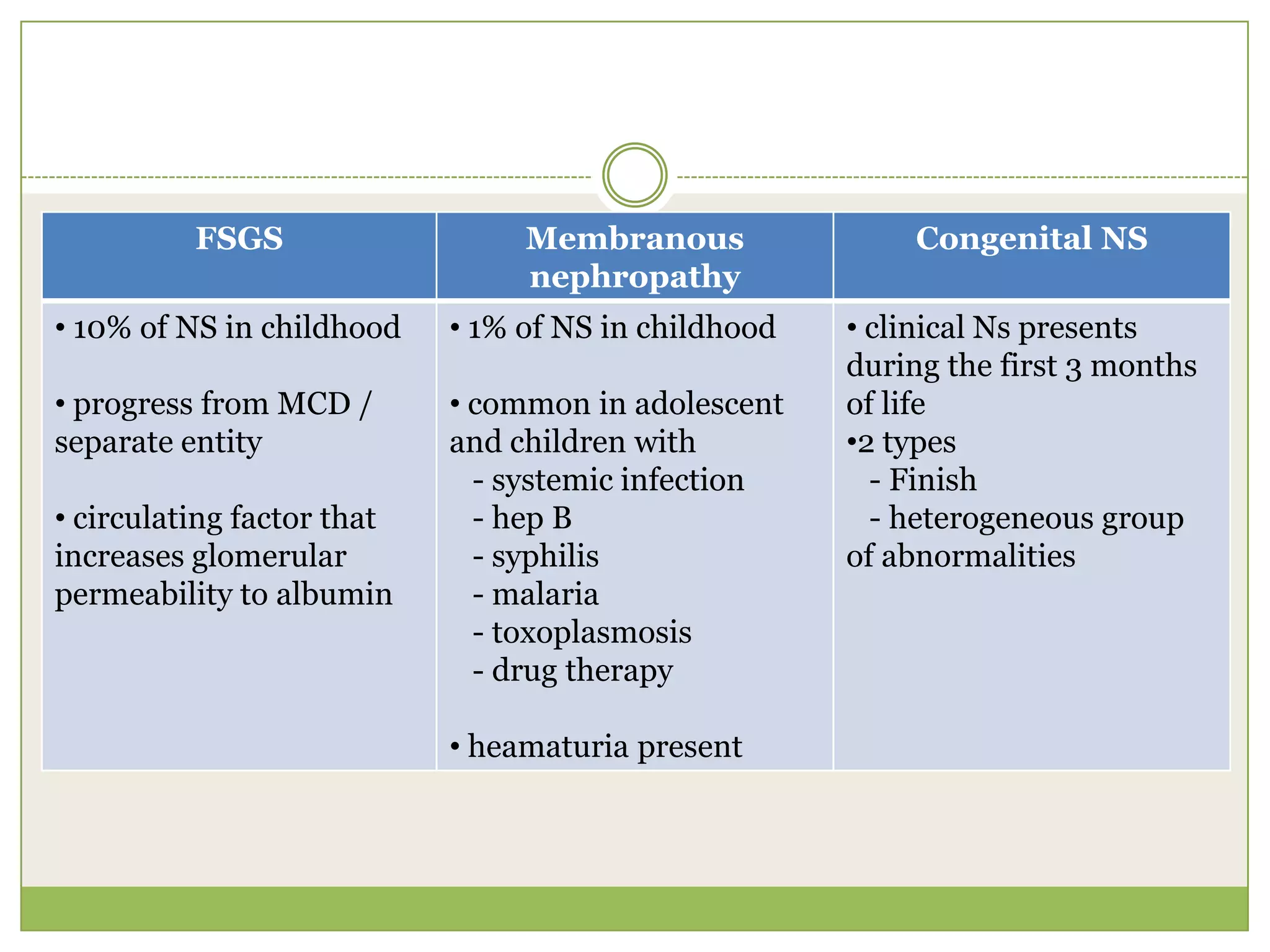
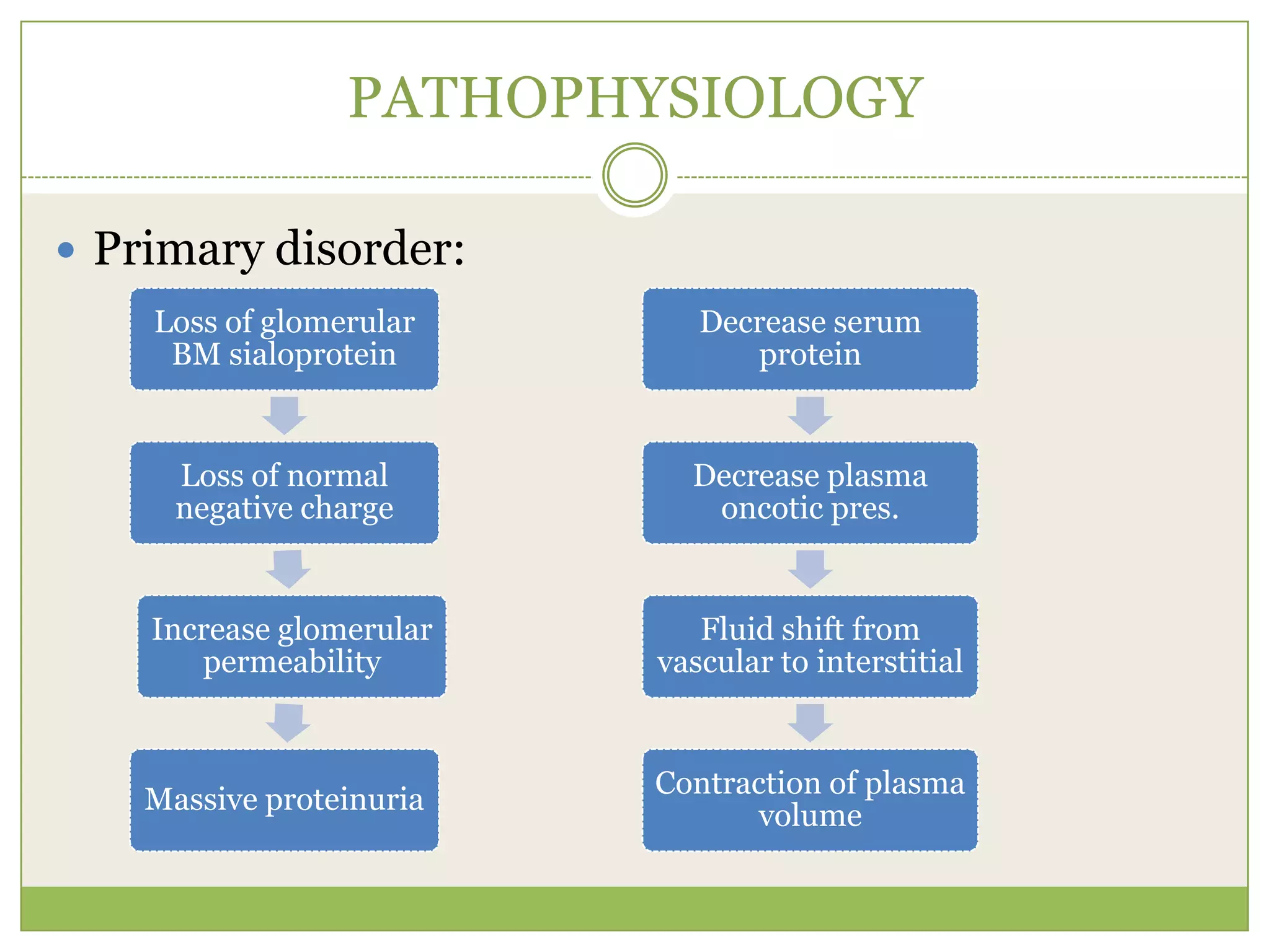
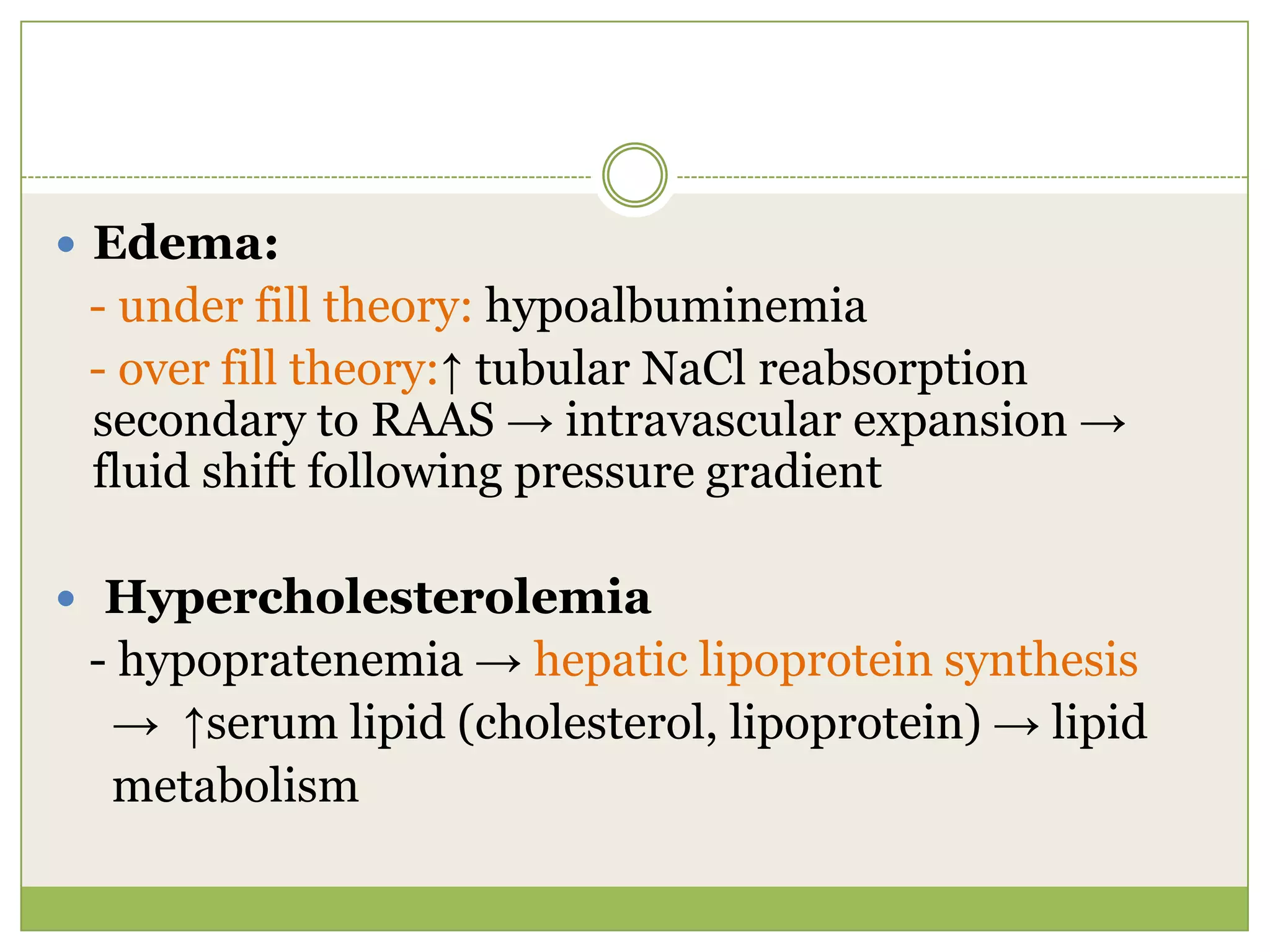
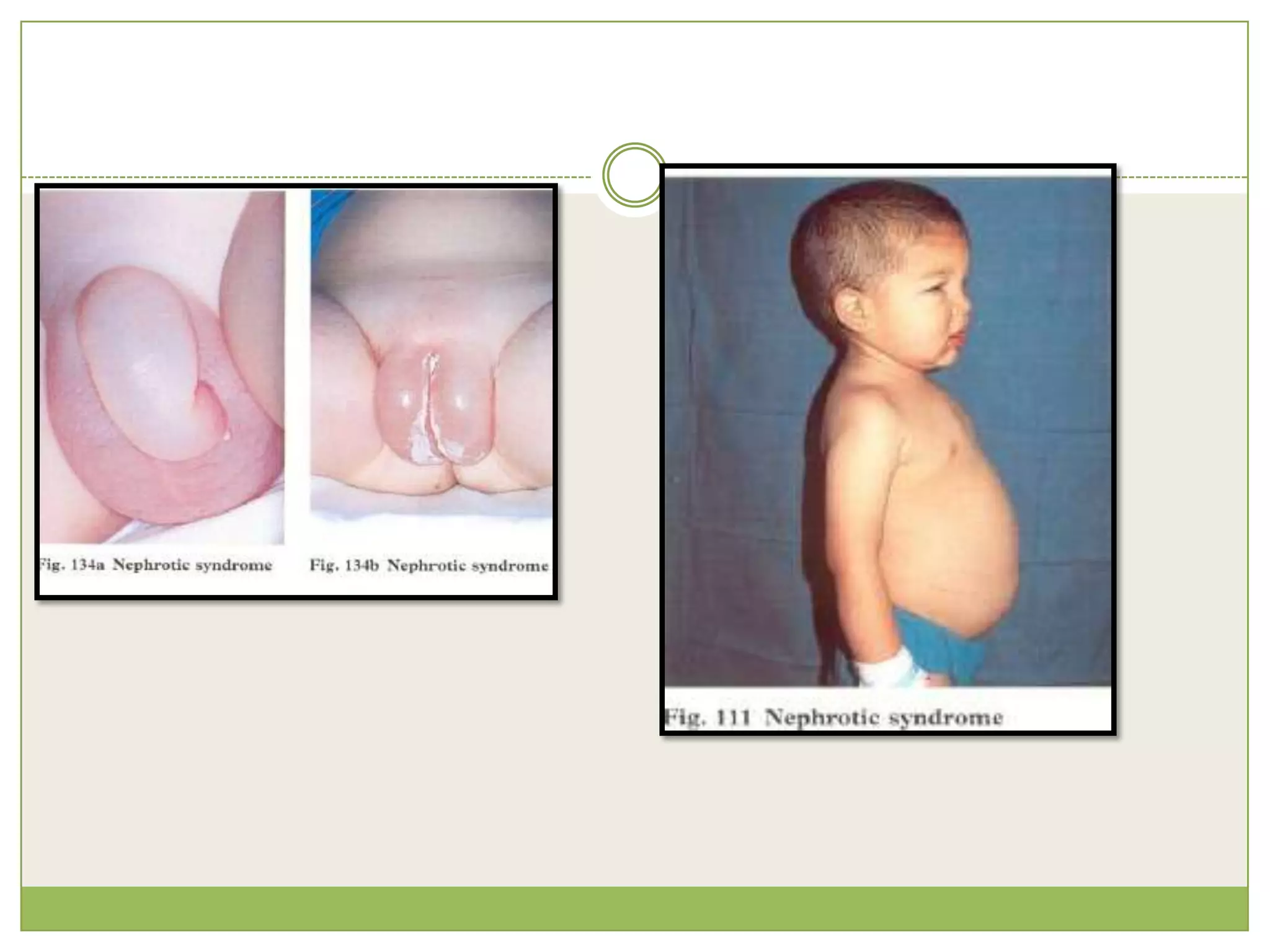
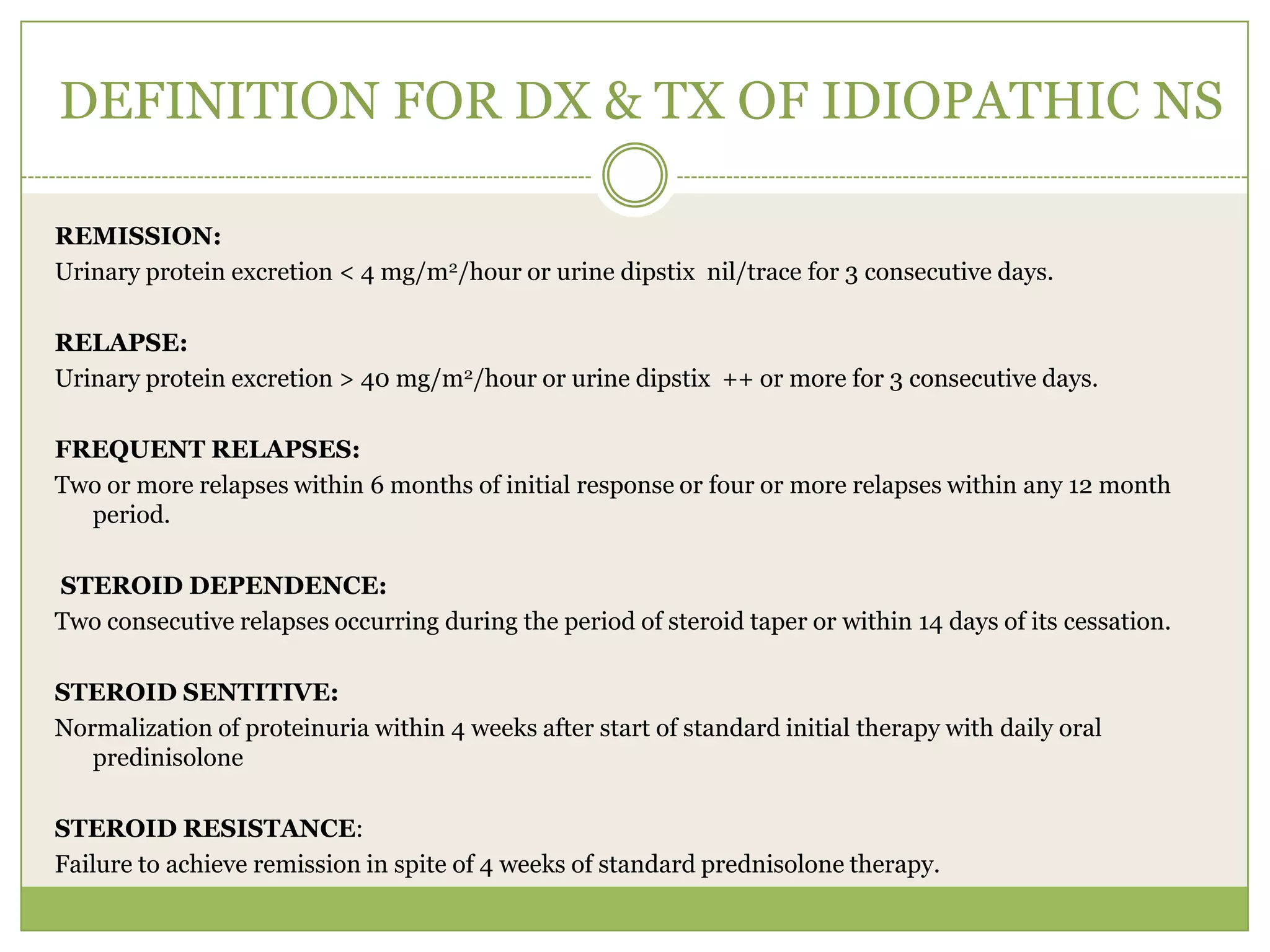
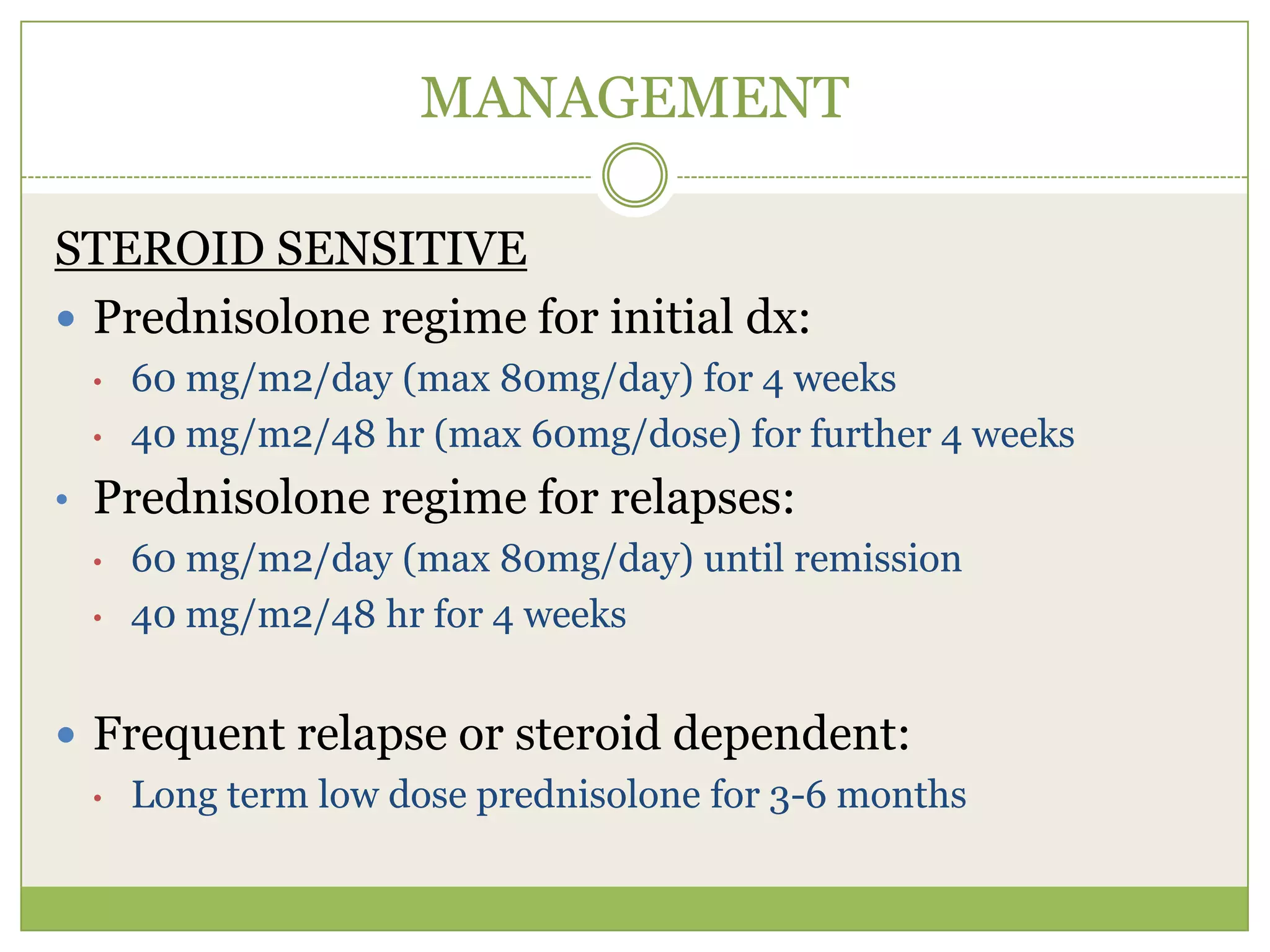
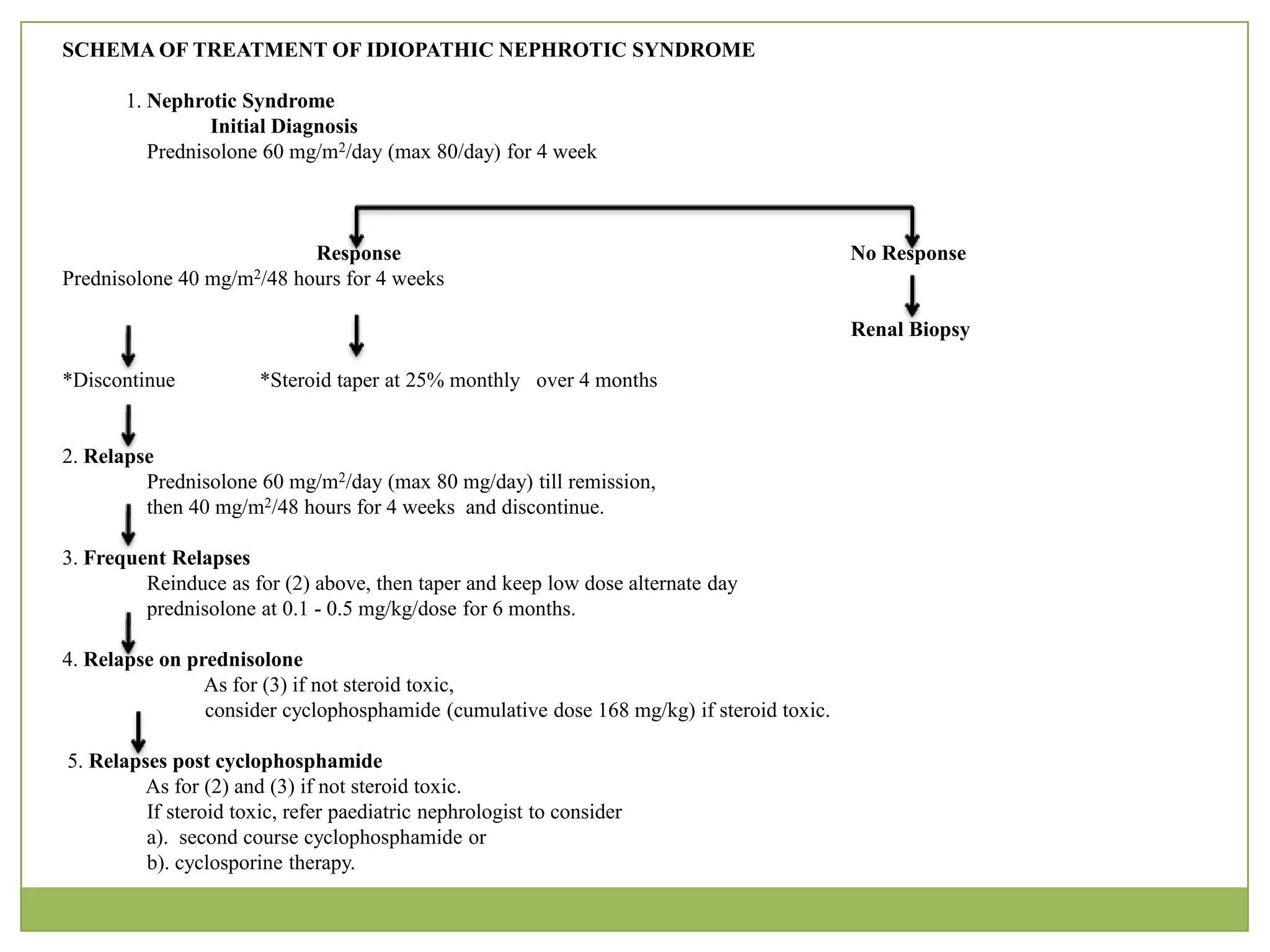
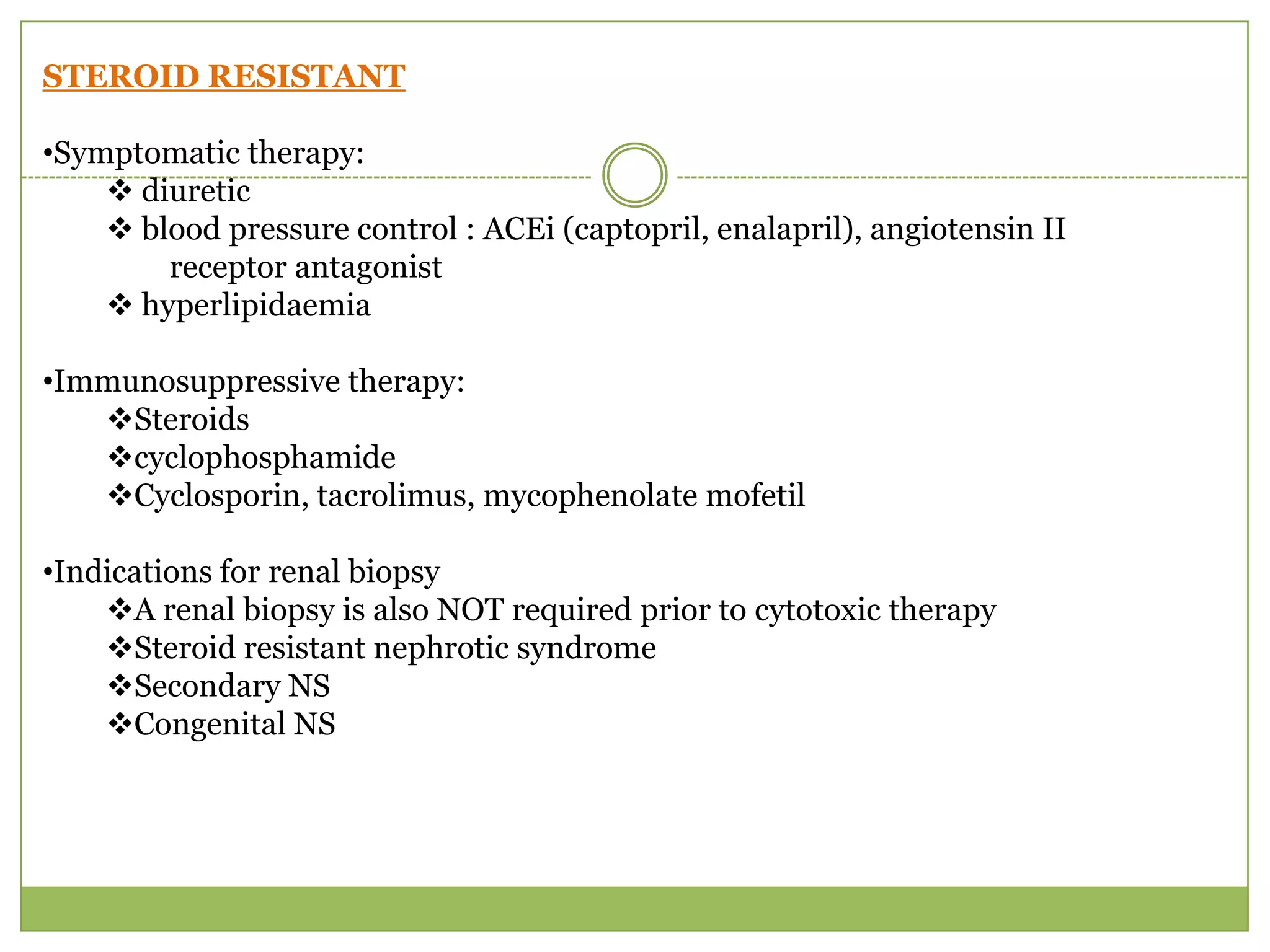
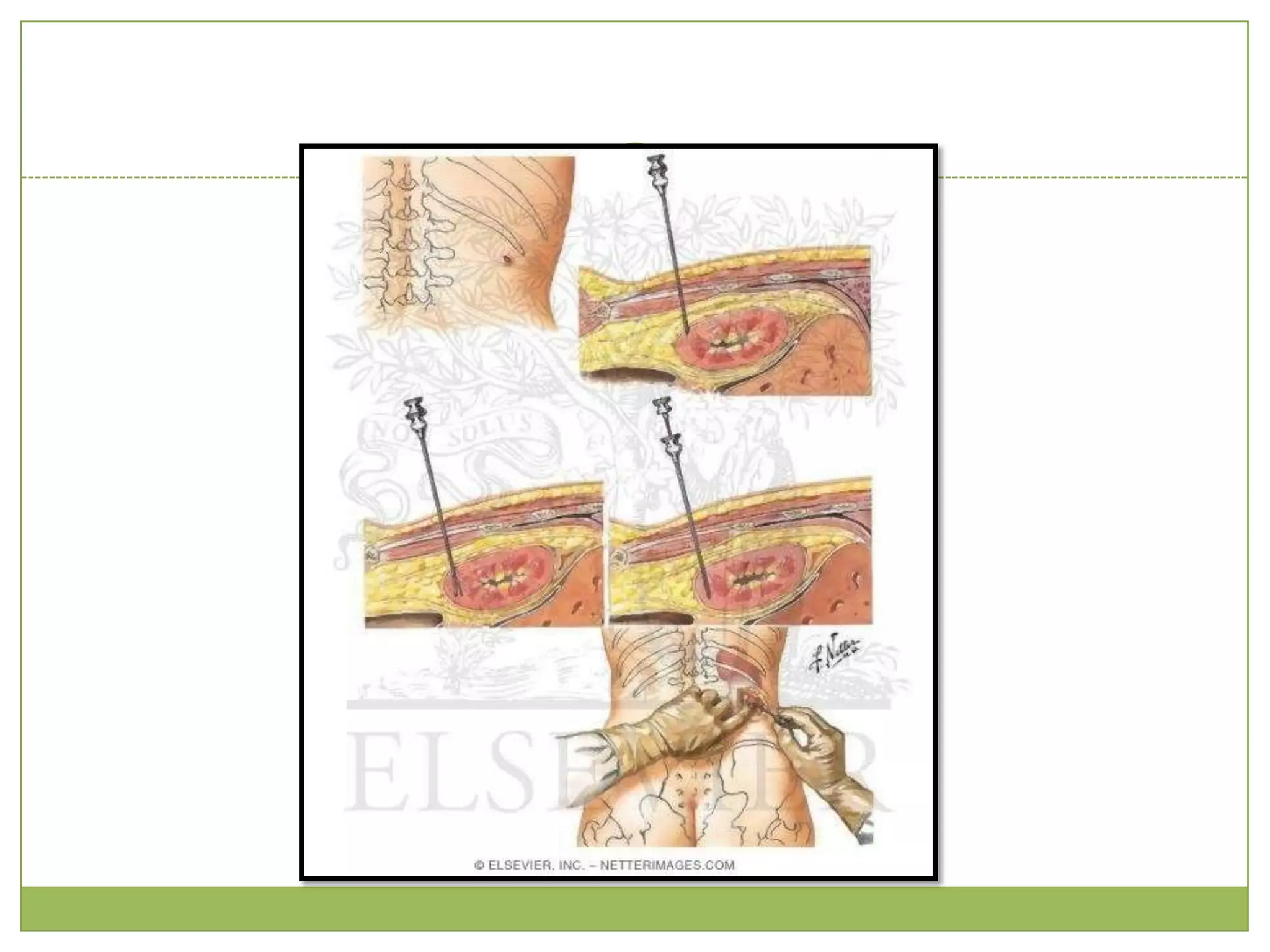
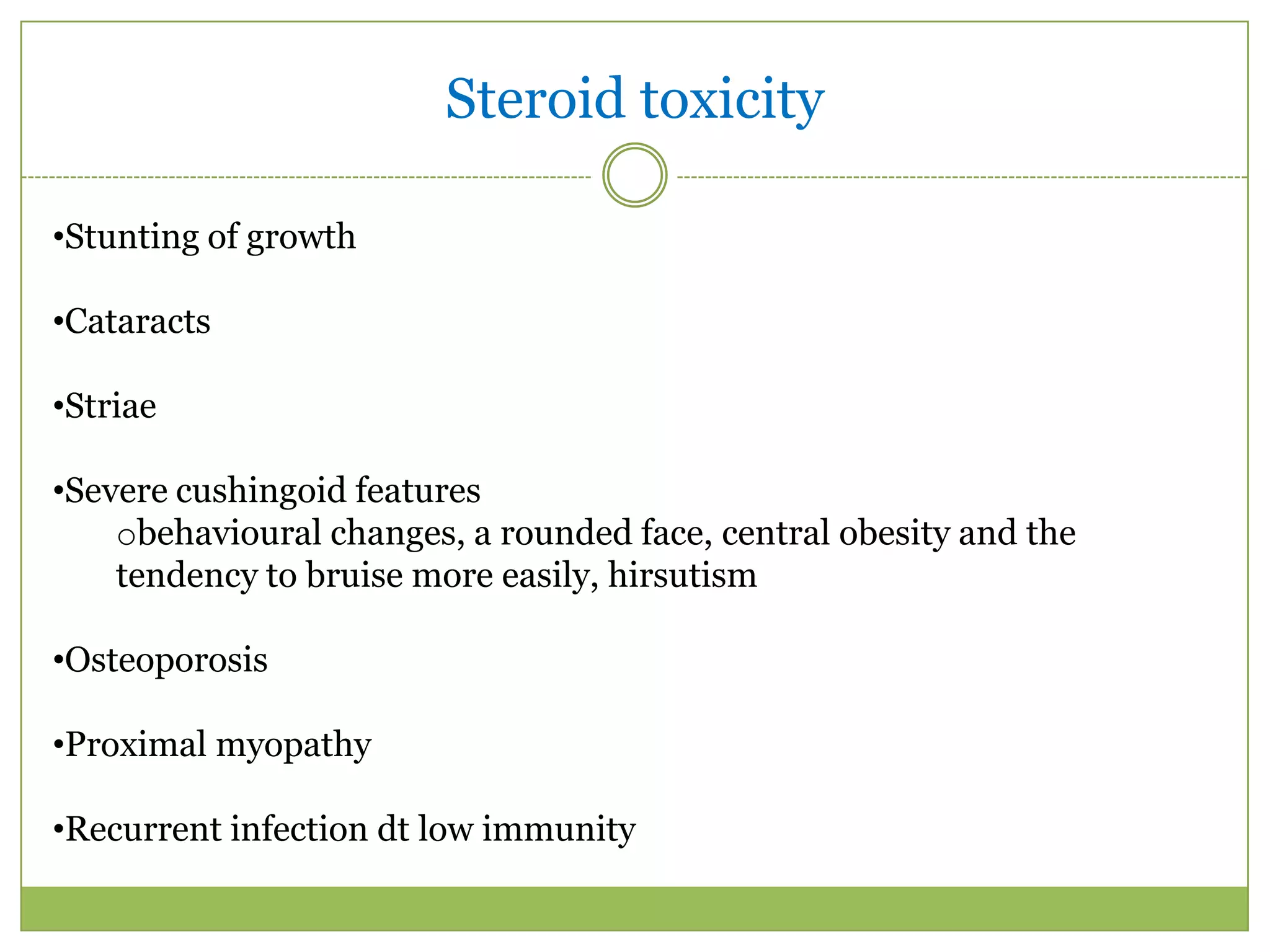
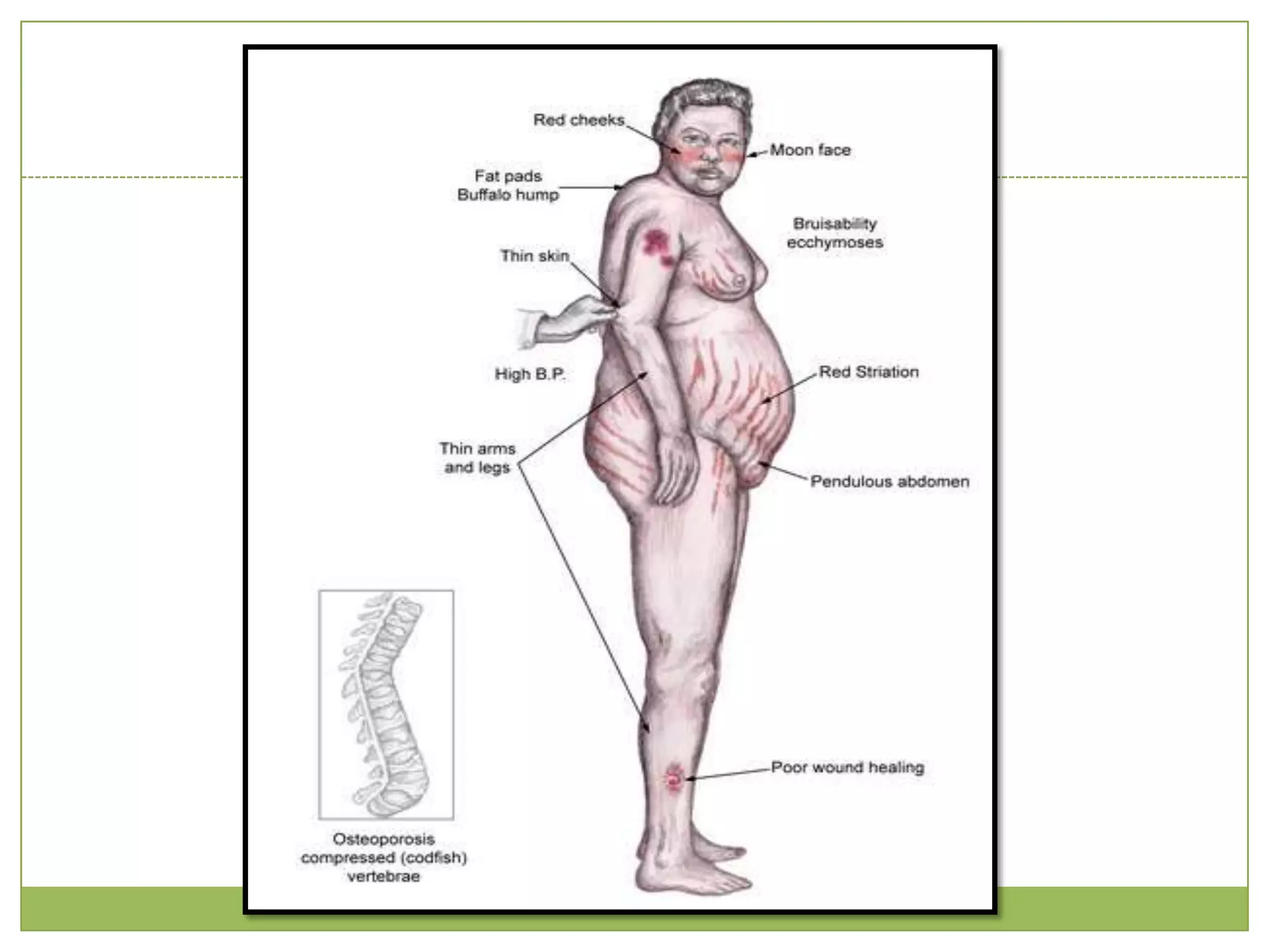
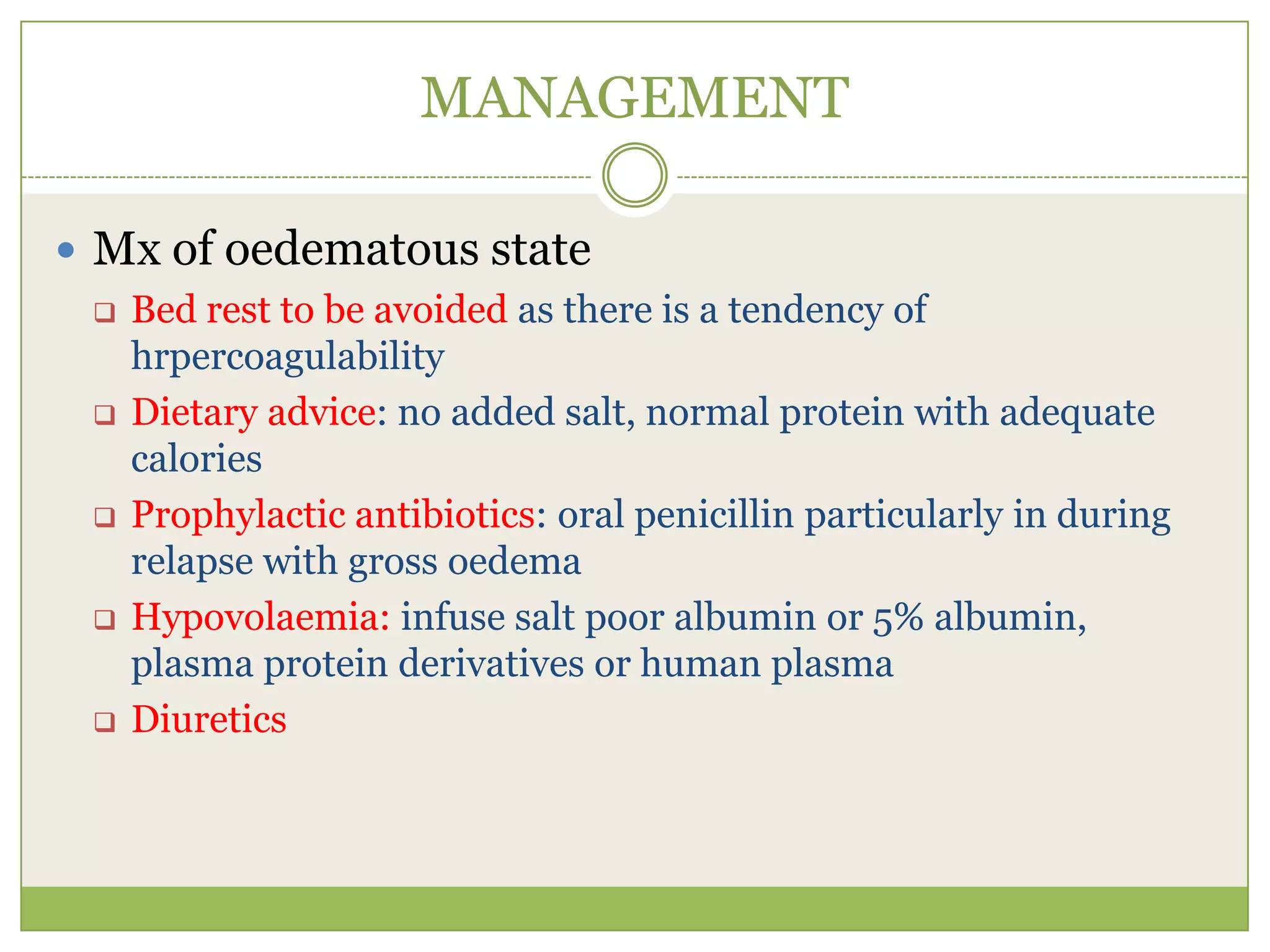
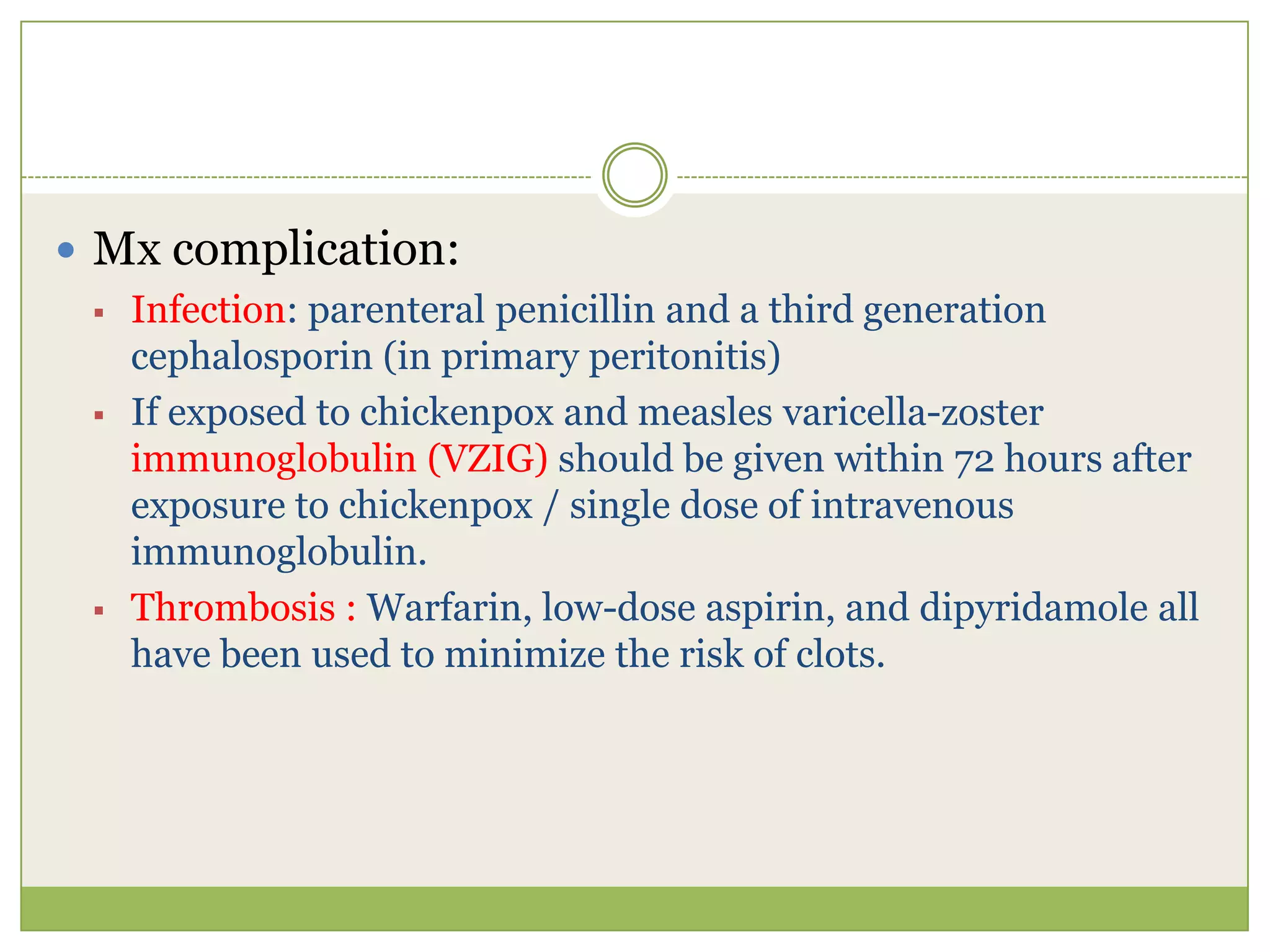
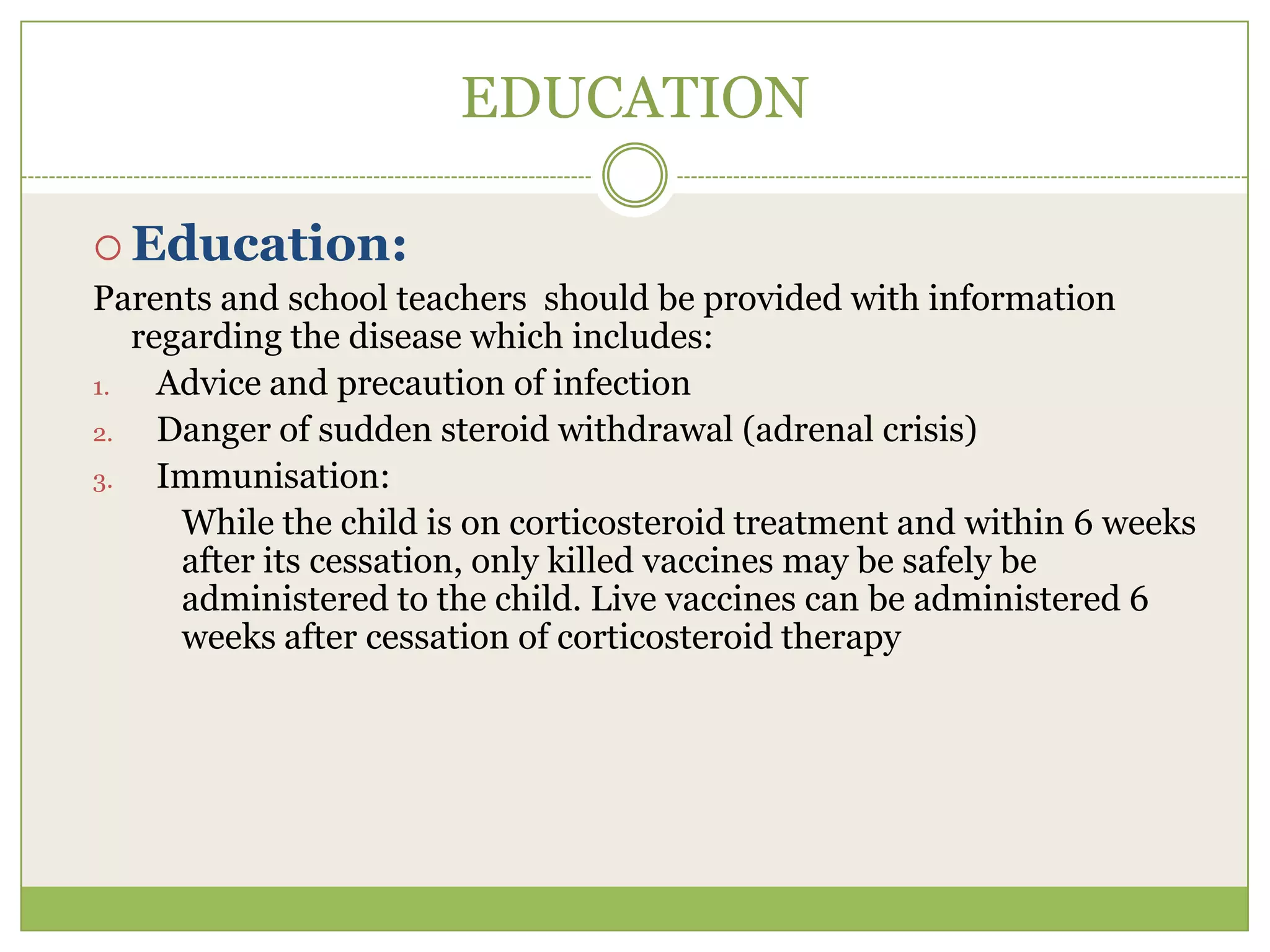
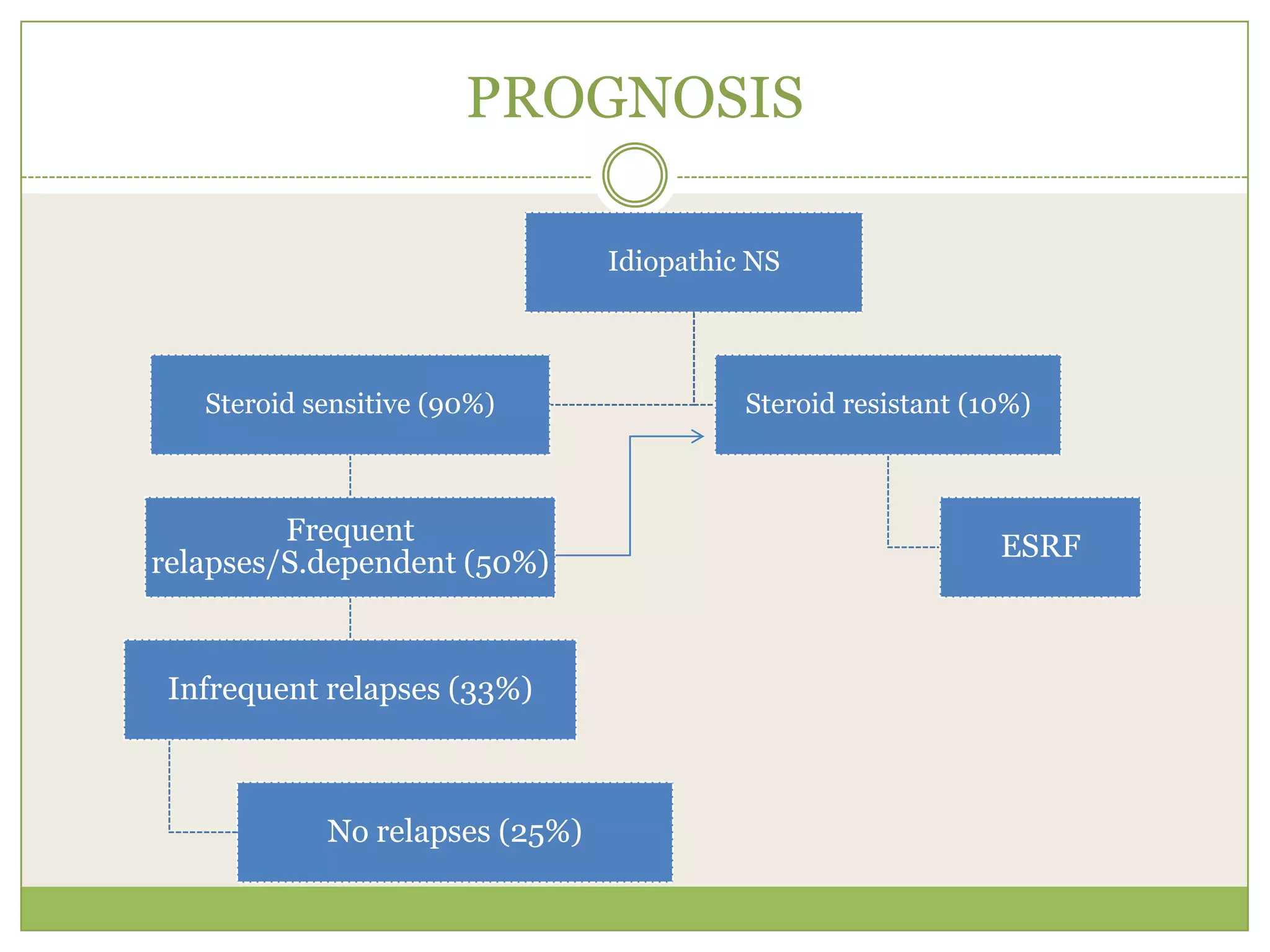
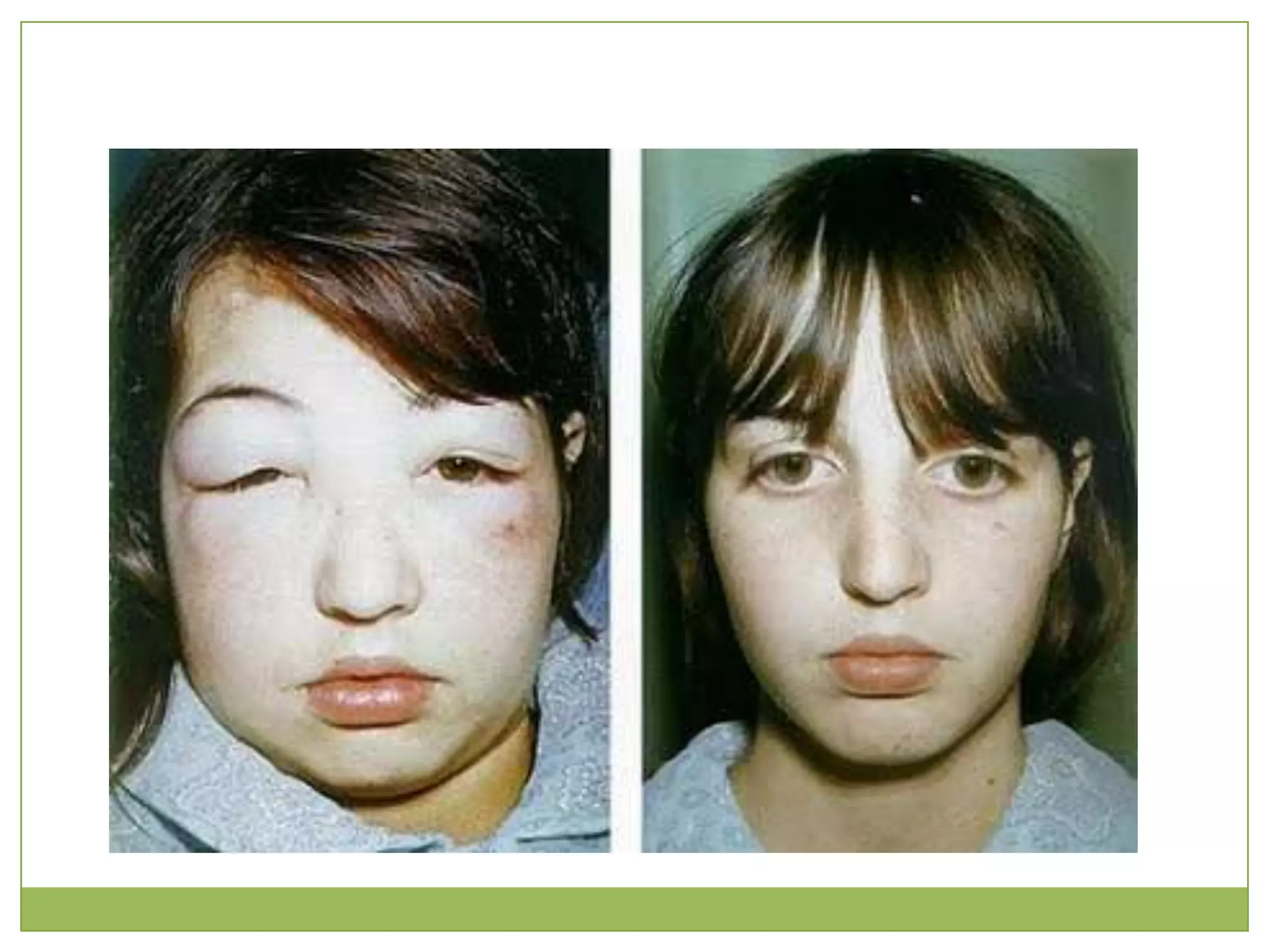
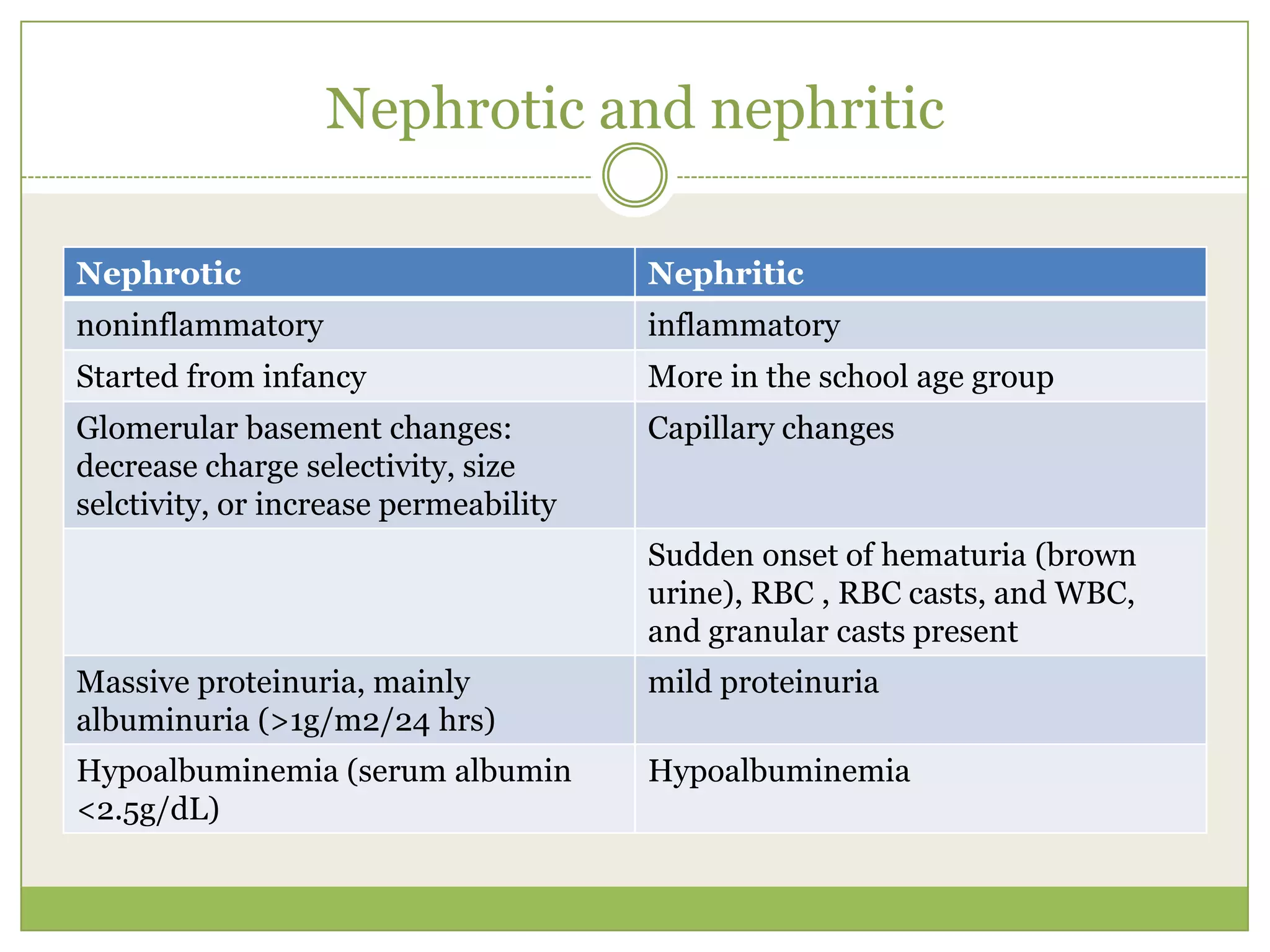
This document provides information on nephrotic syndrome, specifically defining it as a clinical syndrome characterized by heavy proteinuria, hypoproteinemia, edema, and hypercholesterolemia. It describes the epidemiology, classification, pathophysiology, clinical manifestations, investigations, diagnosis, management, and prognosis of nephrotic syndrome. The key points are that minimal change disease is the most common type, presenting with edema, ascites, weight gain, and respiratory distress in children aged 1-10 years. Investigations show proteinuria, hypoalbuminemia, and normal renal function. Management involves steroid therapy, addressing complications, and educating parents on infection prevention and immunization.