1. This case presentation summarizes a 55-year-old male farmer who presented with abdominal swelling and discomfort for 2 months and scanty urination and constipation for 1 month.
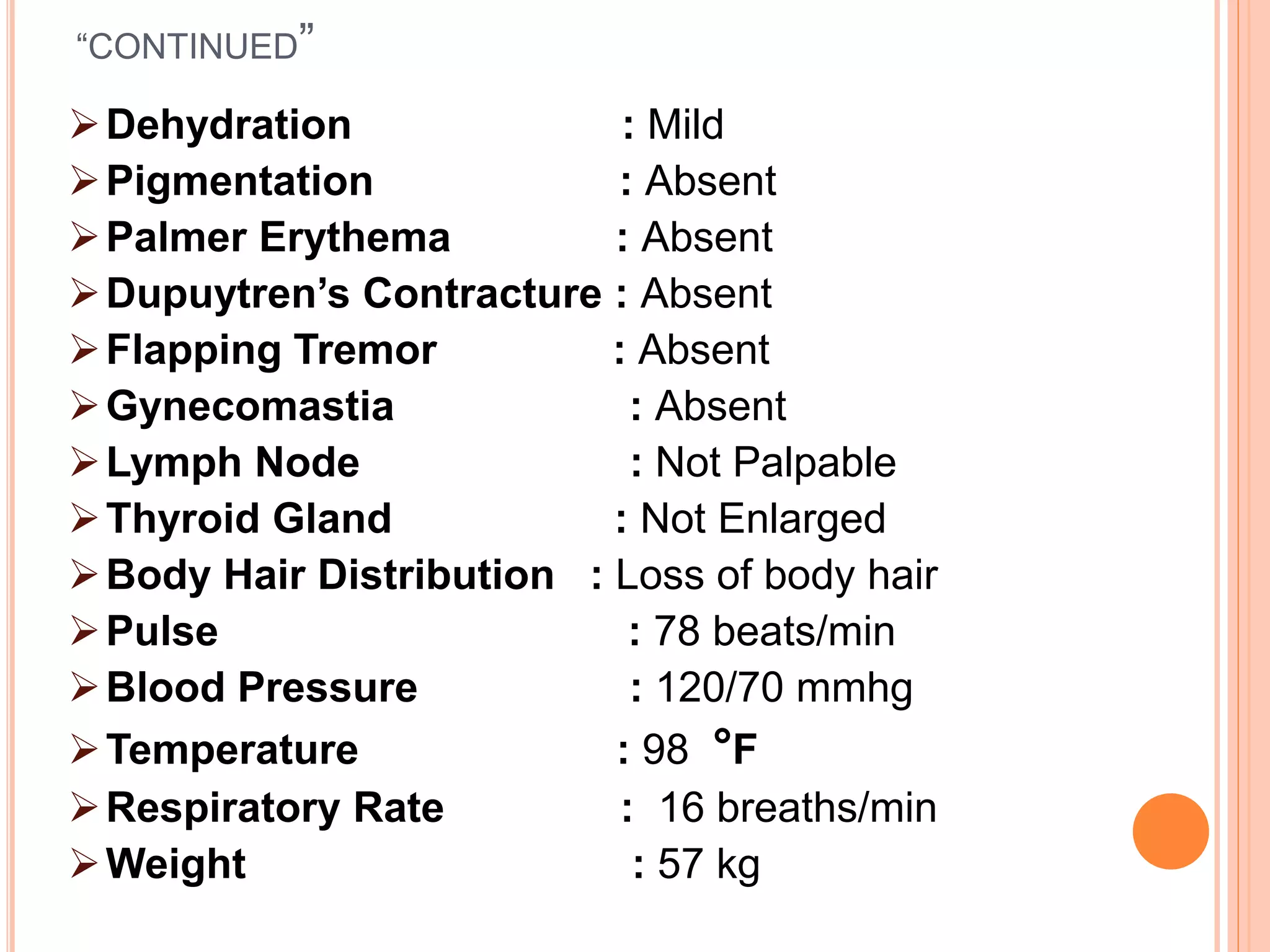
2. On examination, he had signs of chronic liver disease including jaundice, edema, and hepatic encephalopathy.
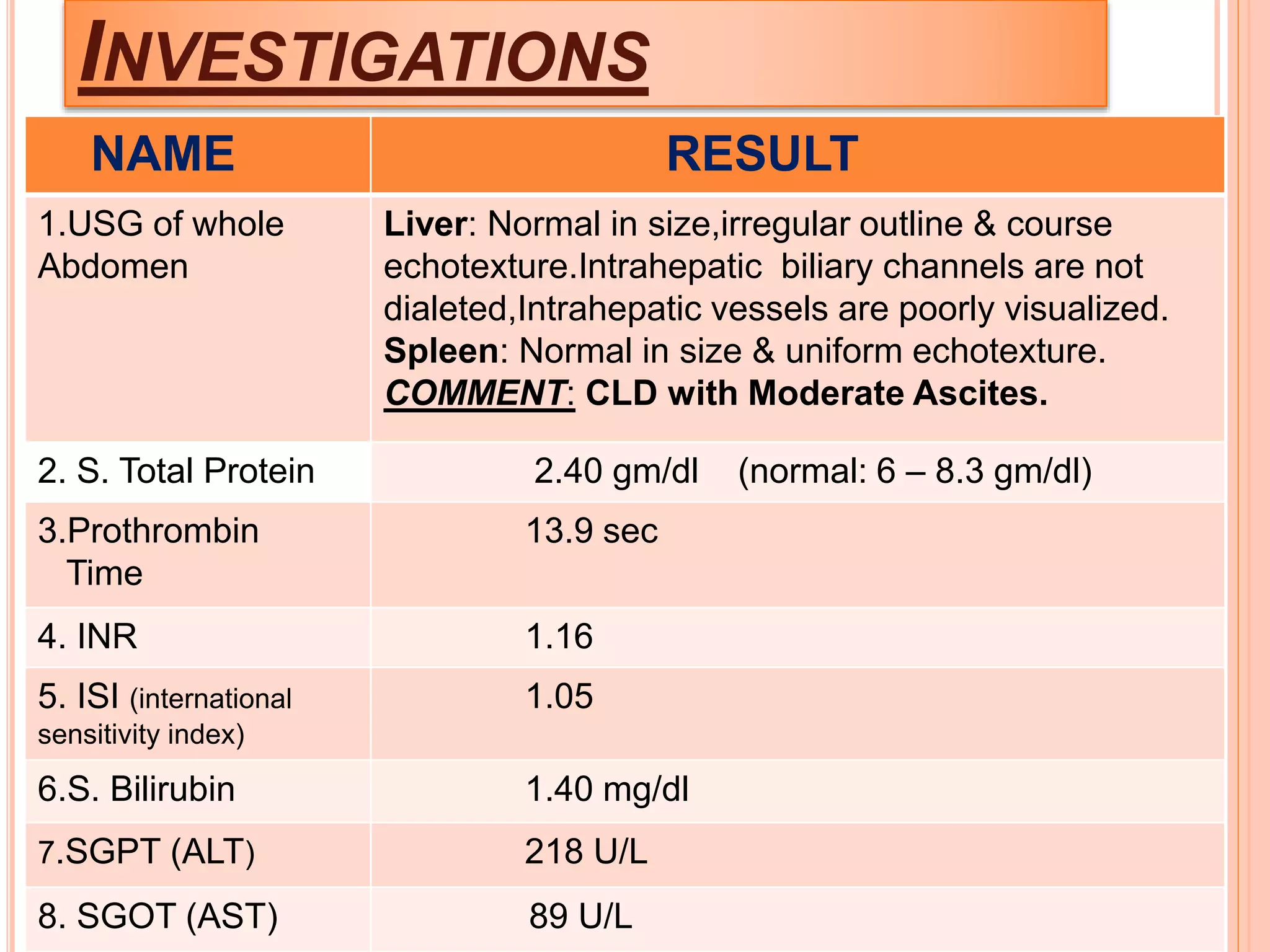
3. Investigations confirmed chronic hepatitis B infection, decompensated cirrhosis, and grade 2-4 esophageal varices.
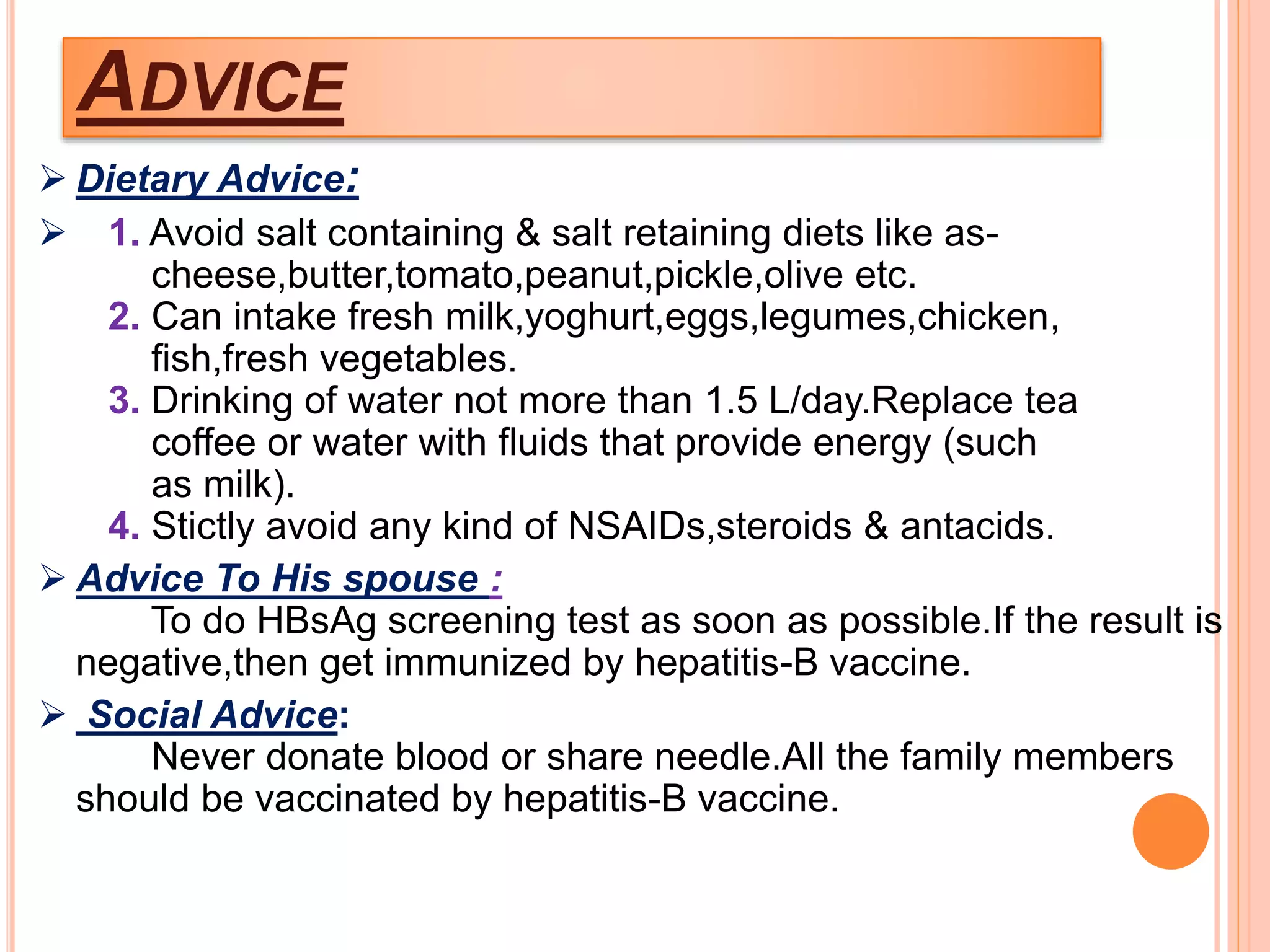
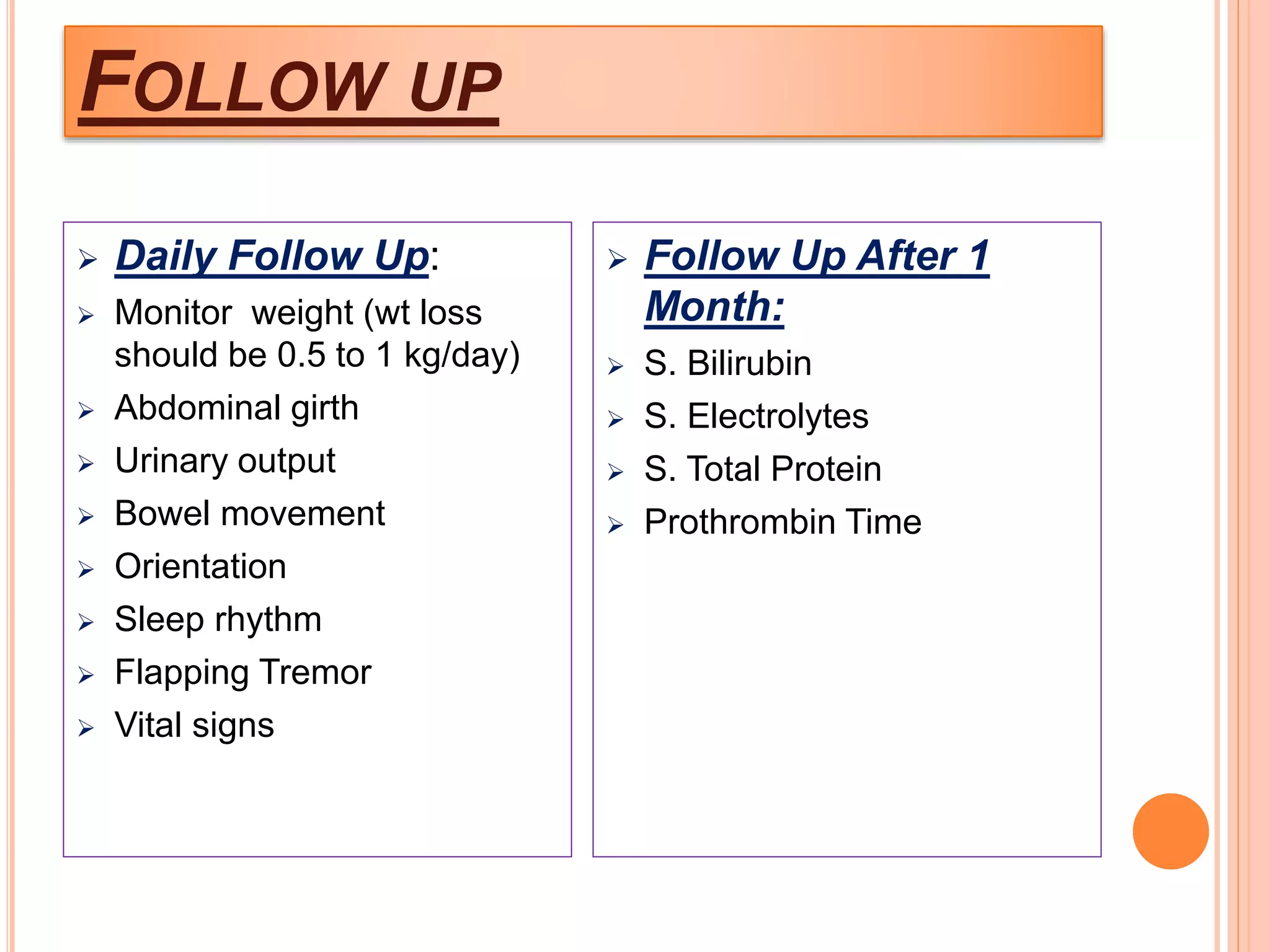
4. He was diagnosed with decompensated chronic liver disease and grade 1 hepatic encephalopathy, and started on treatment including diuretics, beta-blockers, lactulose, and vitamin supplementation.