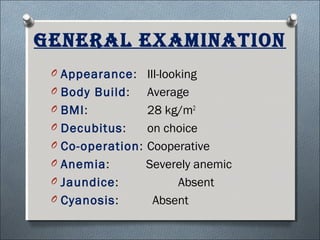
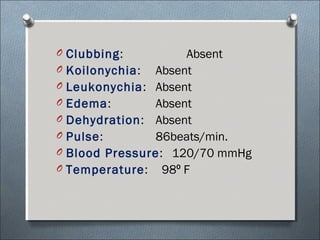
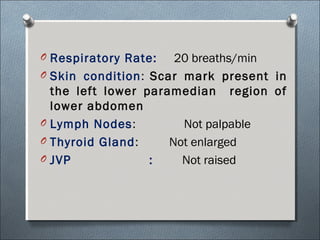
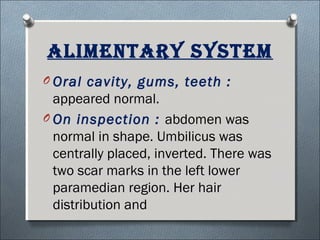
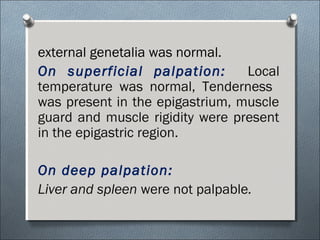
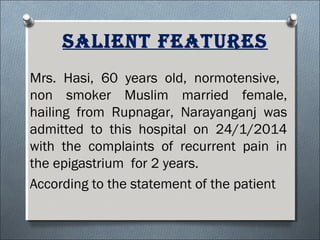
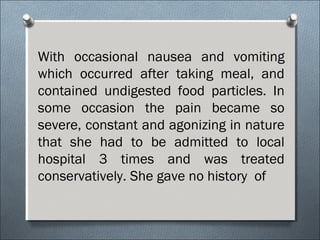
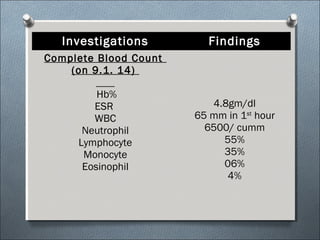
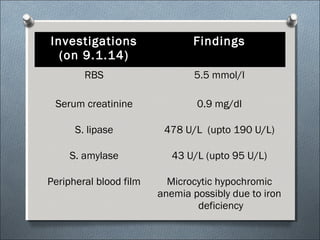
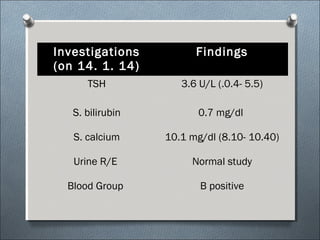
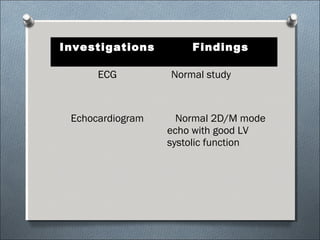
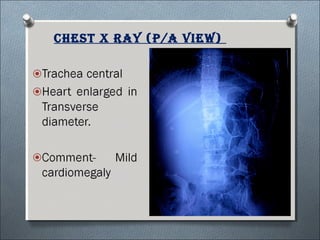
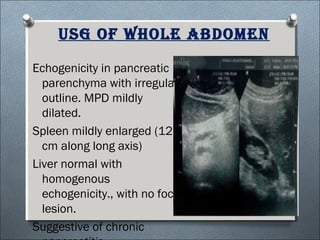
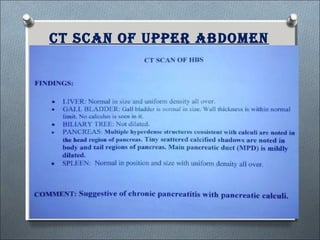
This document summarizes a clinical meeting discussing a 60-year-old female patient presenting with recurrent upper abdominal pain over the past 2 years. Examination findings included tenderness and guarding in the epigastrium. Investigations revealed elevated serum lipase, anemia, and ultrasound findings suggestive of chronic pancreatitis. The provisional diagnosis was chronic pancreatitis, with differential diagnoses of chronic cholecystitis or peptic ulcer disease. CT scan and laboratory results confirmed the diagnosis of chronic pancreatitis due to pancreatic calculi, complicated by iron deficiency anemia.