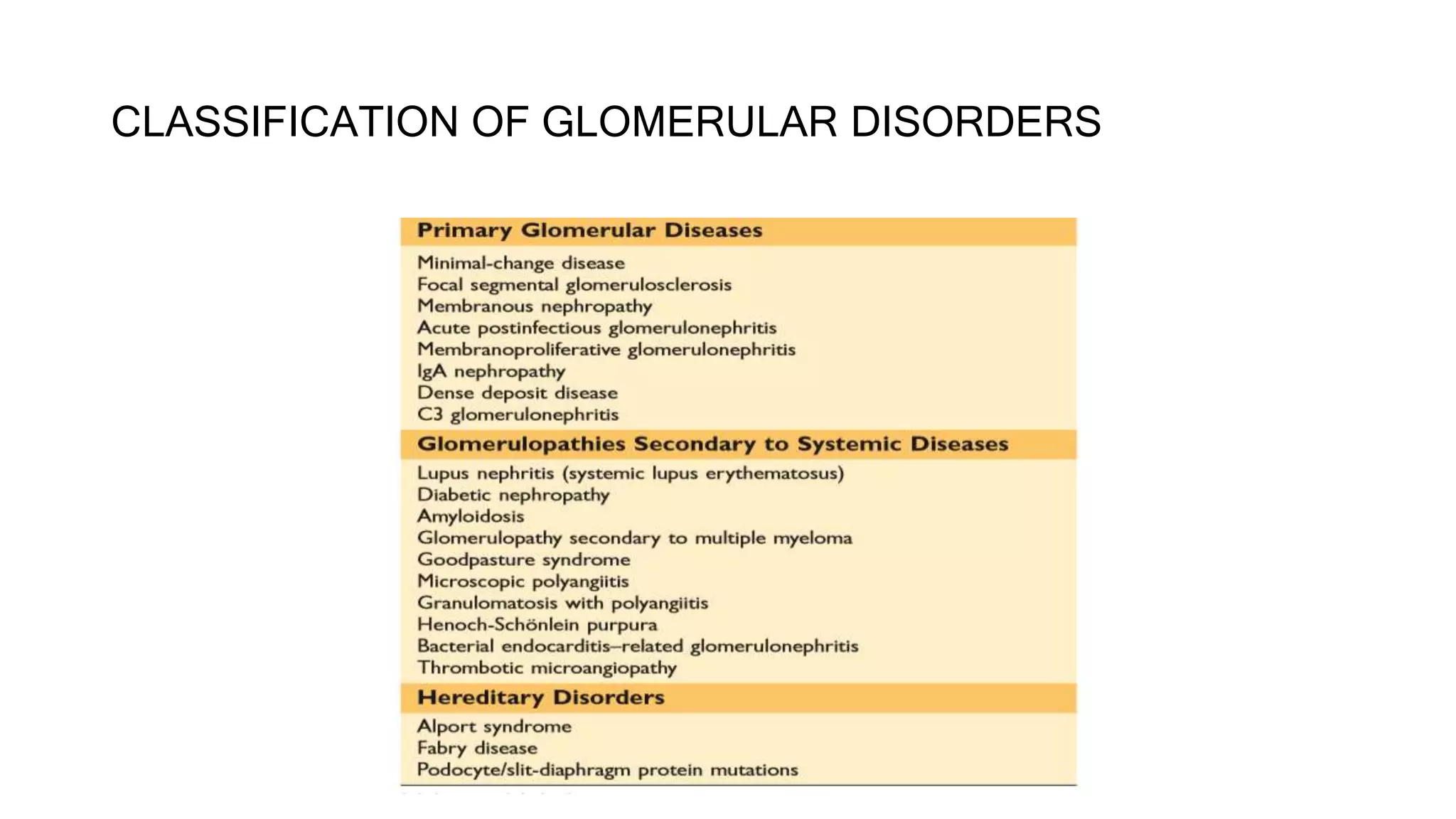
The document discusses acute nephritic syndromes, their classification, pathogenesis, and clinical presentations, emphasizing the immune mechanisms involved in various glomerular diseases. It highlights specific causes of acute nephritis in different age groups, along with diagnostic approaches and laboratory evaluations. Management strategies and prognosis for conditions such as post-streptococcal glomerulonephritis, lupus nephritis, and ANCA-associated glomerulonephritis are also examined.