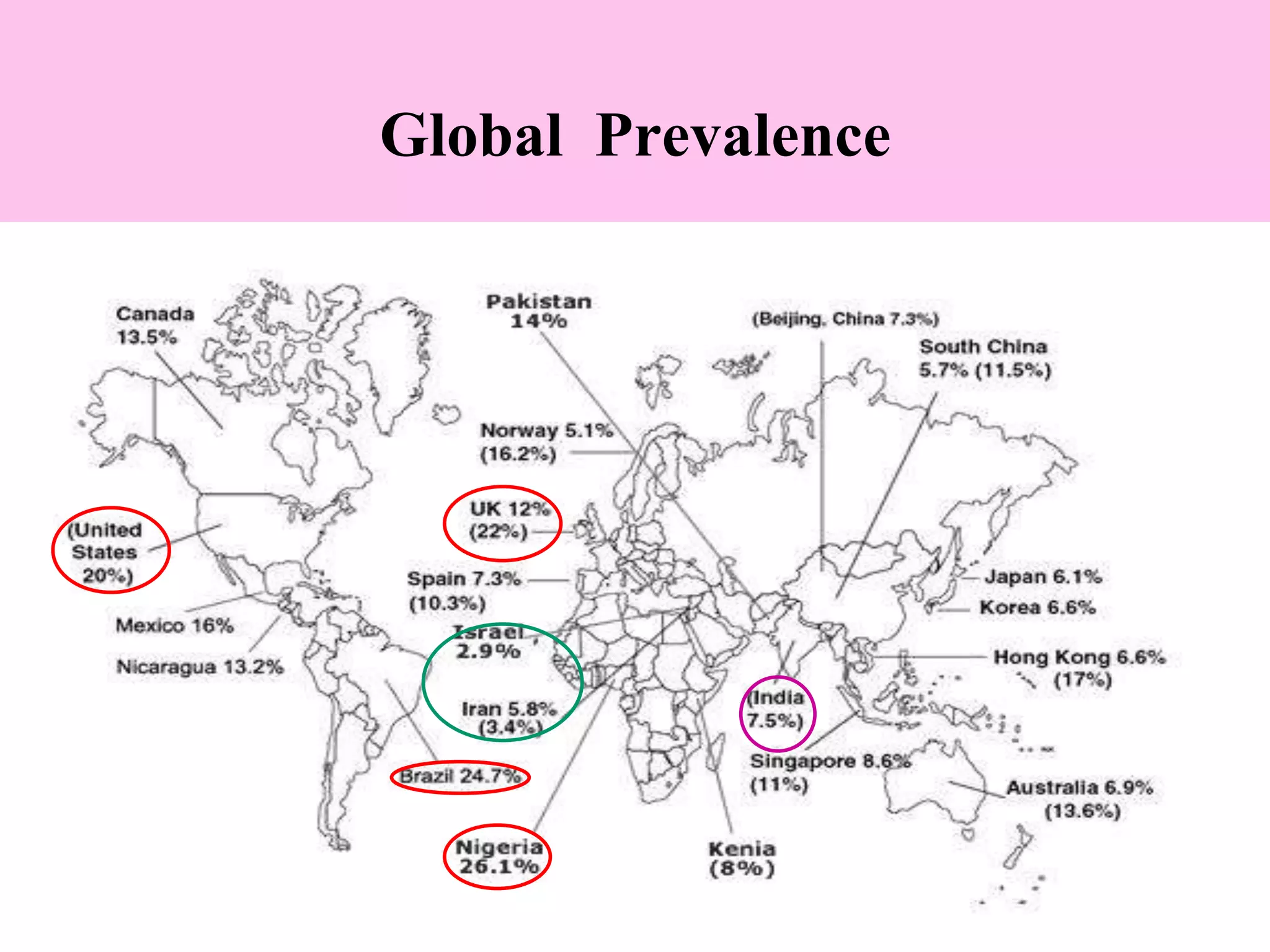
This document provides an overview of irritable bowel syndrome (IBS), including its definition, prevalence, demographics, pathophysiology, clinical features, diagnosis, differential diagnosis, severity assessment, management, and prognosis. Some key points are:
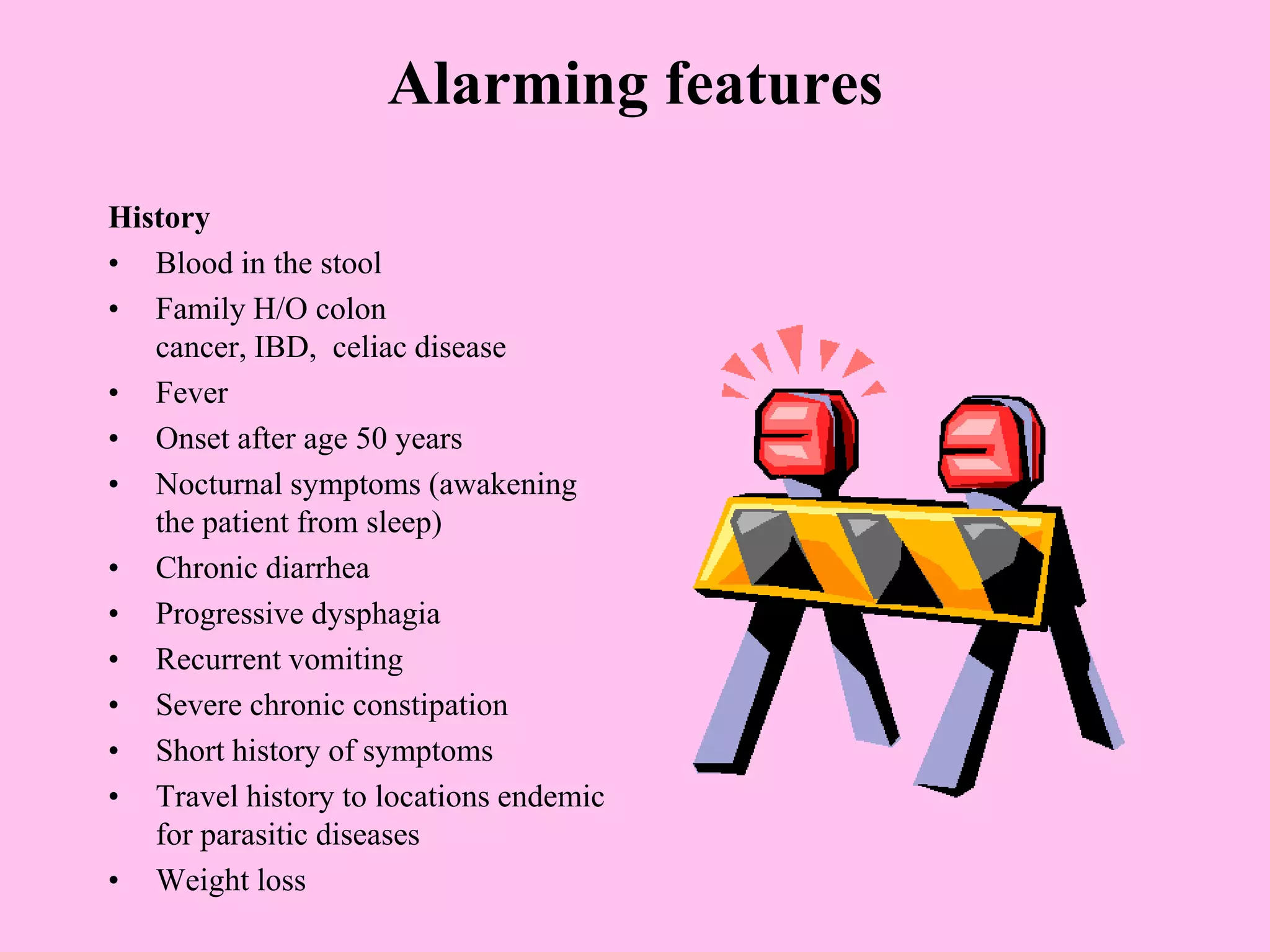
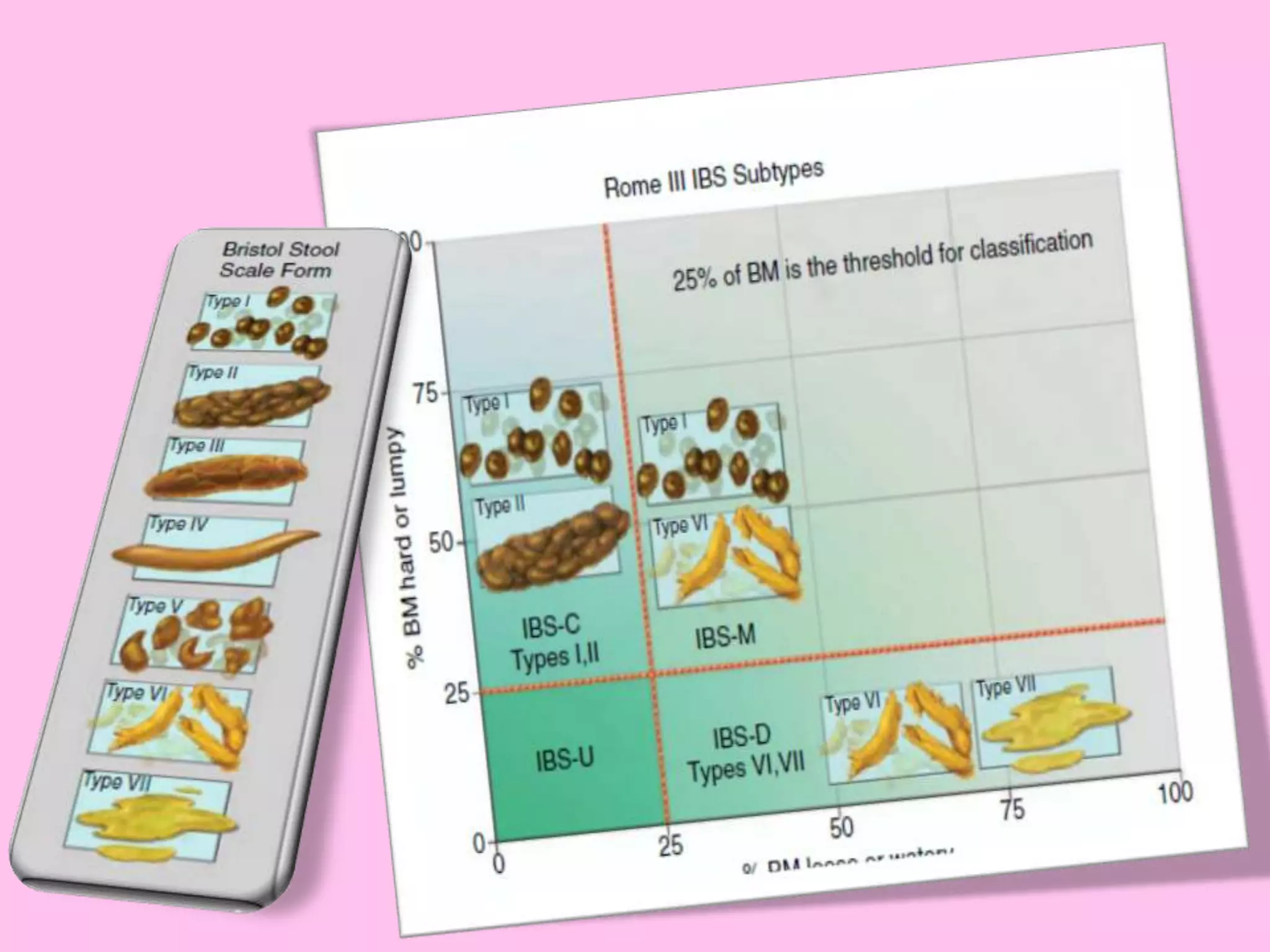
- IBS is a functional bowel disorder characterized by abdominal pain associated with changes in bowel habits. It predominantly affects those aged 15-65 and is more common in women.
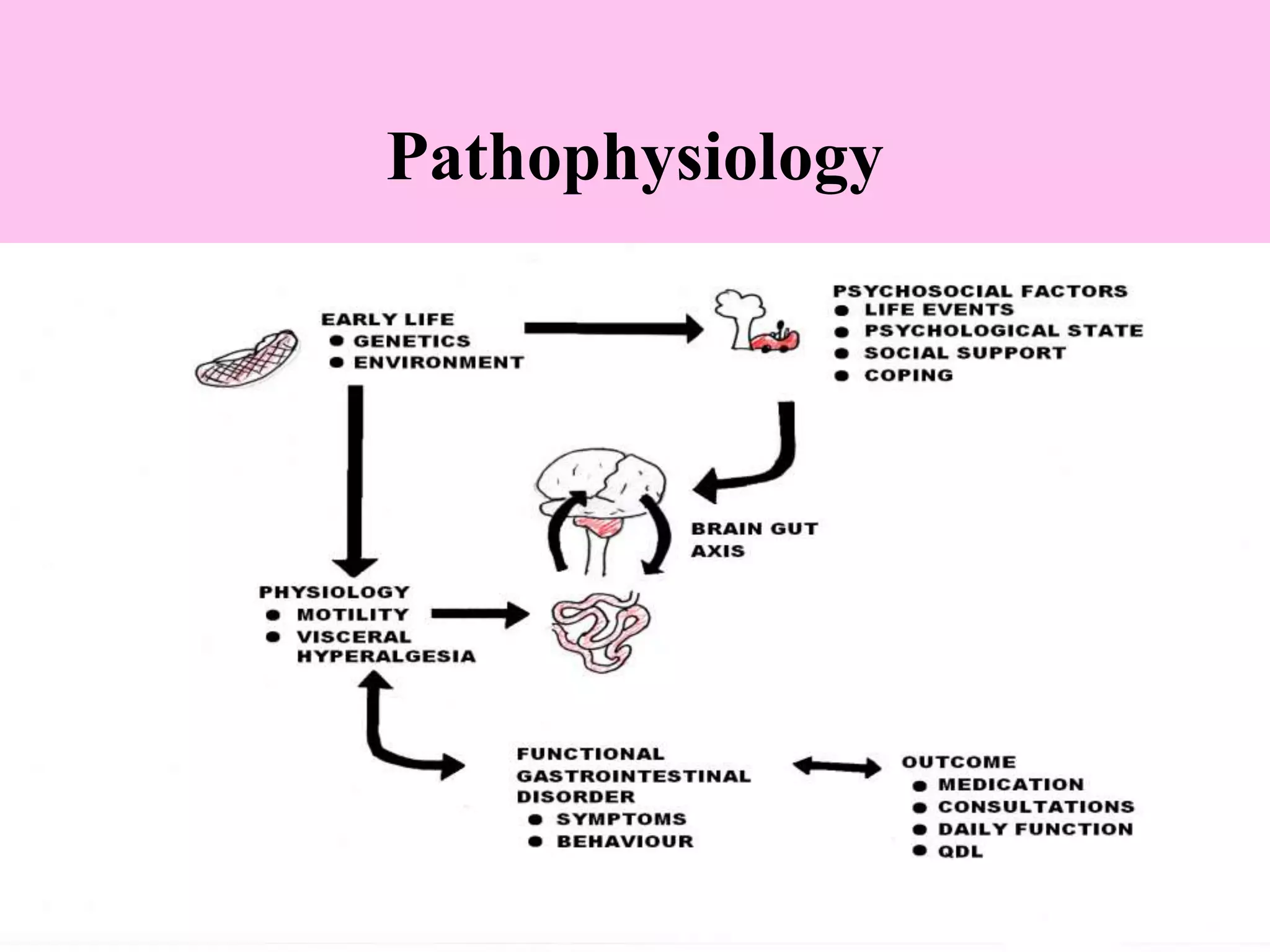
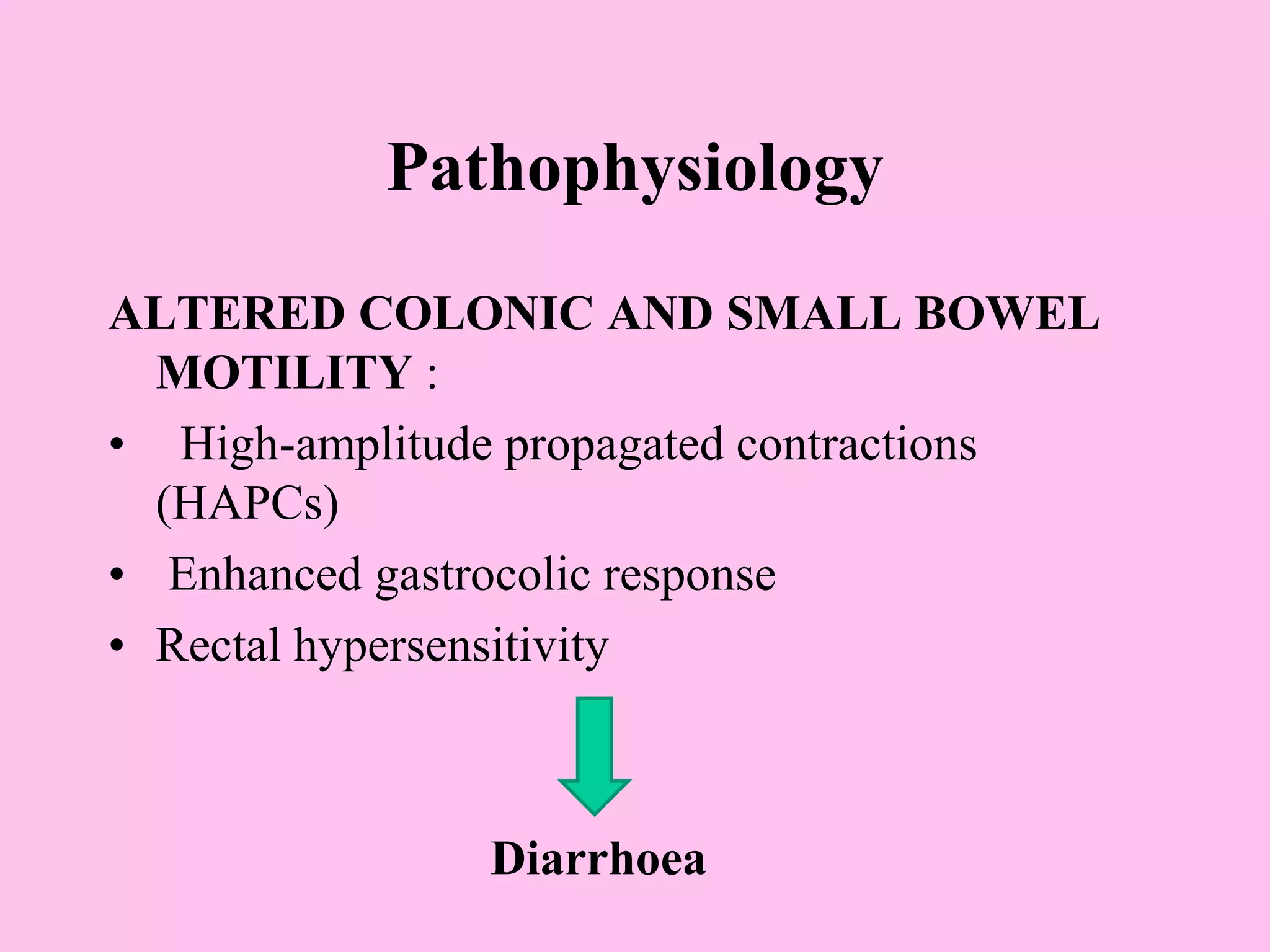
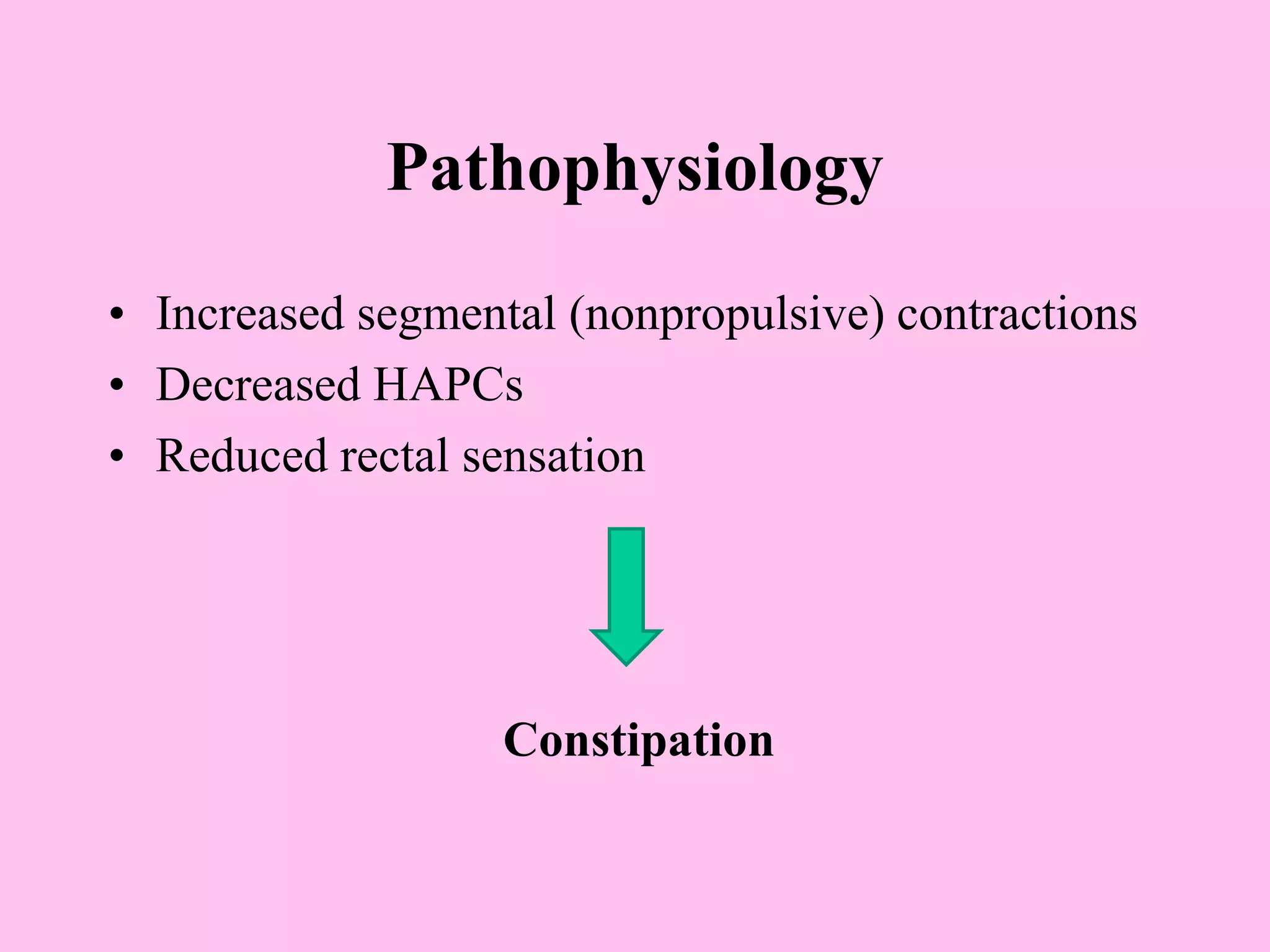
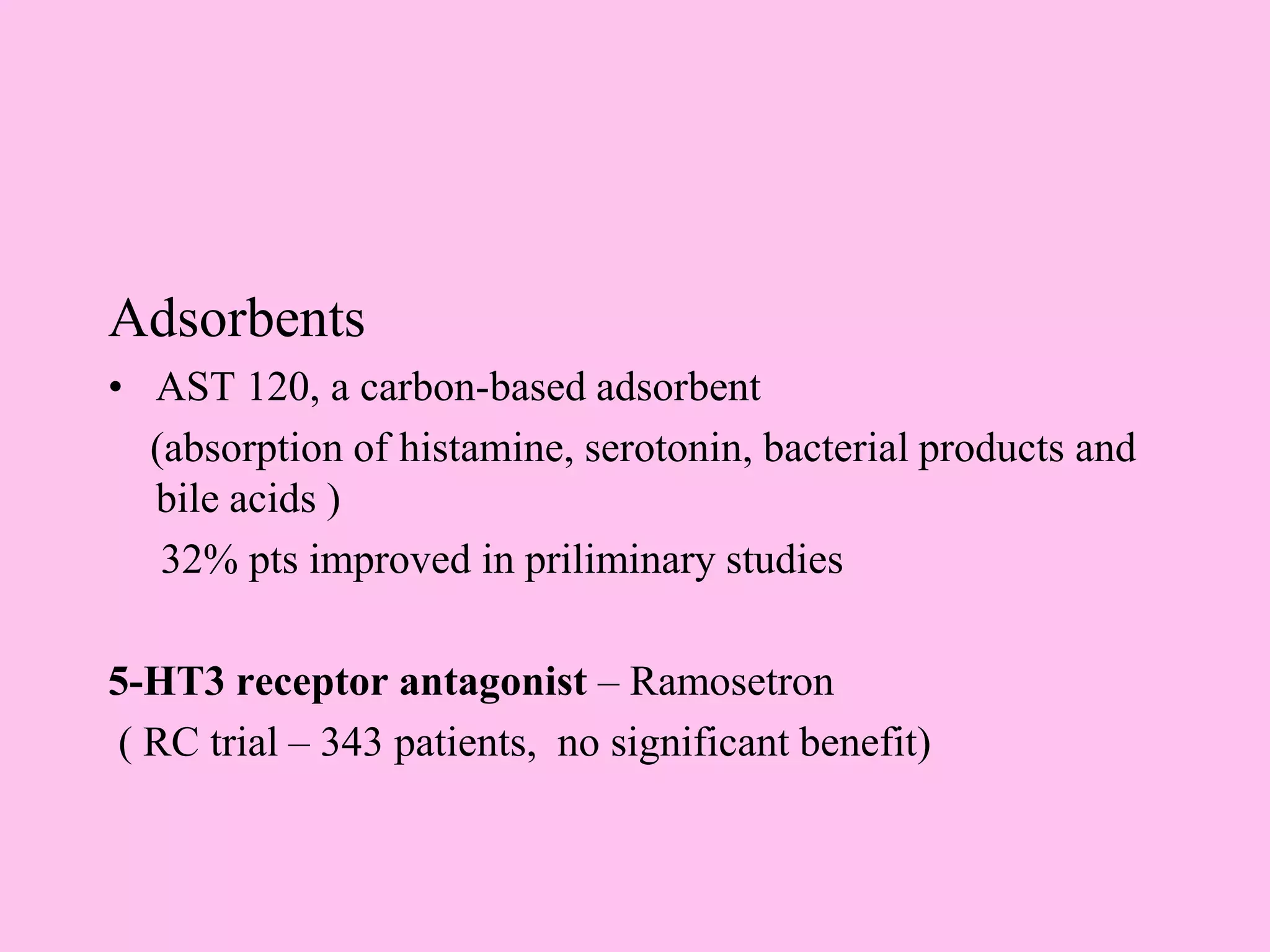
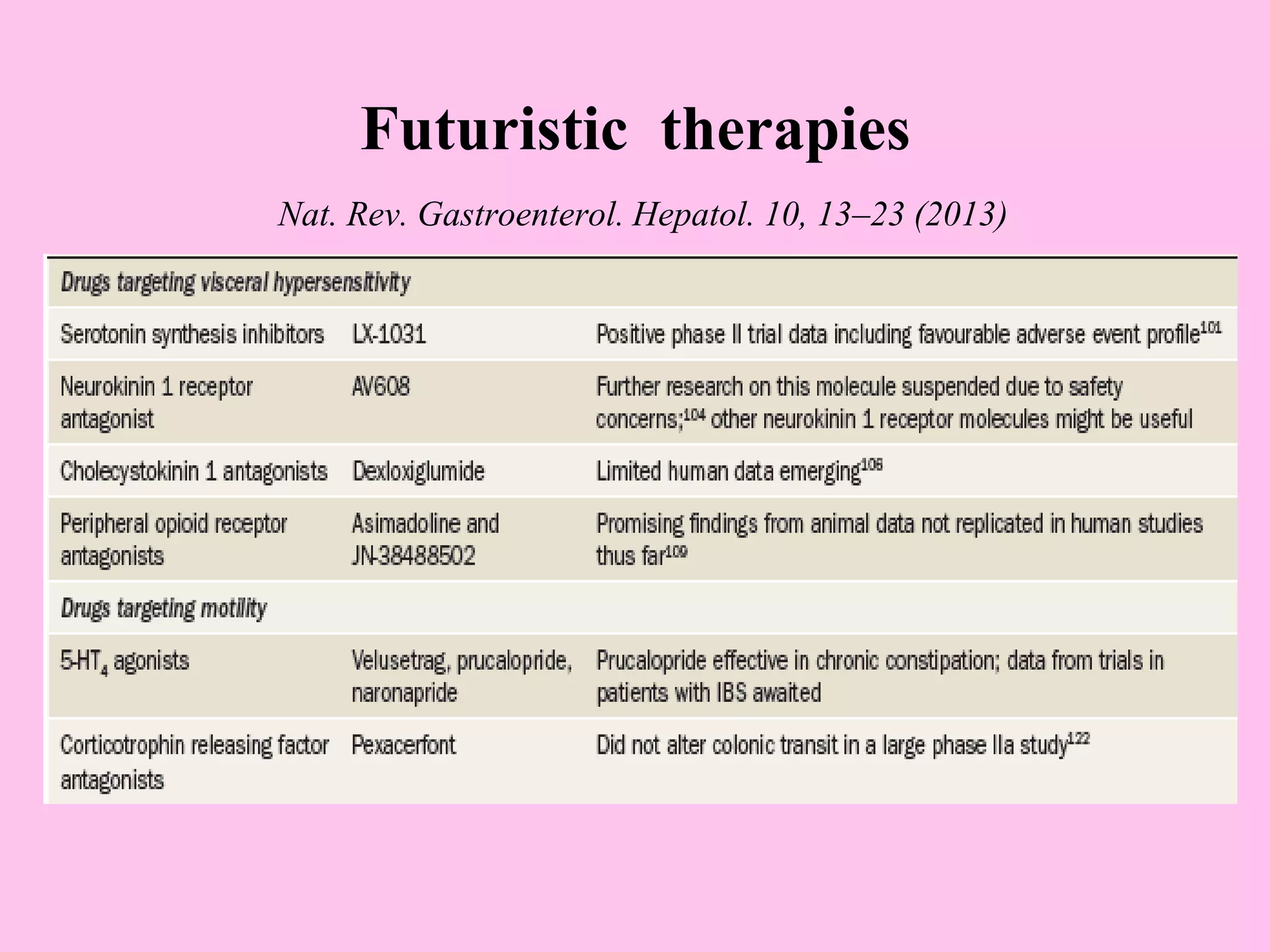
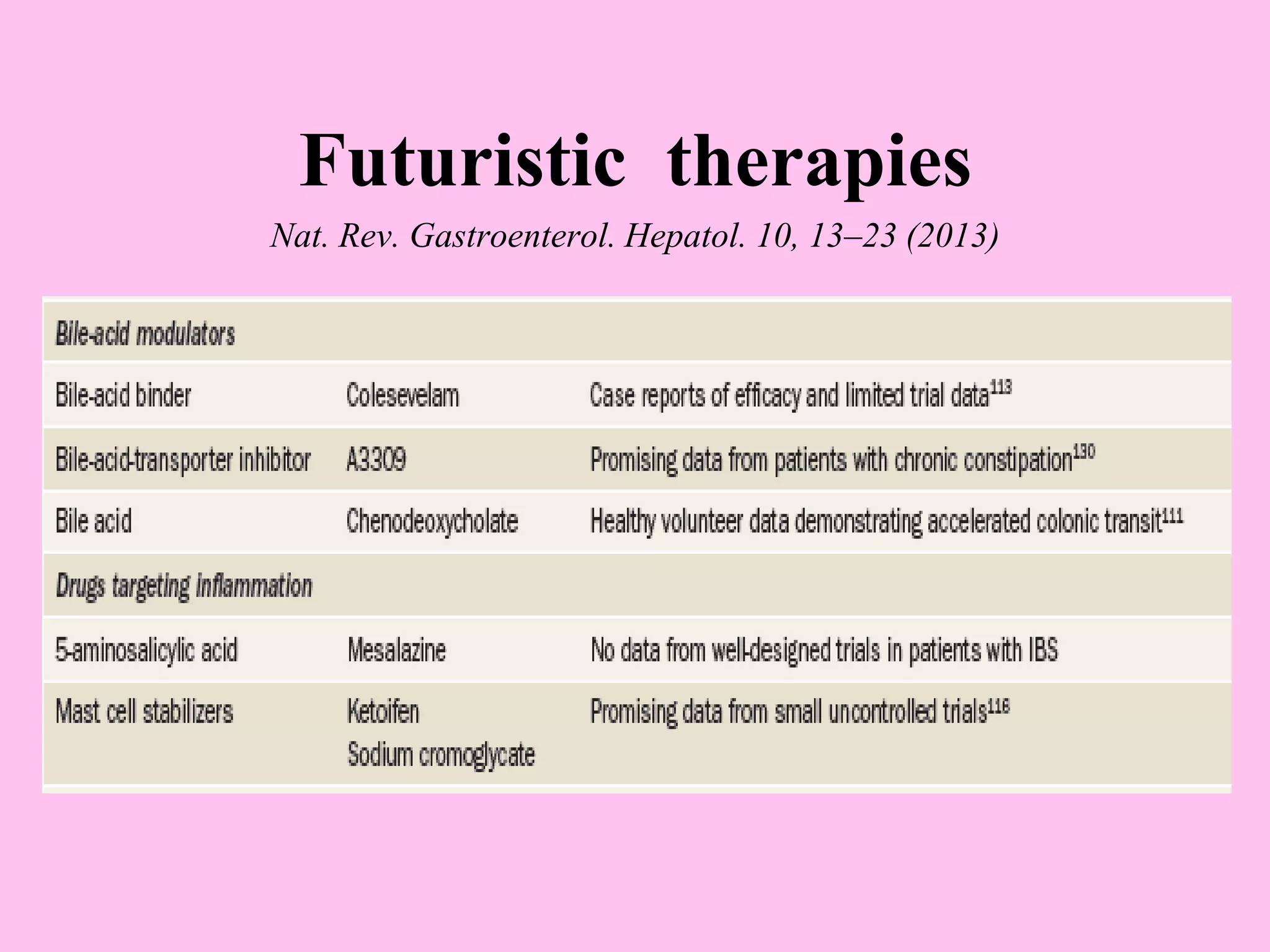
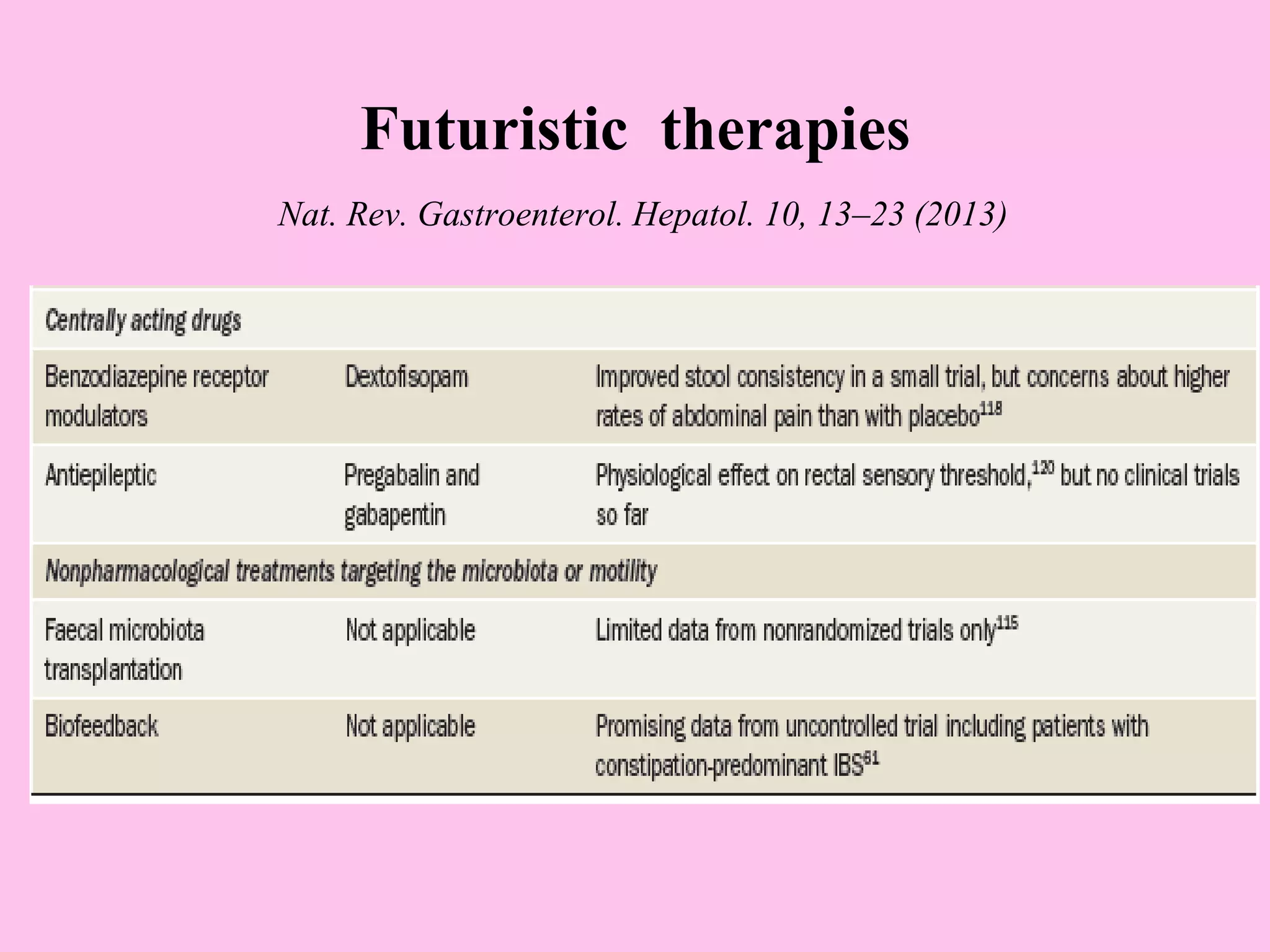
- The pathophysiology involves altered gut motility, visceral hypersensitivity, abnormal gas handling, low-grade inflammation, food sensitivities, abnormal gut microbiota, and central nervous system dysregulation.
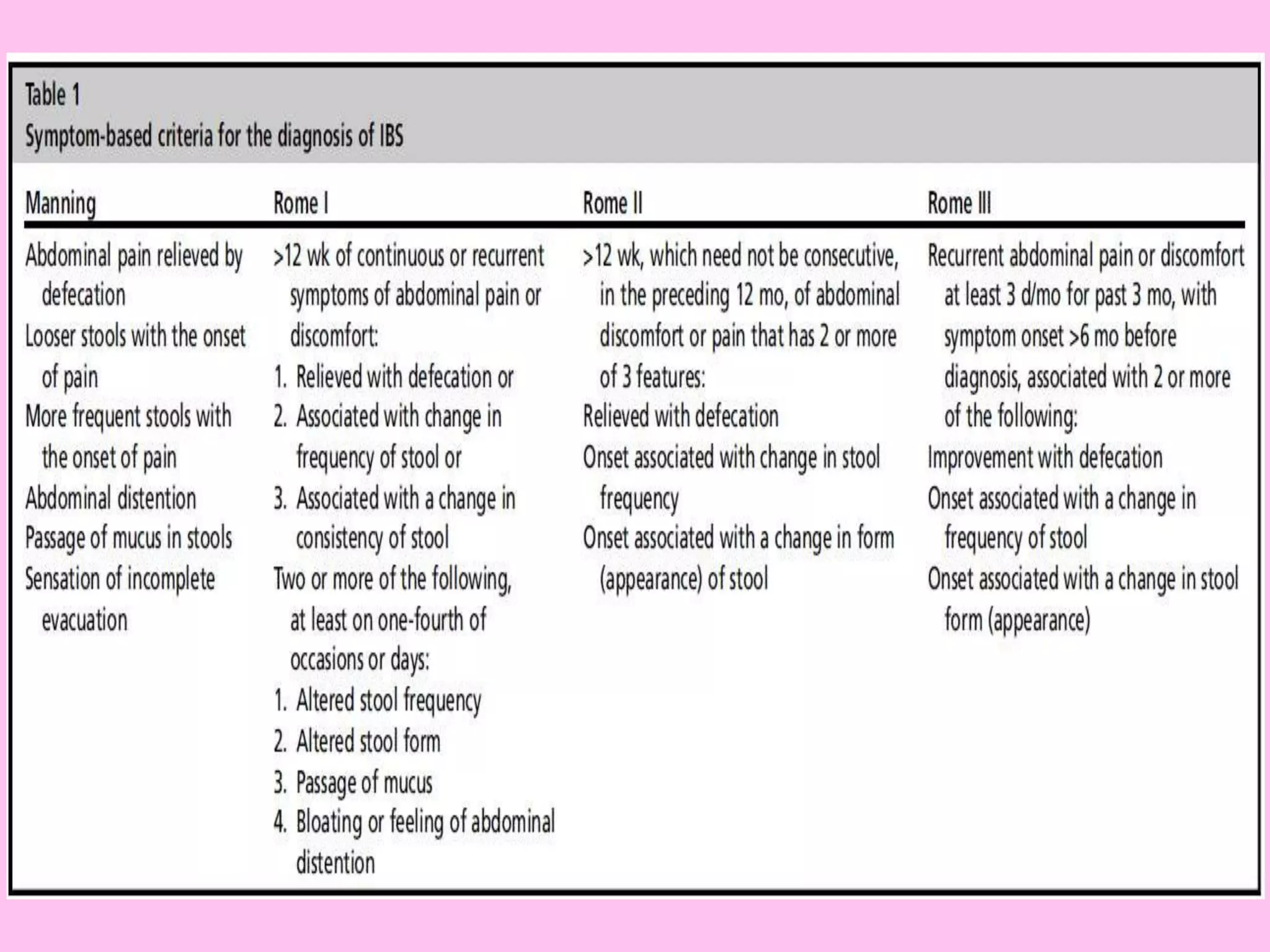
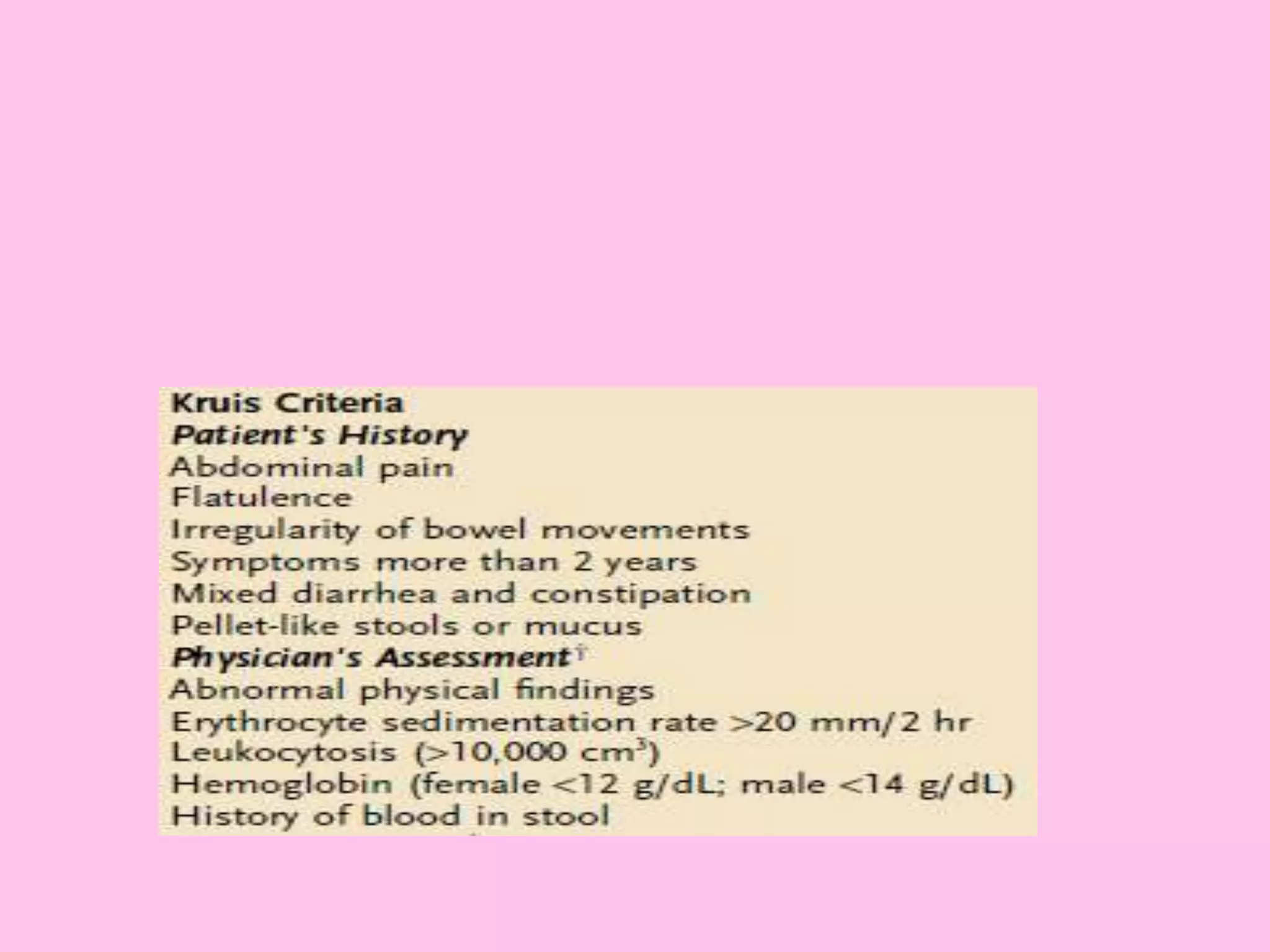
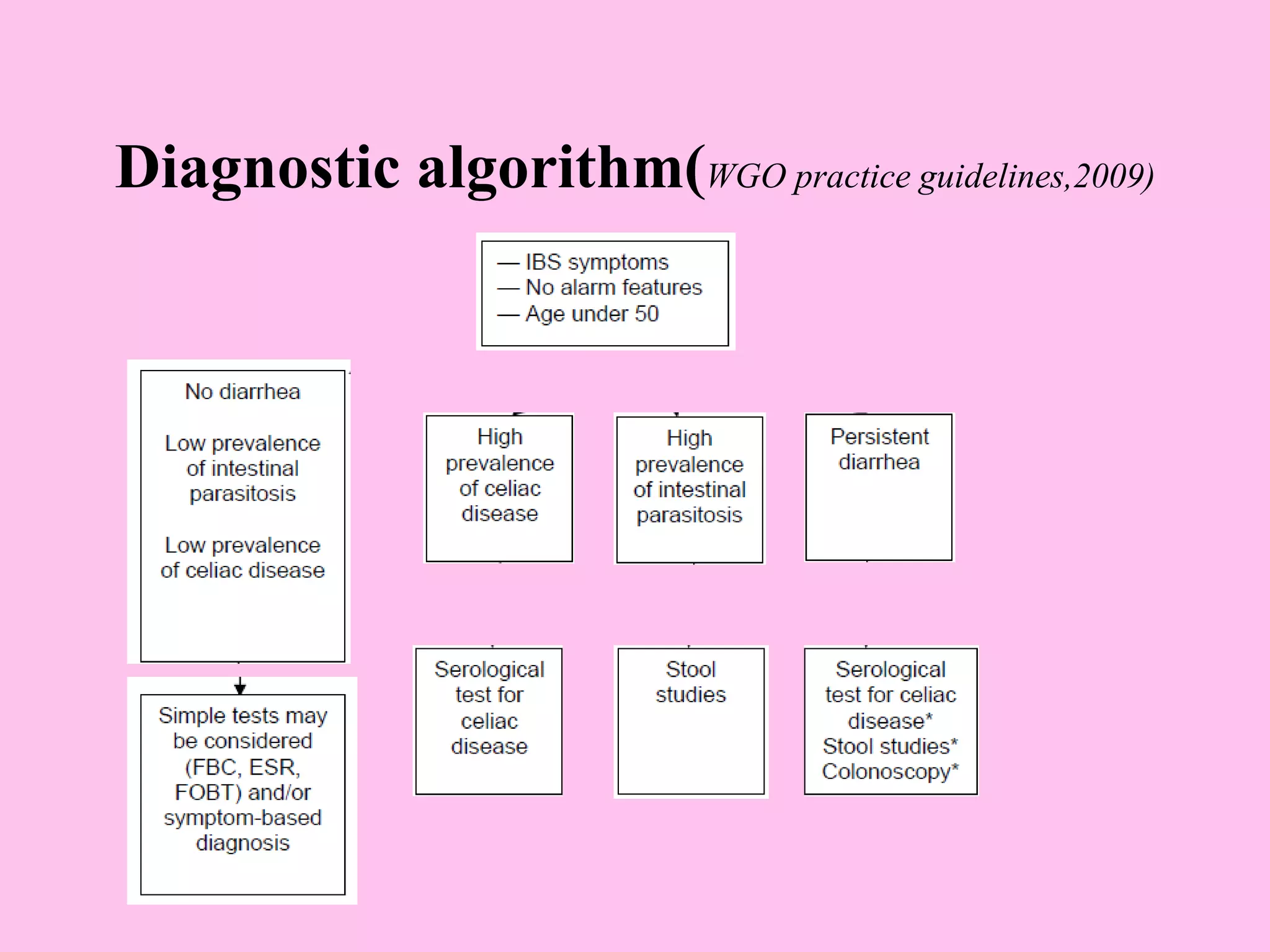
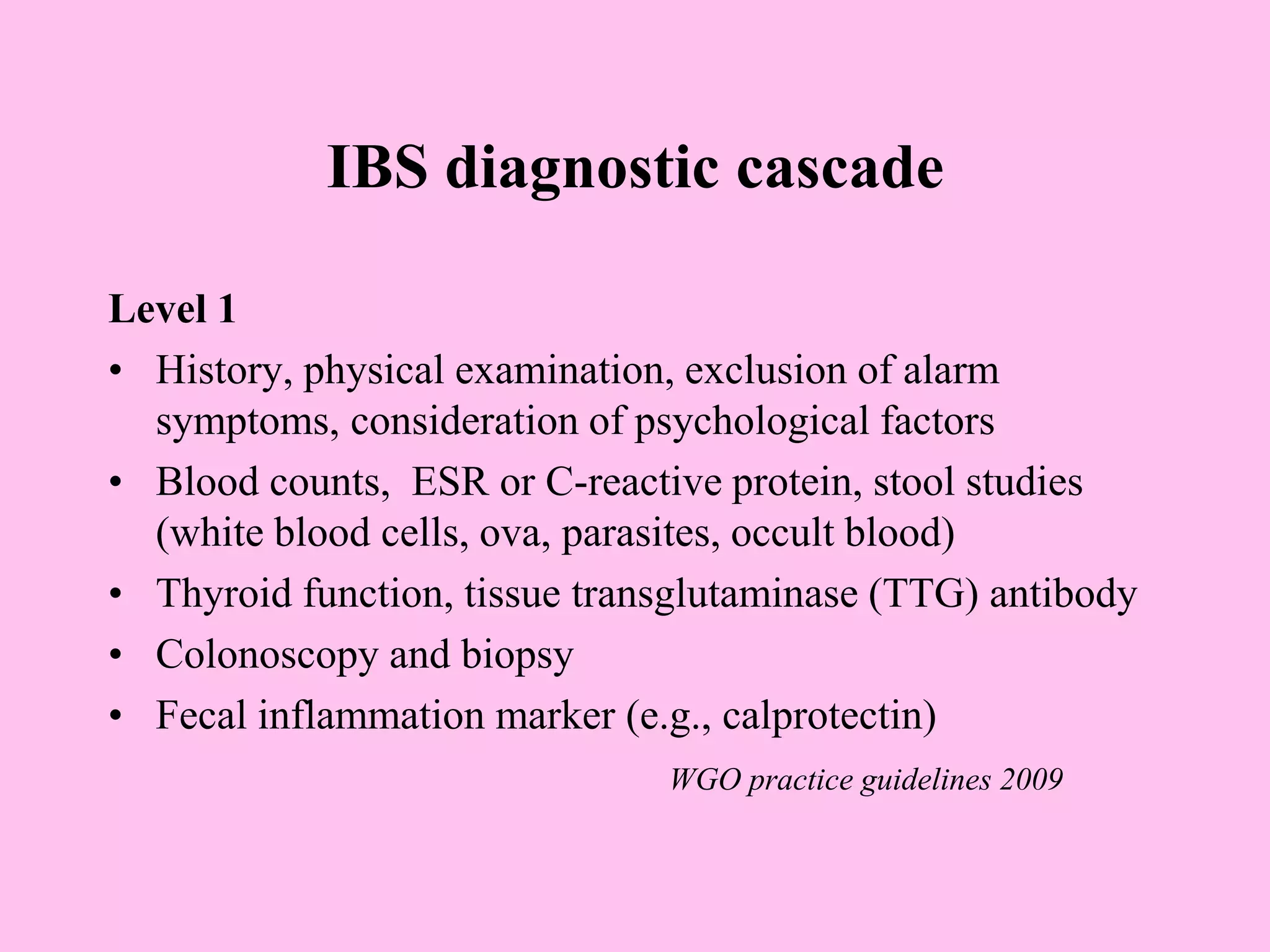
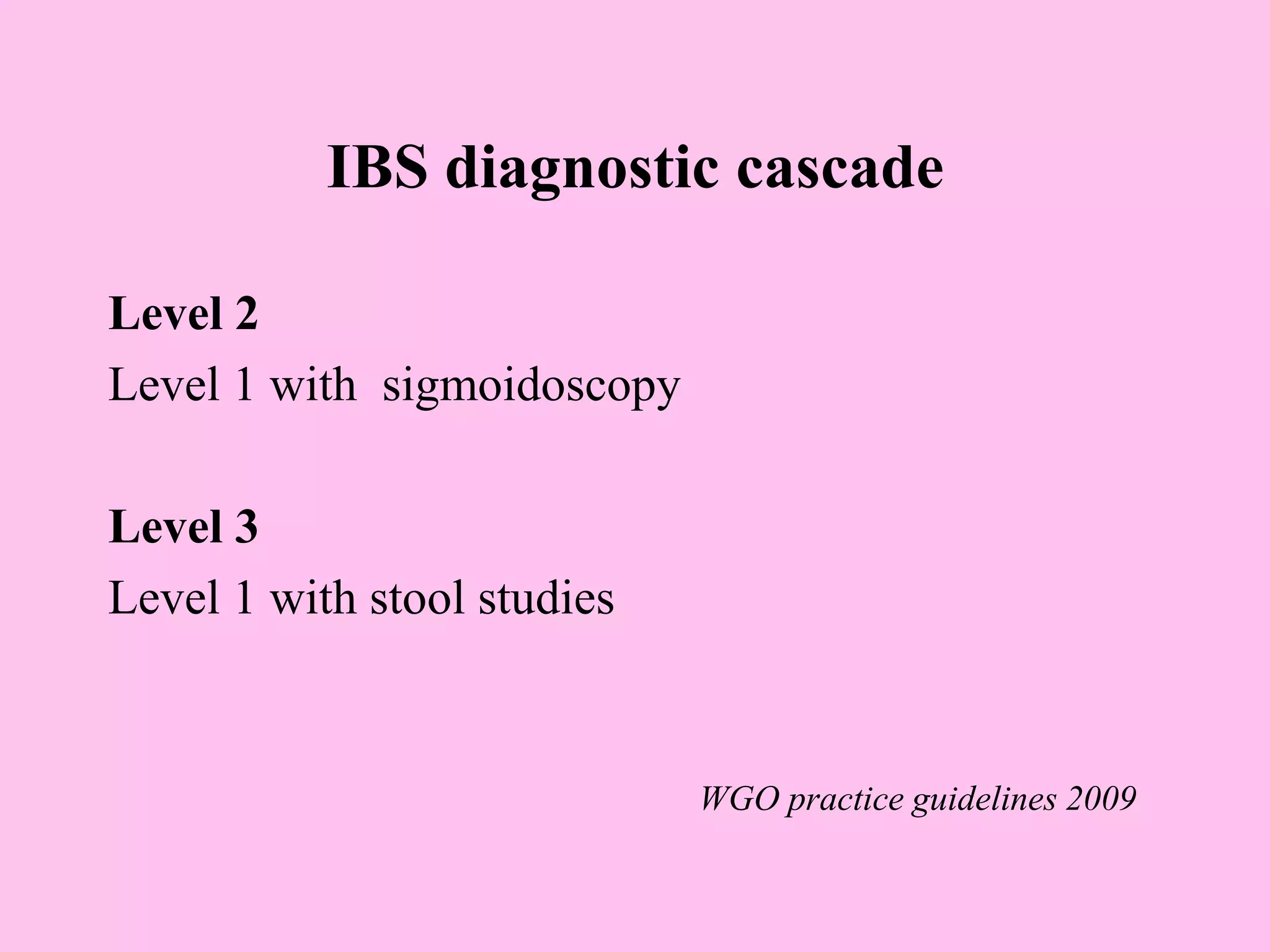
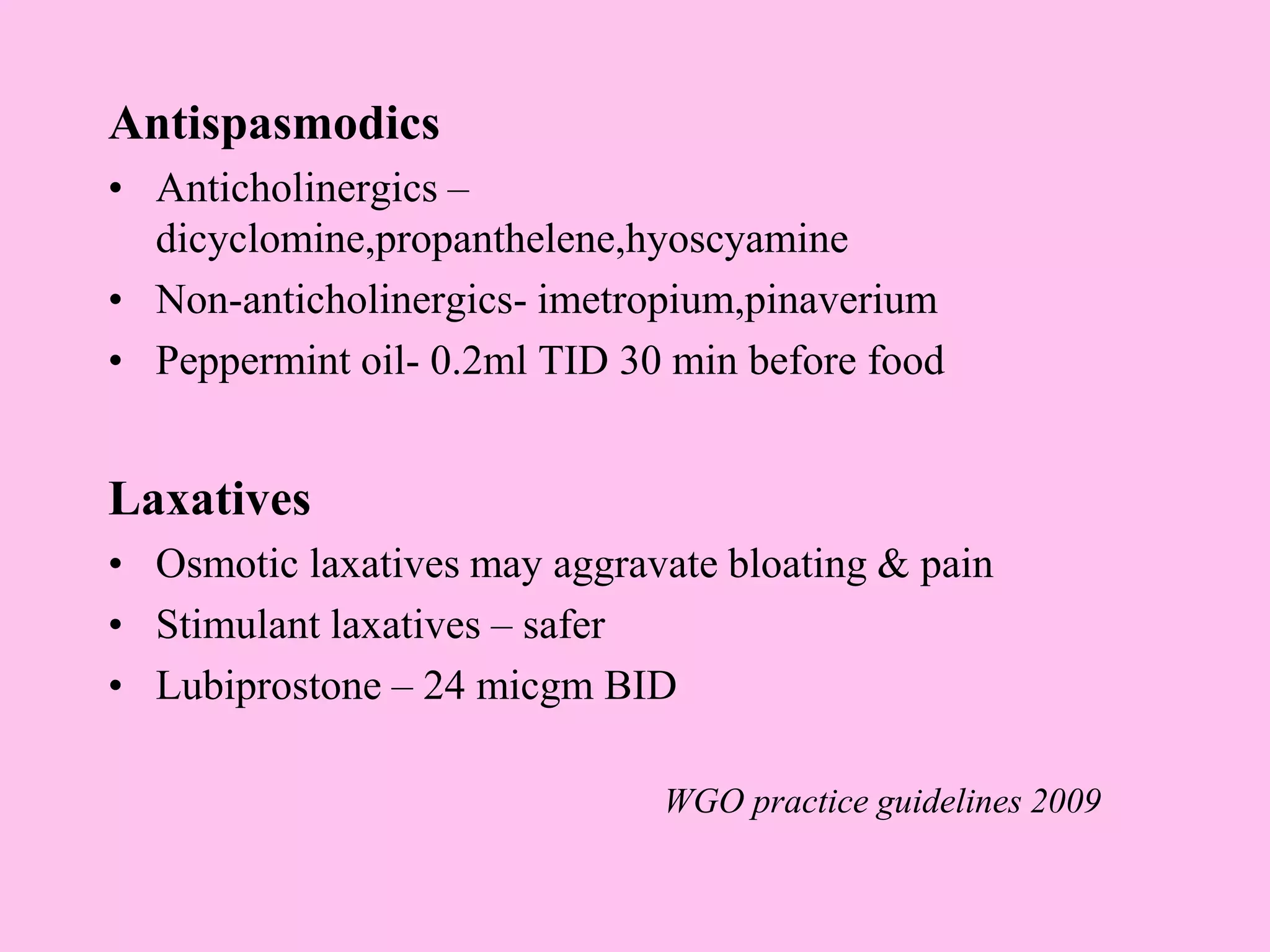
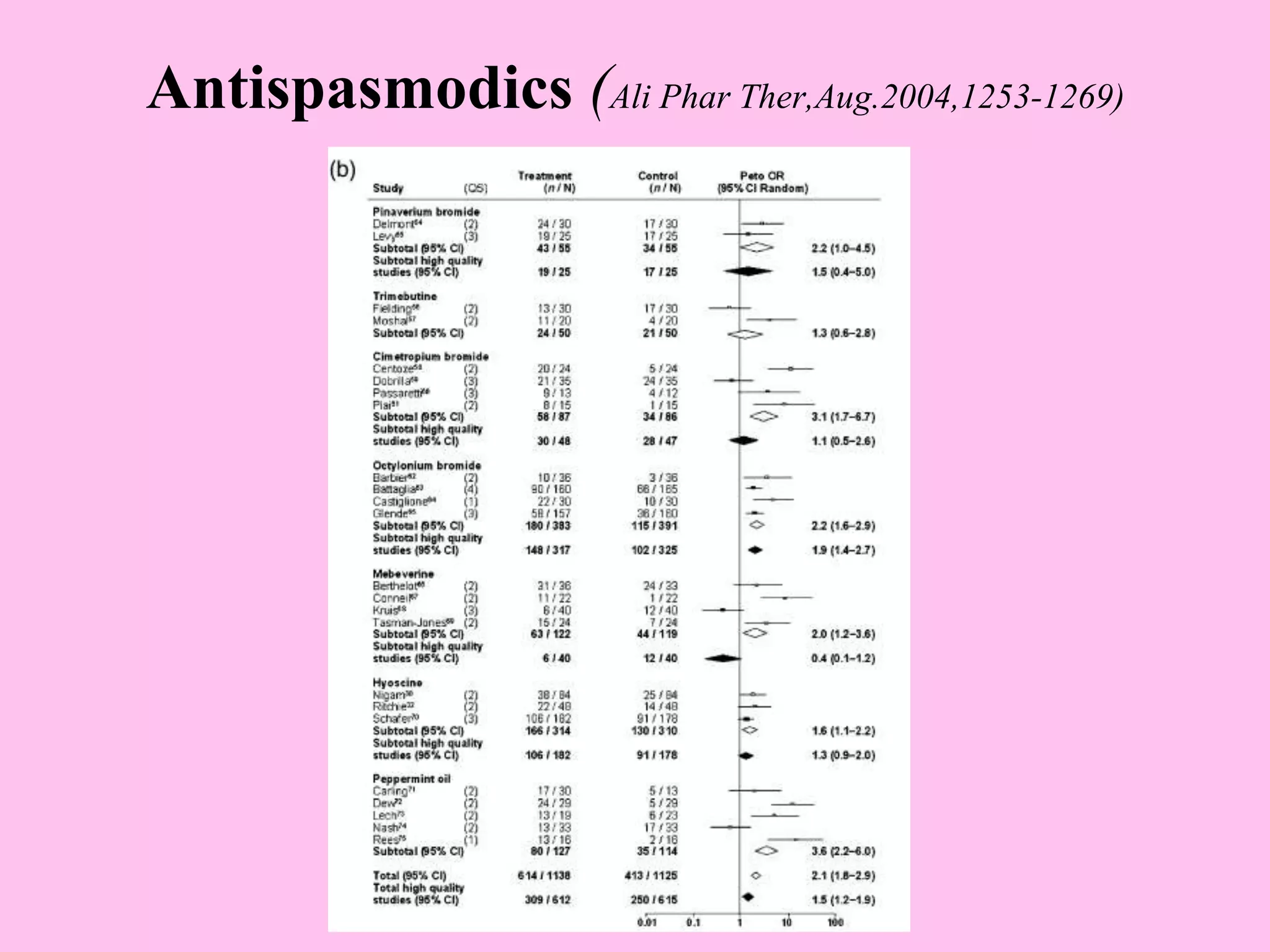
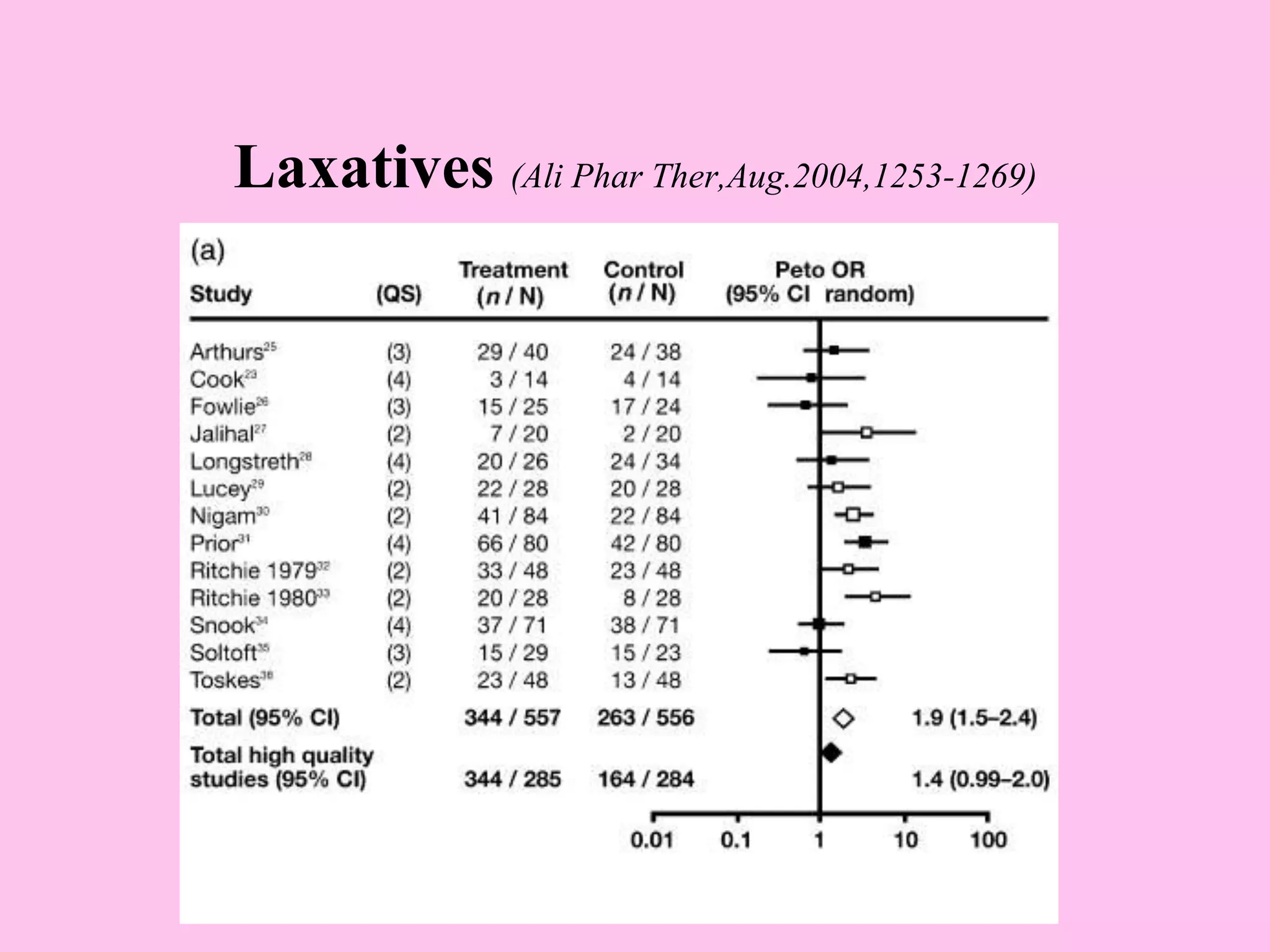
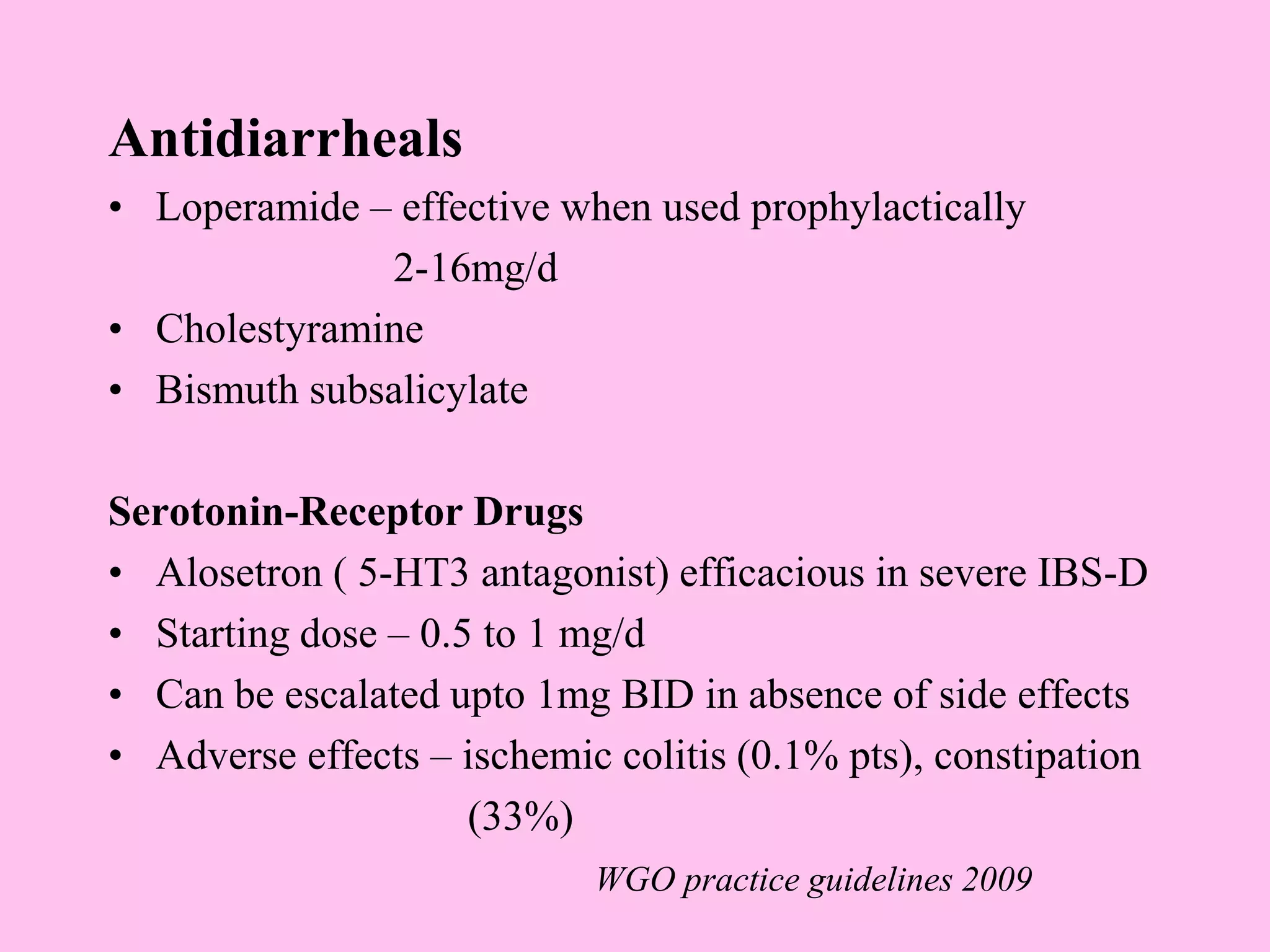
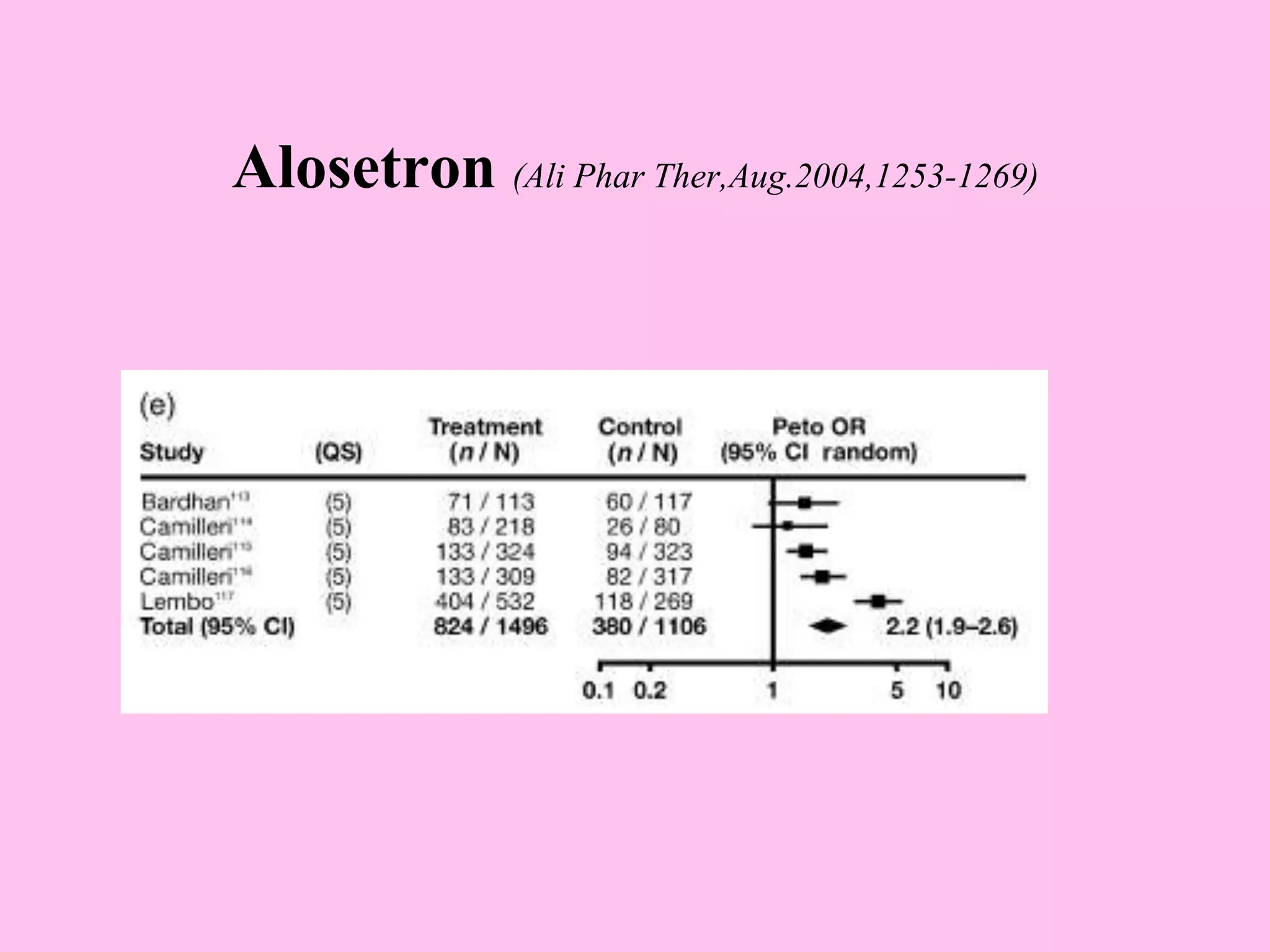
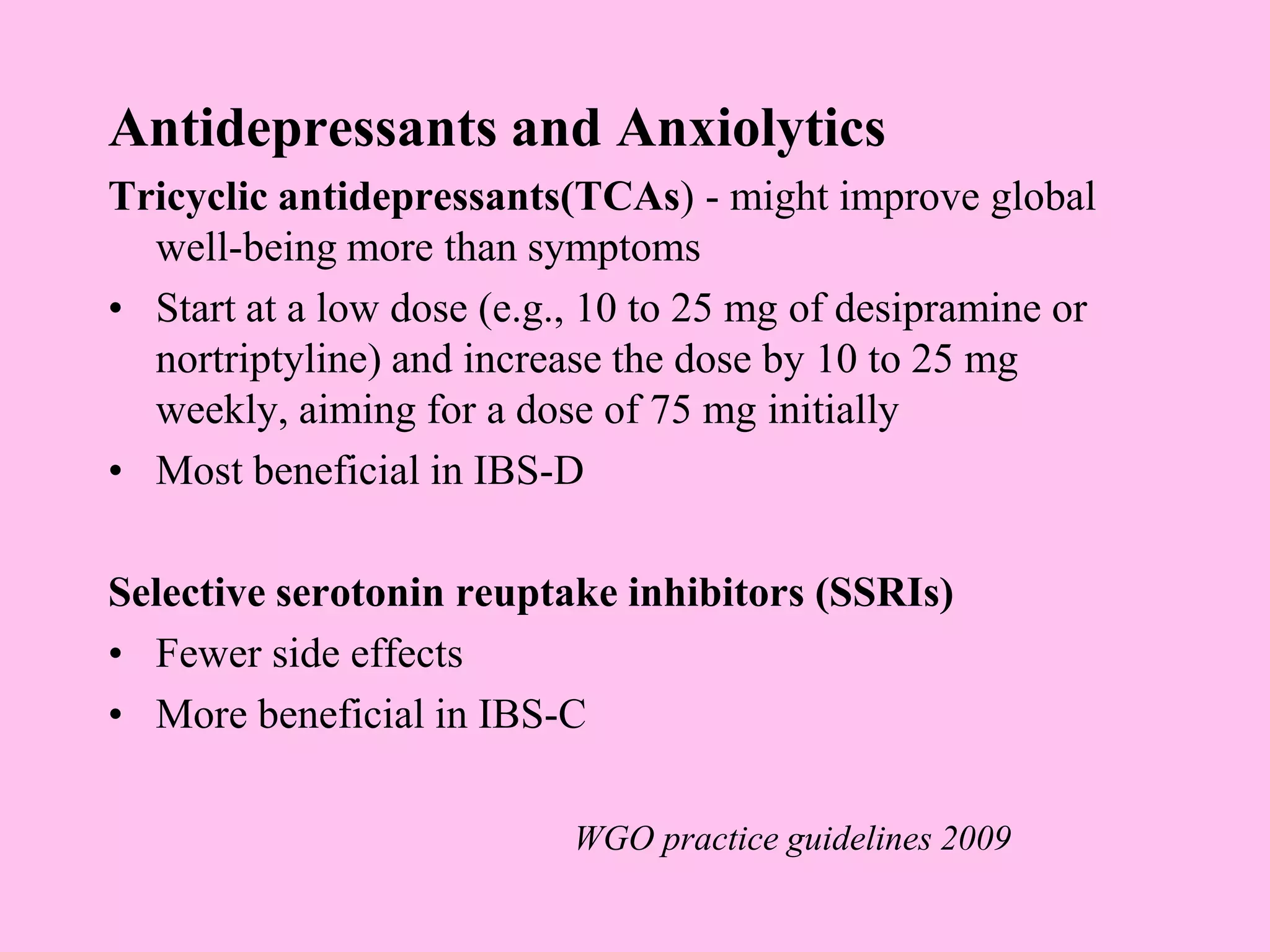
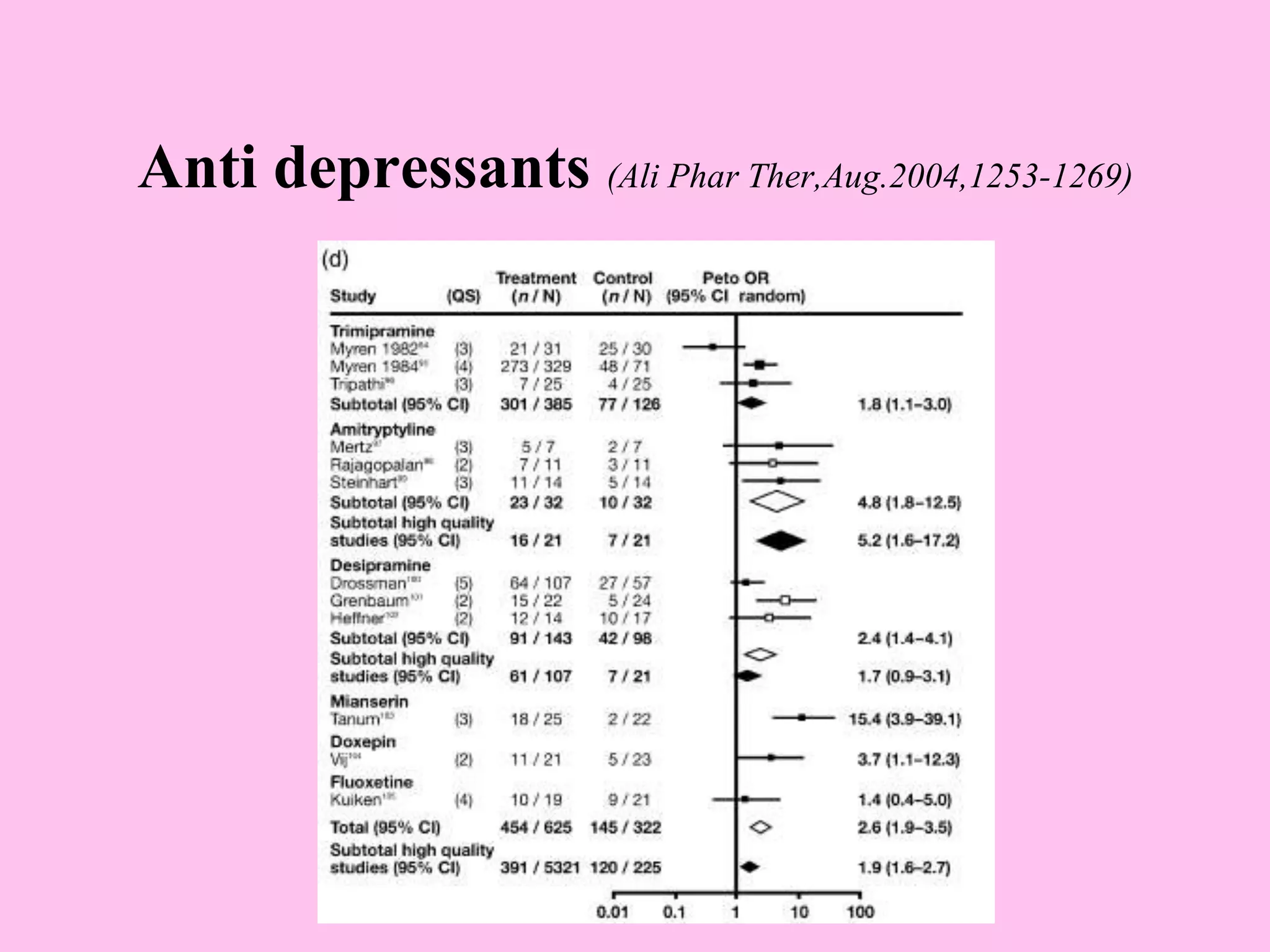
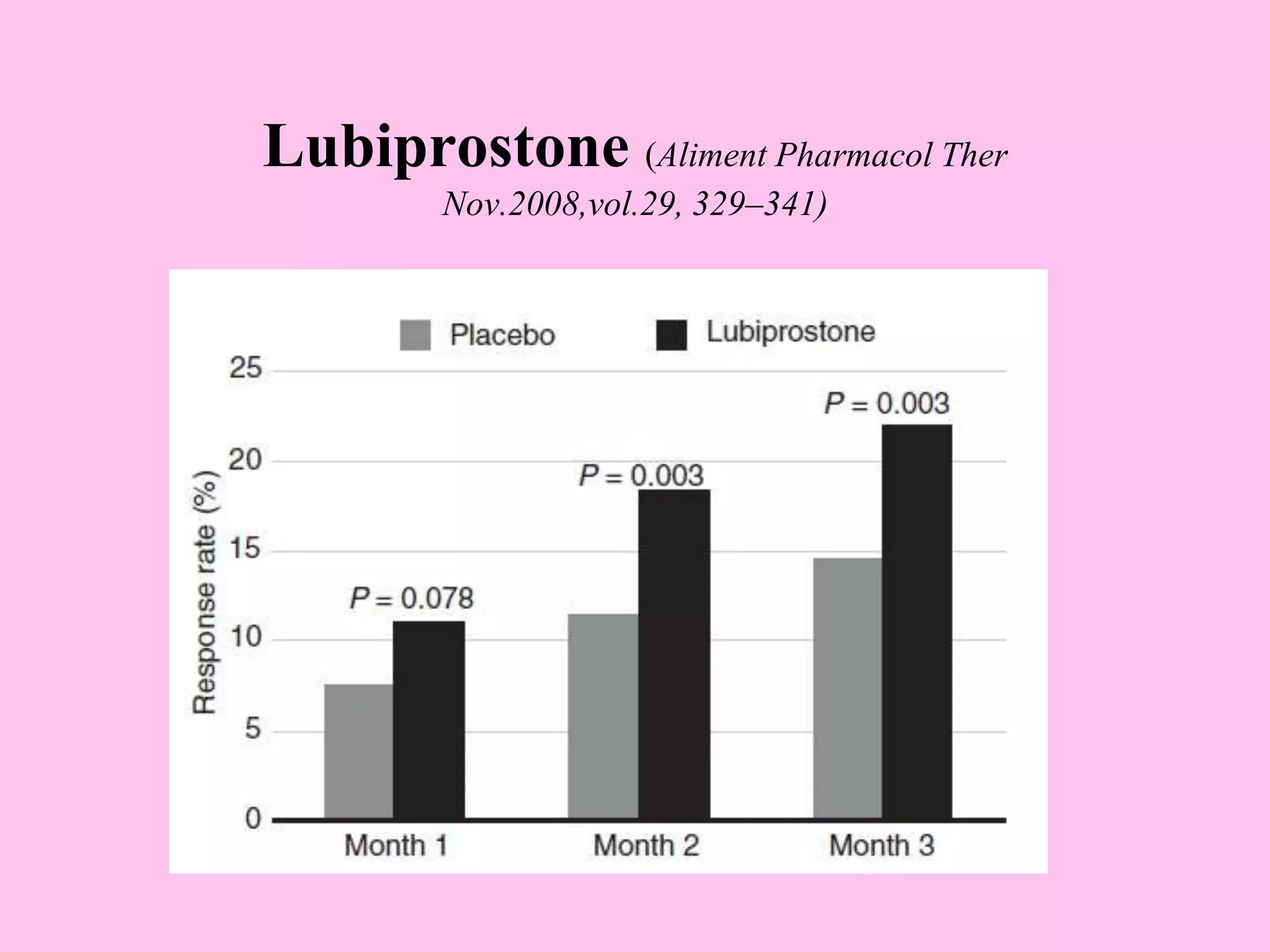
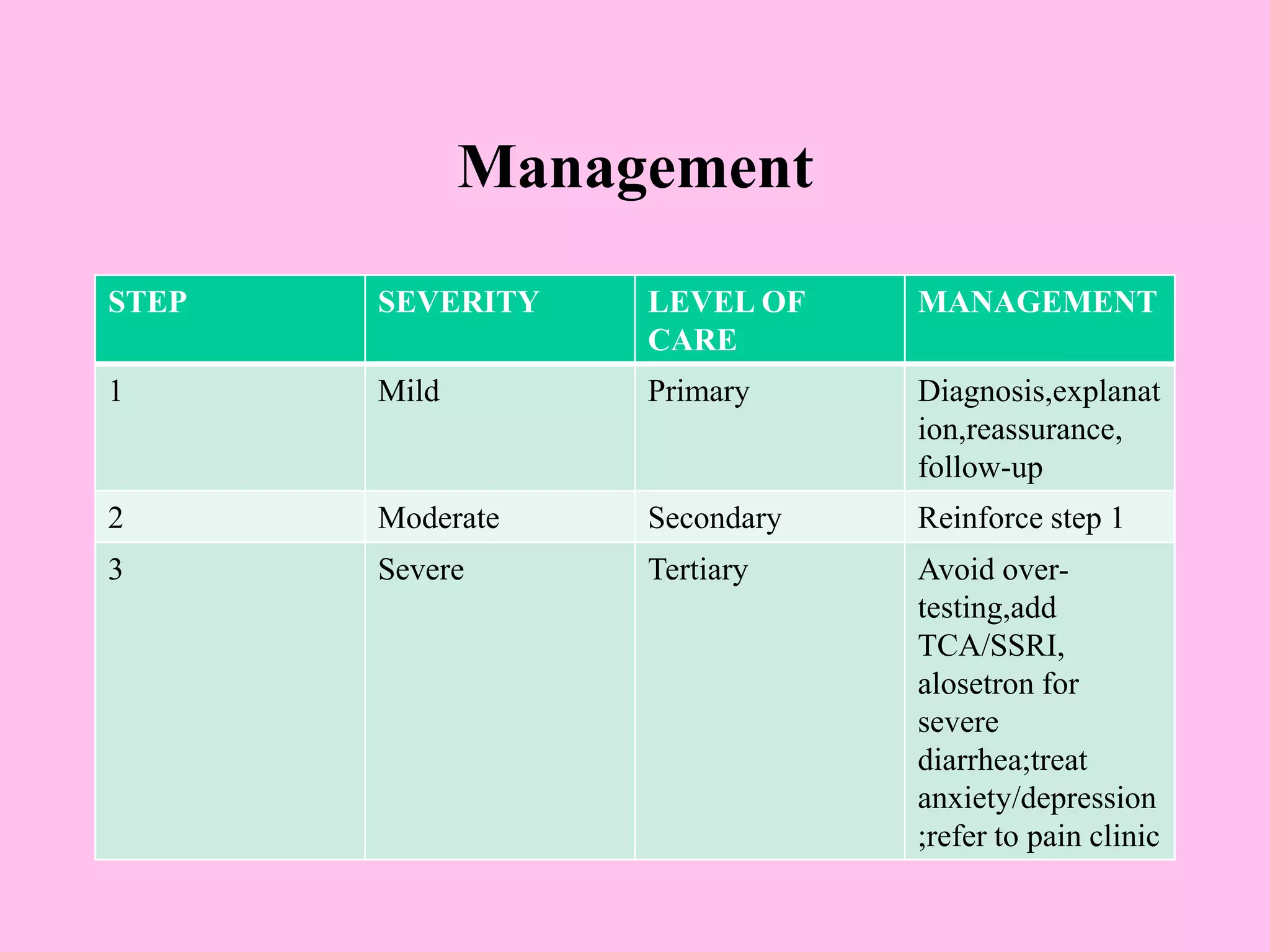
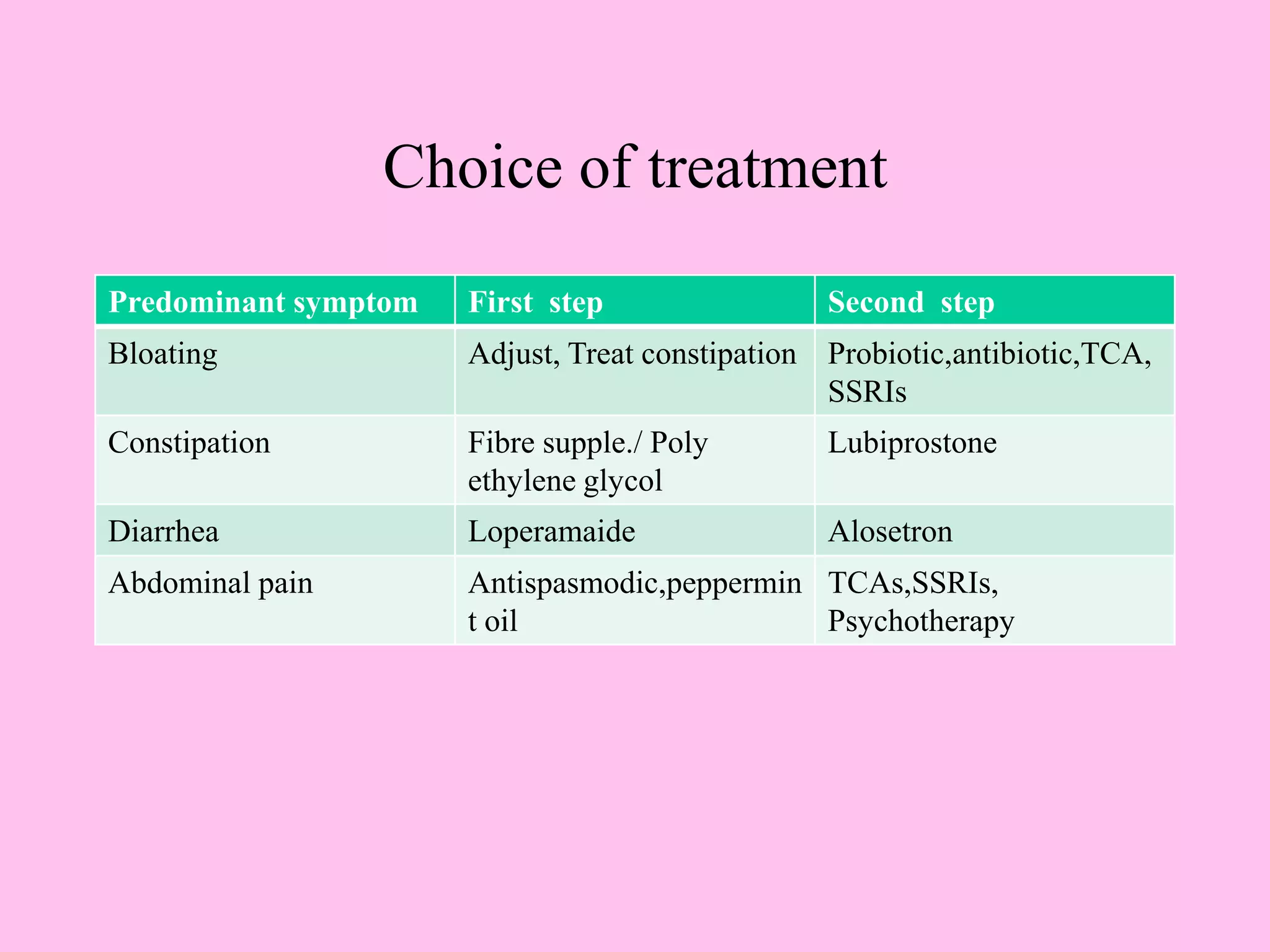
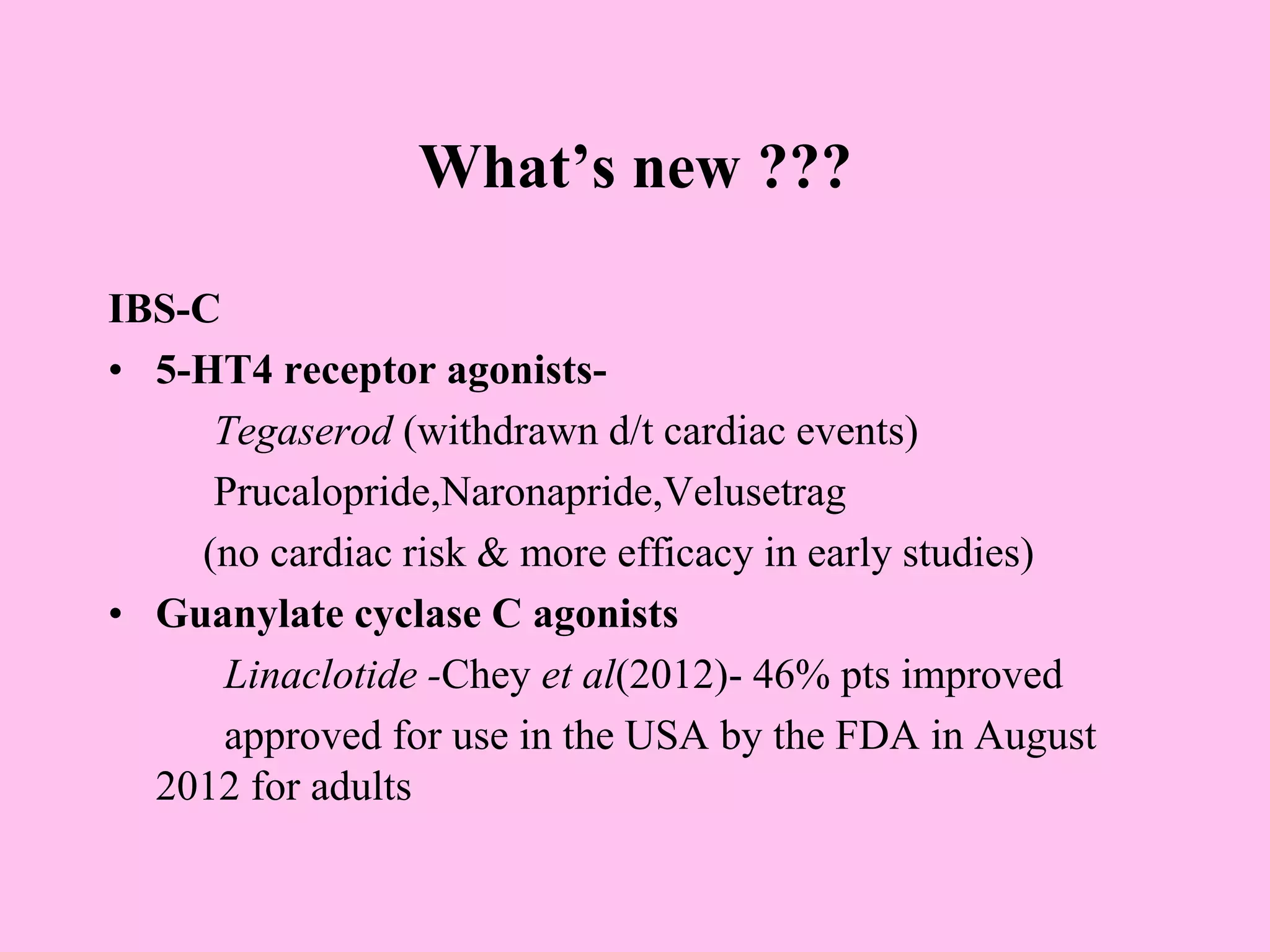
- Diagnosis is based on symptoms meeting certain criteria and exclusion of organic diseases. Management focuses on