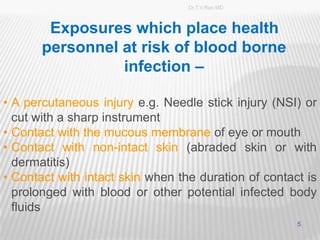
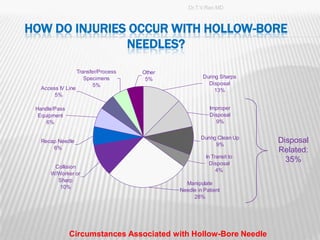
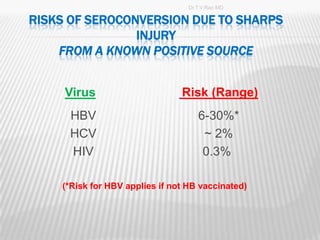
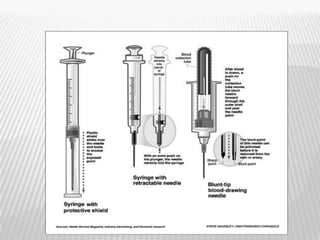
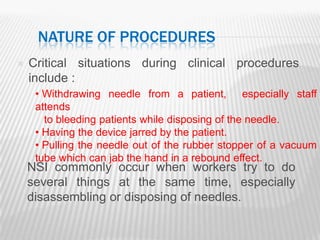
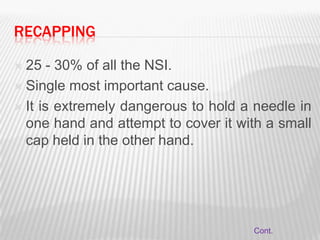
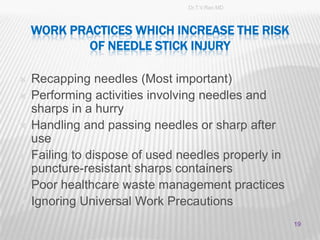
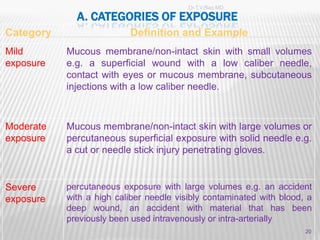
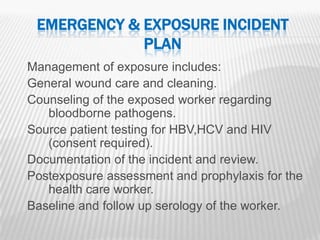
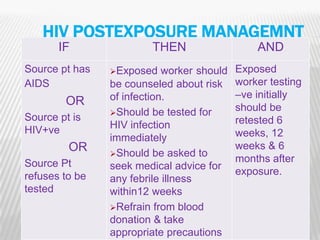
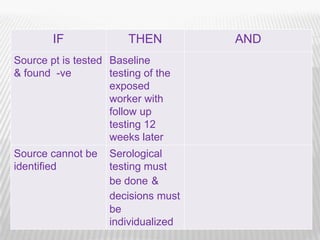
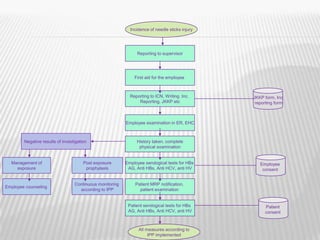
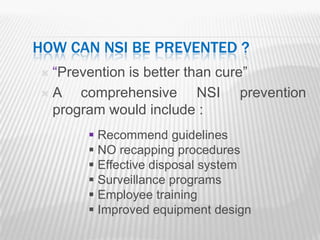
This document discusses needle stick and sharp injuries (NSI). NSI occur when needles accidentally puncture the skin, often when healthcare workers are using, disassembling, or disposing of needles. Improper disposal of needles also poses a risk. NSI can transmit bloodborne pathogens like hepatitis B, hepatitis C, and HIV. Despite training programs, NSI remain a problem. Nurses and other clinical staff are most at risk. Injuries often occur during disposal or manipulation of needles in patients. Proper handling and disposal of sharps can help prevent these injuries.