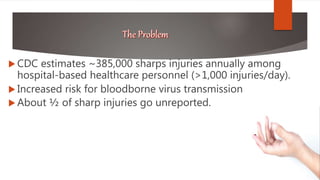
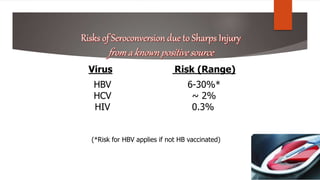
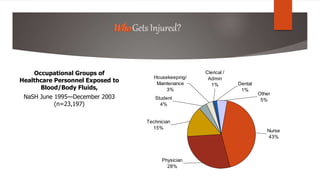
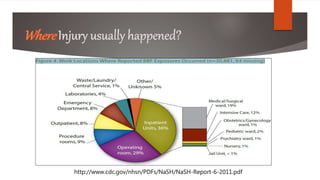
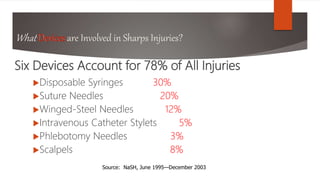
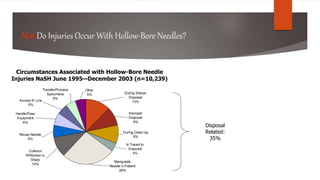
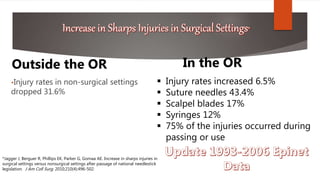
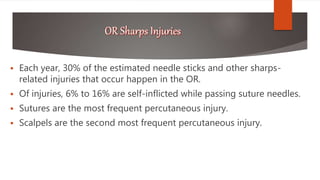
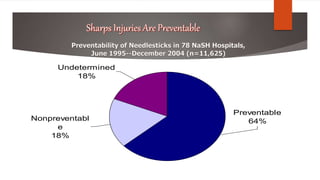
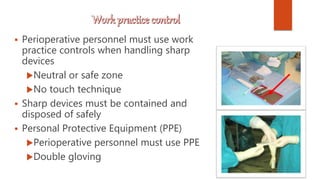
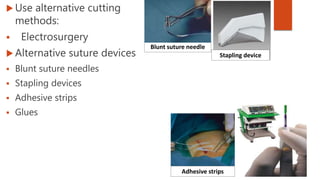
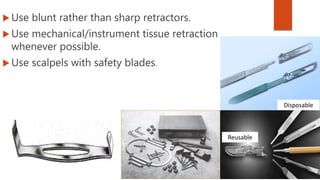
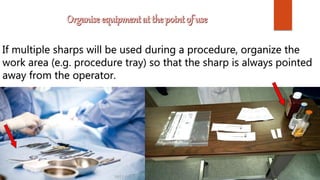
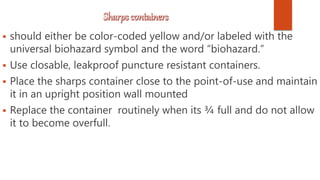
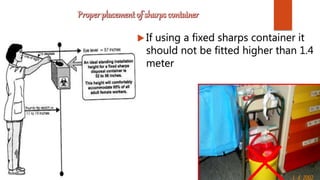
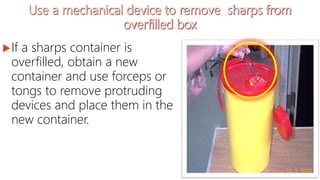
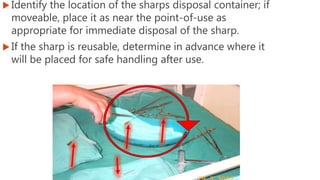
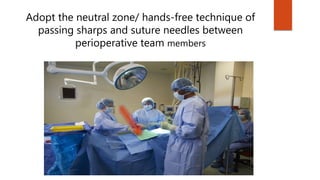
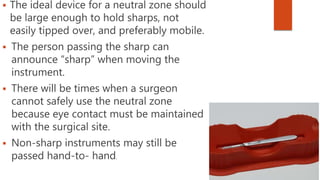
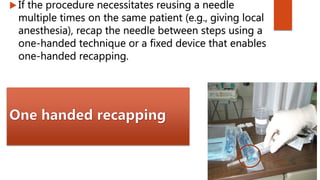
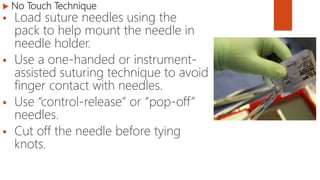
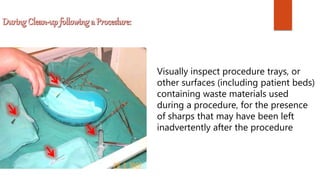
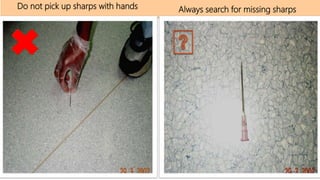
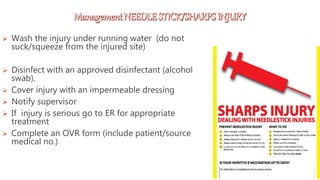
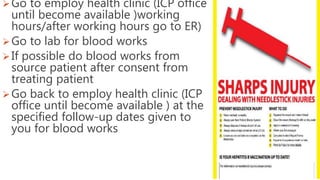
This document discusses sharps injuries among healthcare personnel and recommendations to prevent such injuries. It notes that there are an estimated 385,000 sharps injuries annually, with nurses being the occupational group most commonly exposed. The six devices that account for most injuries are disposable syringes, suture needles, winged-steel needles, intravenous catheter stylets, phlebotomy needles, and scalpels. Over a third of injuries are disposal-related. Recommendations include using safety-engineered devices, safe handling practices like neutral zones, and proper disposal in closable sharps containers.