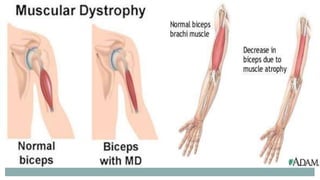
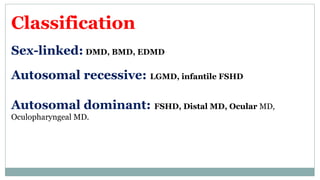
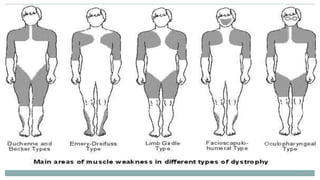
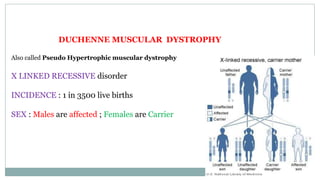
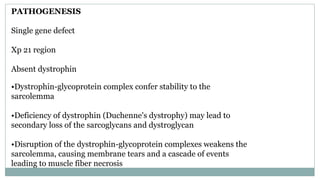
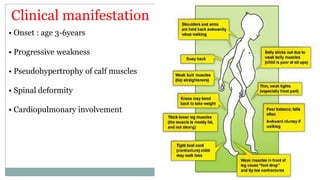
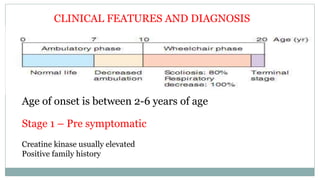
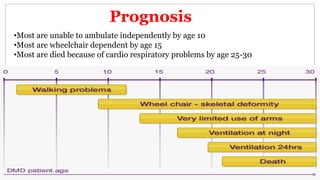
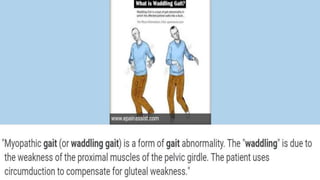
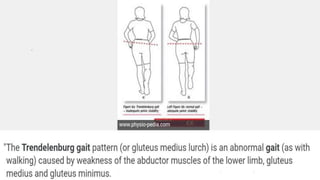
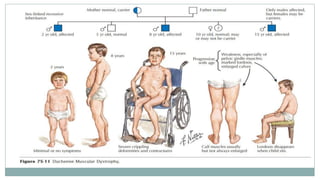
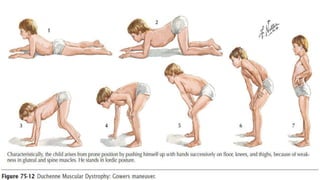
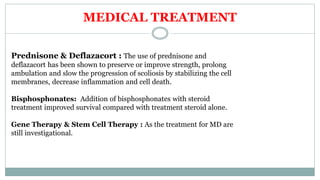
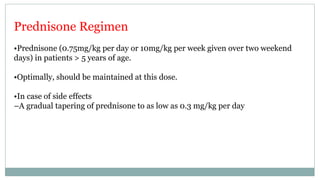
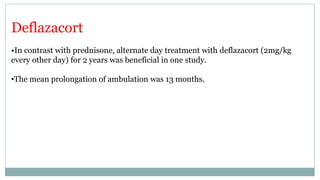
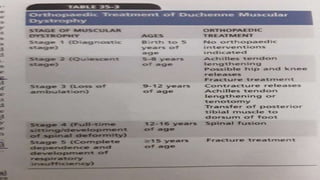
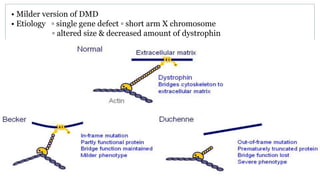
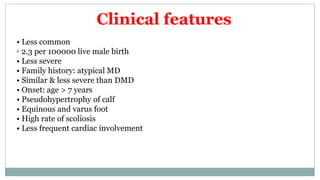
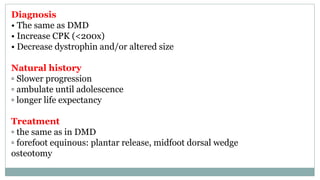
Muscular dystrophies are a group of hereditary disorders that cause progressive skeletal muscle degeneration and weakness. The document focuses on Duchenne Muscular Dystrophy (DMD), which is an X-linked recessive disorder affecting males, causing muscle weakness and deterioration. Symptoms of DMD begin in early childhood and include difficulty walking, joint contractures, and respiratory/cardiac problems. Treatment aims to preserve mobility and function, including corticosteroids, orthopedic interventions, and bracing. While currently incurable, management can prolong ambulation and improve quality of life.