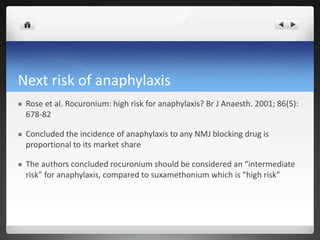
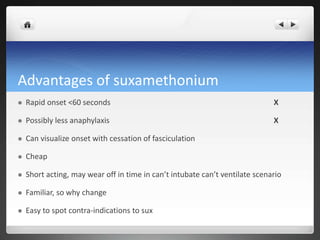
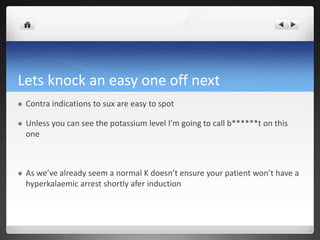
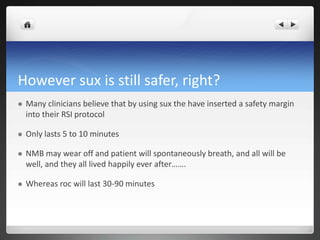
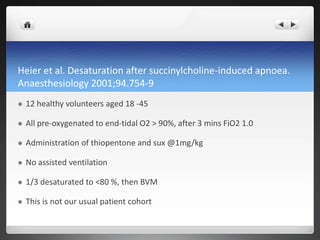
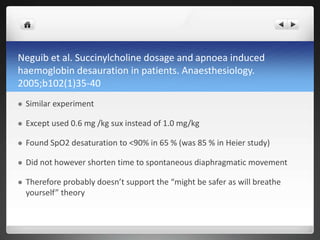
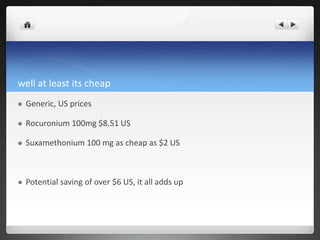
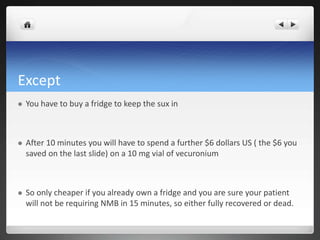
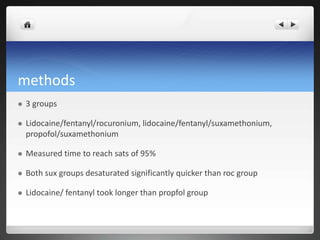
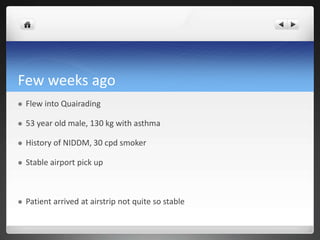
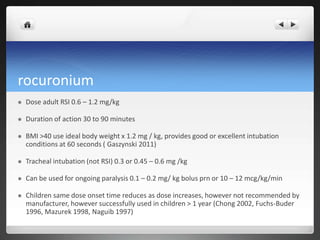
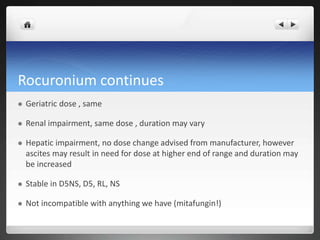
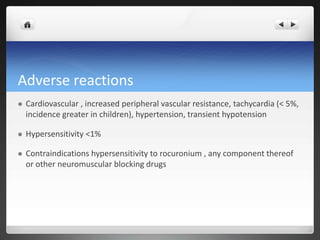
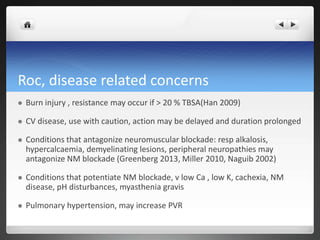
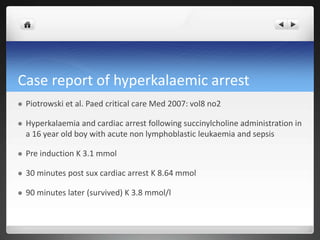
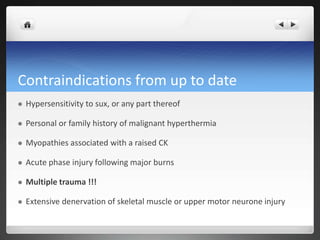
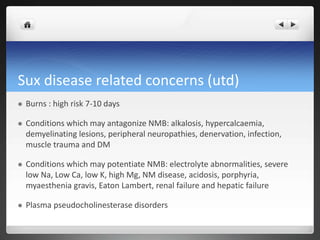
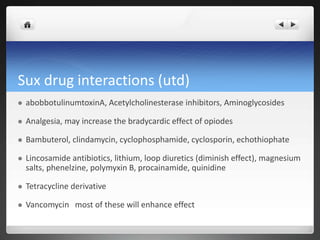
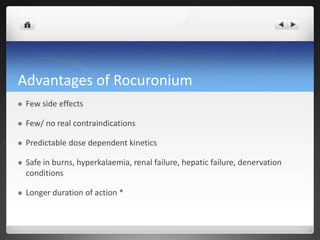
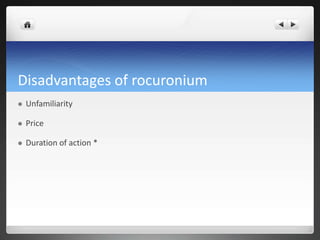
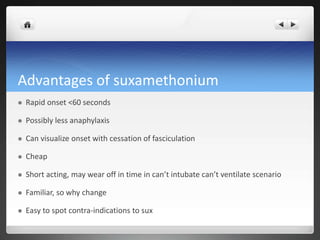
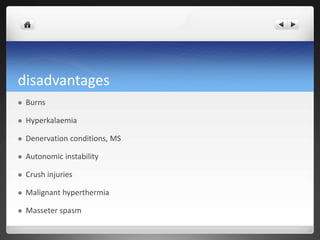
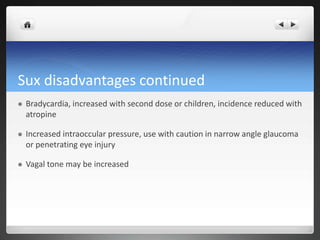
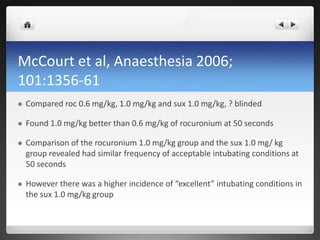
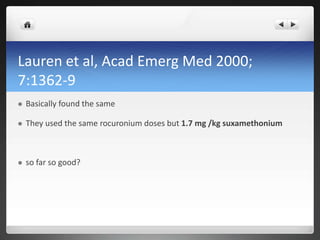
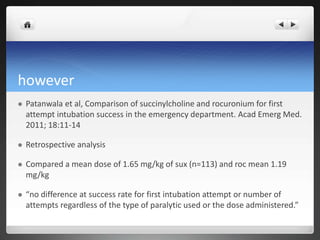
This document compares the advantages and disadvantages of rocuronium versus suxamethonium for rapid sequence induction of anesthesia in remote settings. While suxamethonium has a faster onset of less than 60 seconds, studies have shown that rocuronium at doses of 1.0-1.2 mg/kg provides comparable intubation conditions. Suxamethonium also carries significant risks like malignant hyperthermia, hyperkalemia, and prolonged desaturation during apnea. Overall, rocuronium provides predictable pharmacokinetics, fewer contraindications, and is safer for conditions like burns and muscle diseases compared to suxamethonium. Though initially cheaper, the cost savings of suxame
![Then Cochrane chipped in their 2 cents
worth in 2008
“rocuronium versus succinylcholine for rapid sequence induction”
Combined 37 studies
Concluded “no statistical difference in intubating condition when
[suxamethonium] was compared to 1.2 mg/kg of rocuronium”
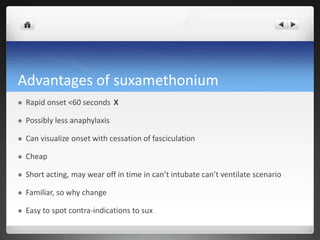
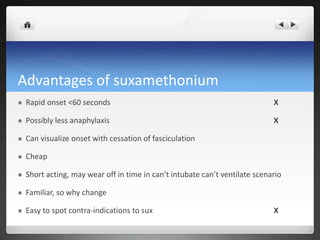
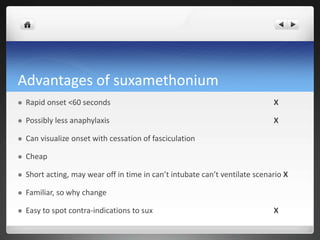
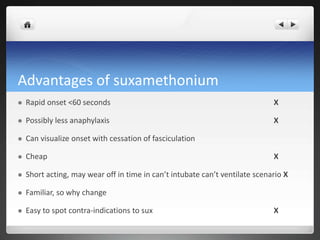
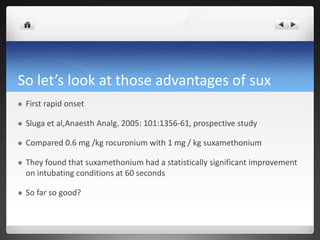
So let’s review the advantages of sux](https://image.slidesharecdn.com/musclerelaxants-151001070609-lva1-app6892/85/Muscle-relaxants-35-320.jpg)