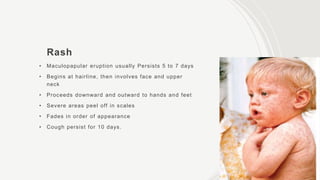
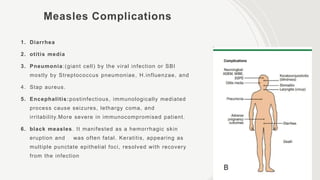
This document outlines key information about measles, including its definition, etiology, epidemiology, clinical manifestations, diagnosis, complications, treatment, and prevention methods. It describes the transmission of the disease, symptoms such as fever and rash, and emphasizes the importance of vaccination and vitamin A supplementation in preventing severe complications. The document also highlights the lack of specific treatments and the necessity for supportive care in complicated cases.