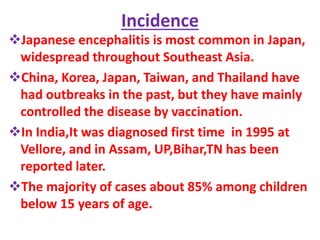
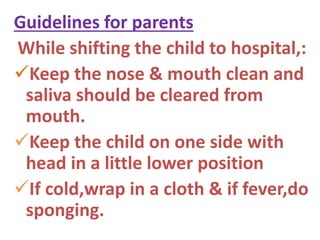
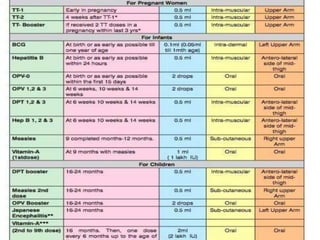
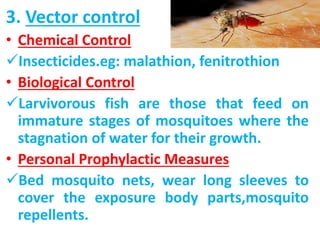
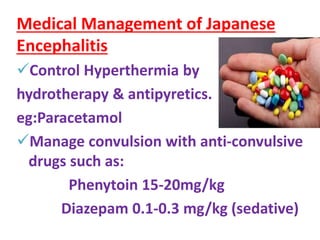
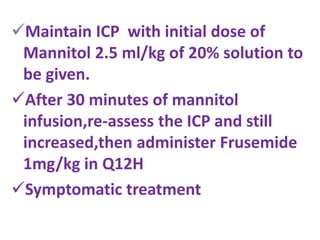
Japanese encephalitis is a mosquito-borne viral infection that causes inflammation of the brain. It is most common in parts of Asia including Japan, China, and India. The virus is transmitted via Culex mosquitoes and pigs and birds can act as reservoirs. Most cases occur in children under 15 years of age during the rainy season. Symptoms progress through prodromal, acute encephalitic, and late stages with high fever, seizures, unconsciousness, and potential long-term neurological impairment. Diagnosis involves detecting IgM antibodies or antigens in blood or CSF. Prevention focuses on vaccination programs and vector control like insecticides and larvivorous fish. Treatment involves fever control, anti-convulsants, and