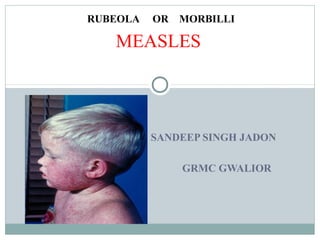
This document provides information on measles (rubeola), including its definition, epidemiology, pathogenesis, clinical manifestations, complications, diagnosis, treatment, vaccination, and prophylaxis. It describes measles as a highly contagious viral disease characterized by fever and rash. Key points include that measles virus is transmitted via respiratory droplets; the vaccine is live attenuated measles virus that provides 95% protection with two recommended doses at 12-15 months and 4-6 years of age.