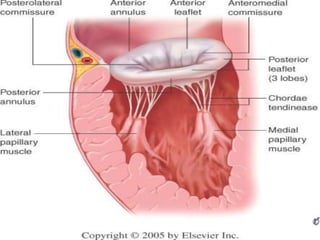
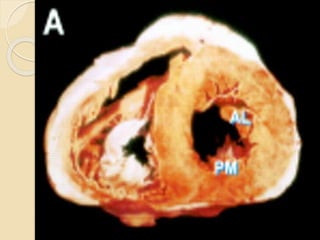
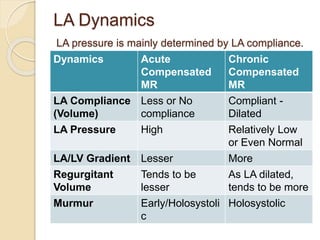
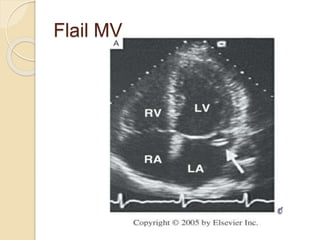
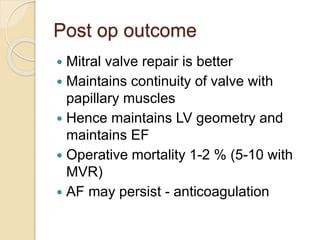
Mitral regurgitation is caused by abnormalities of the mitral valve leaflets, chordae tendineae, or annulus that prevent complete coaptation of the leaflets during systole. The main causes include degenerative diseases like mitral valve prolapse or rheumatic heart disease. Severe mitral regurgitation can lead to left atrial and ventricular dilation and dysfunction over time if left untreated. Echocardiography is the main imaging modality used to assess severity based on regurgitant jet area and velocity. Surgery is recommended for symptomatic patients or asymptomatic patients with severe regurgitation and abnormal ventricular size or function. Mitral valve repair is preferred over replacement when possible due to better long-