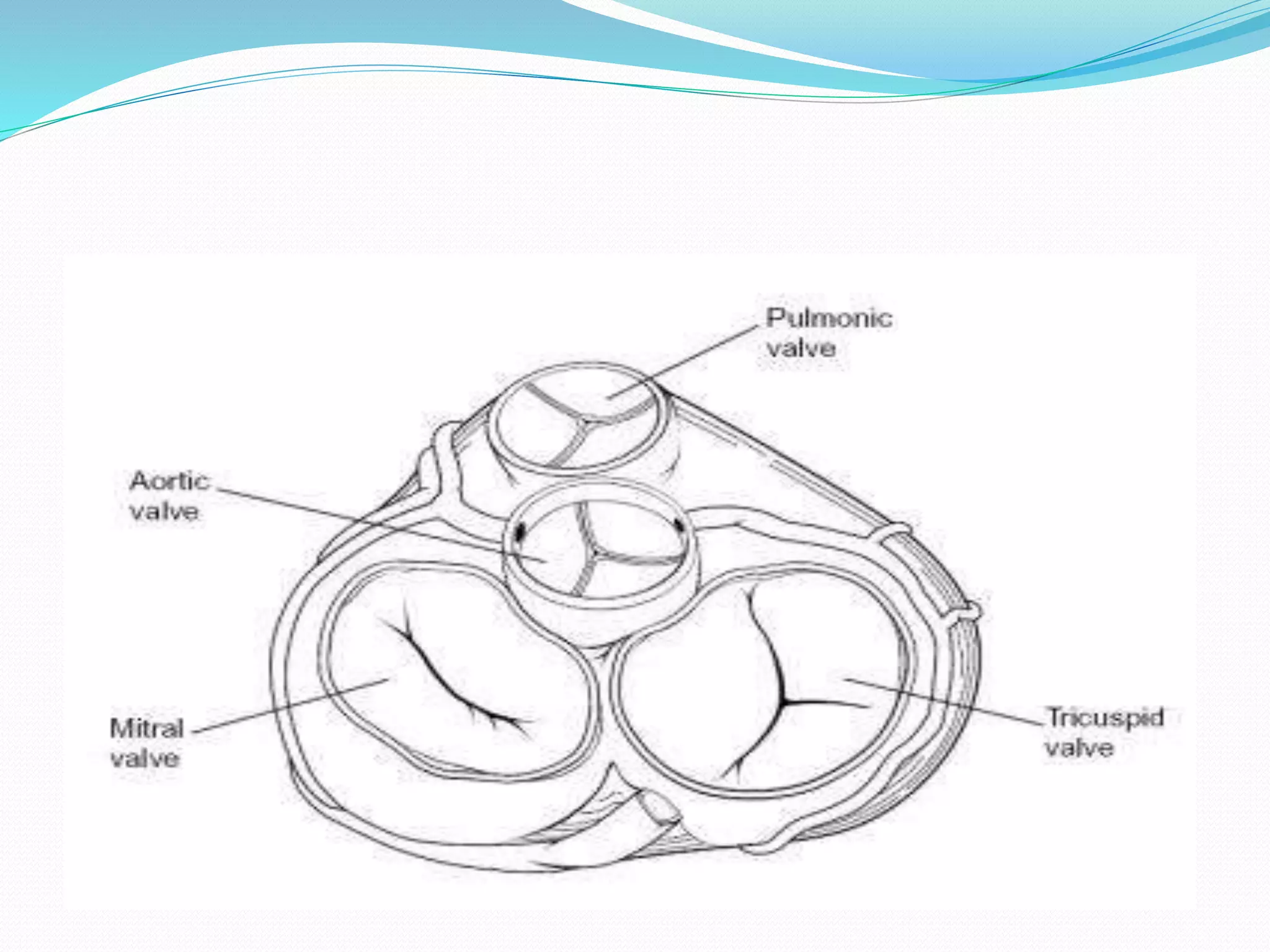
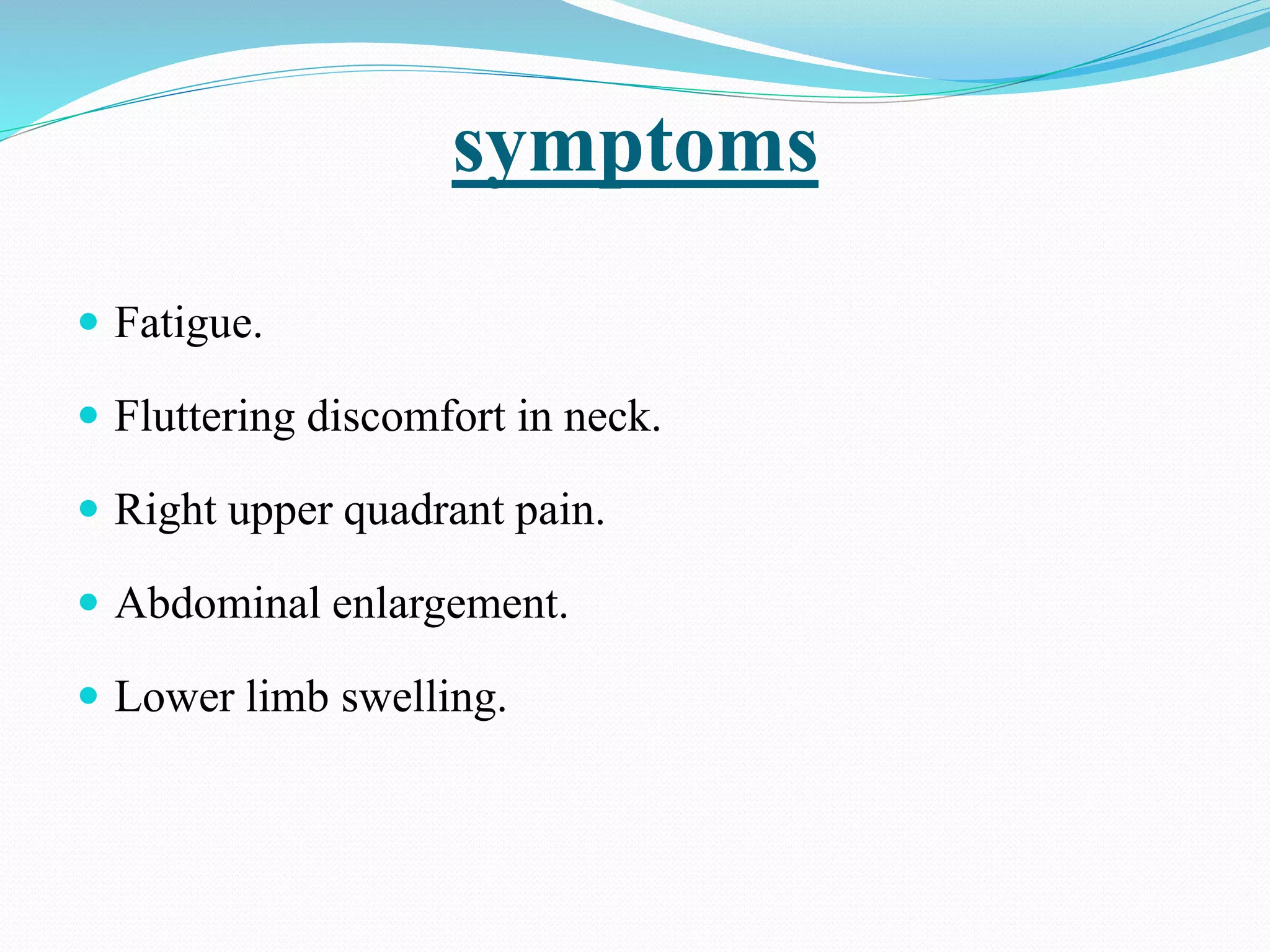
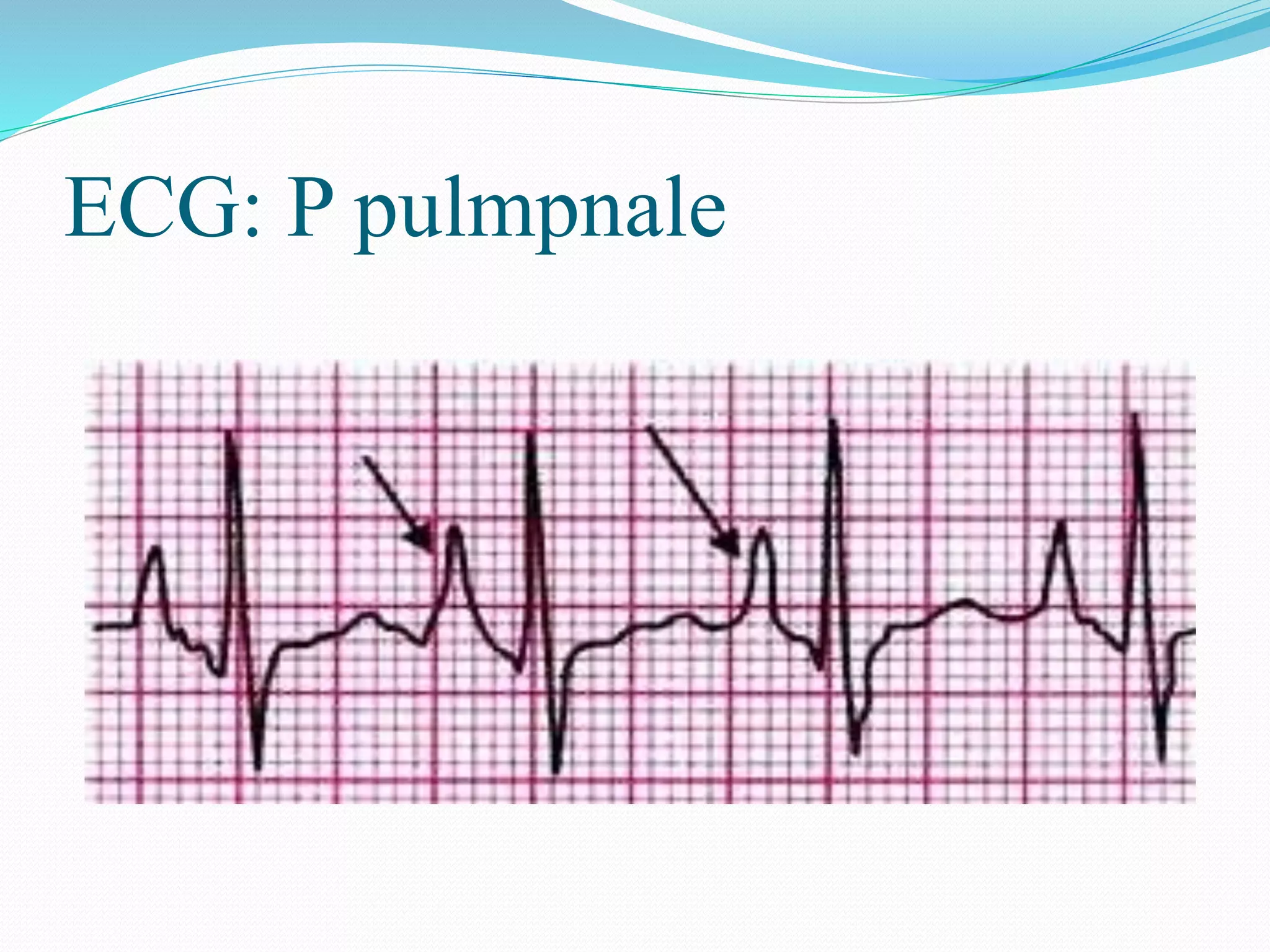
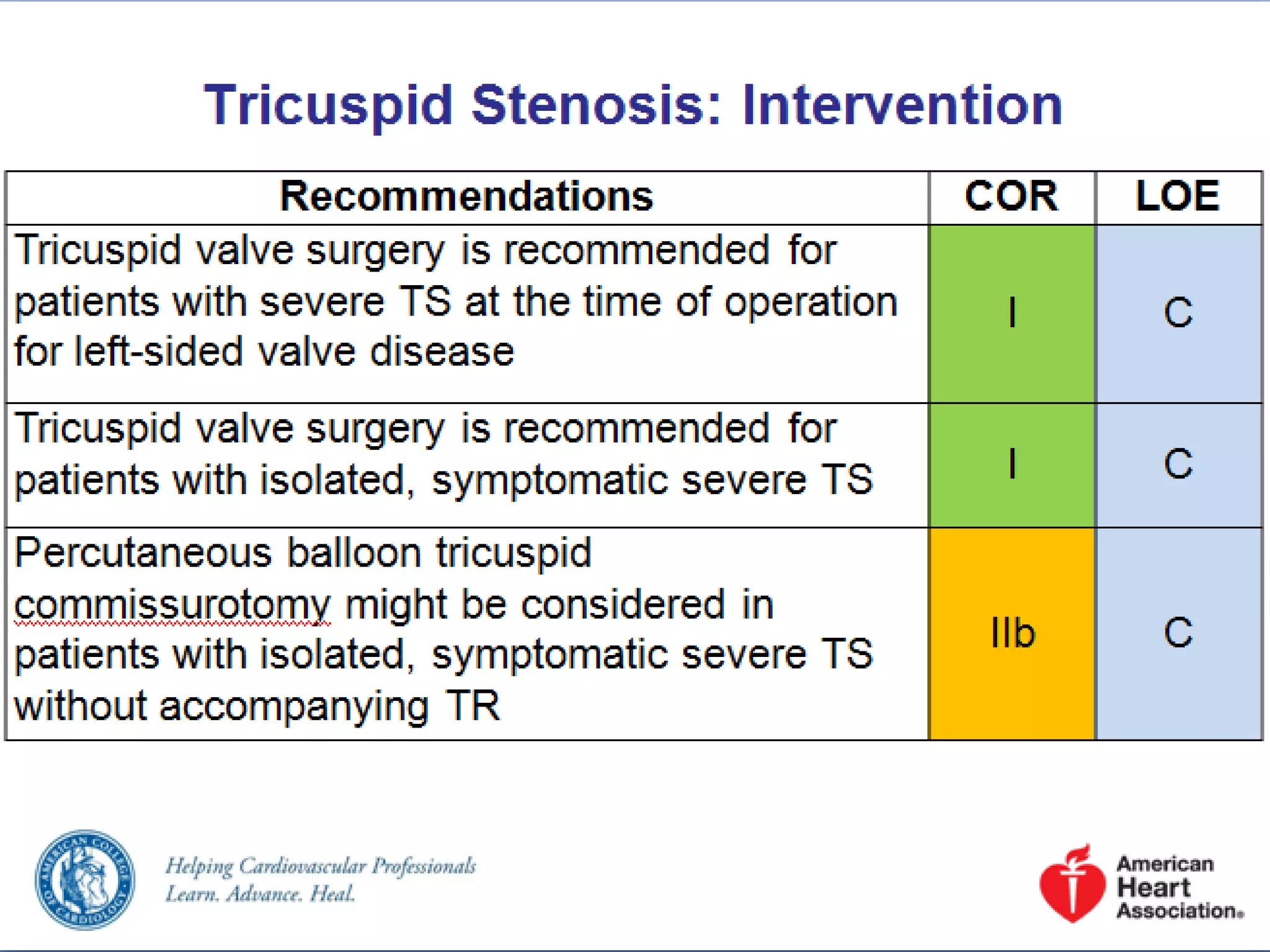
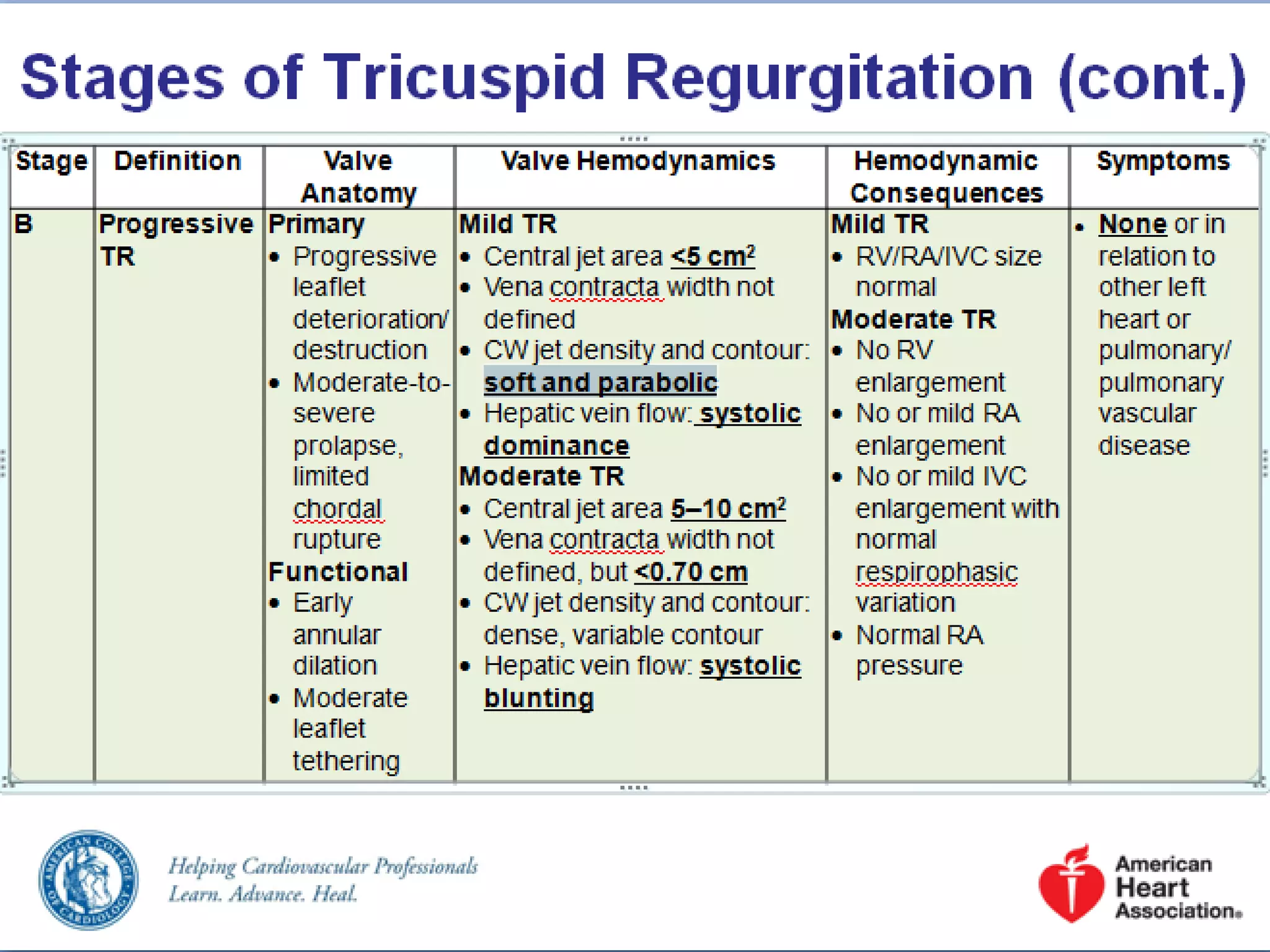
This document discusses the anatomy, assessment, and management of tricuspid valve disease. It covers tricuspid stenosis and tricuspid regurgitation. For tricuspid stenosis, the most common causes are rheumatic fever and infective endocarditis. Symptoms include fatigue and swelling. Transthoracic echocardiogram is used to assess the mean gradient and valve morphology. For tricuspid regurgitation, the most common primary causes are rheumatic fever and carcinoid heart disease. Secondary causes are related to right ventricular dilation. Symptoms are similar to stenosis. Echocardiogram can assess the severity of regurgitation and pulmonary pressures. Management involves medical therapy depending on severity of disease.