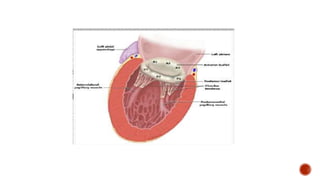
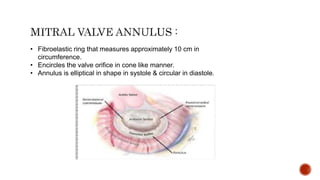
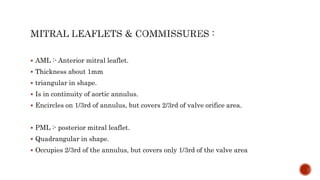
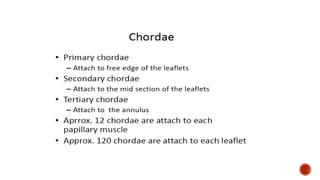
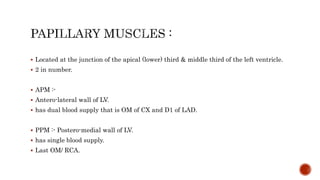
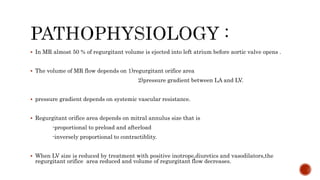
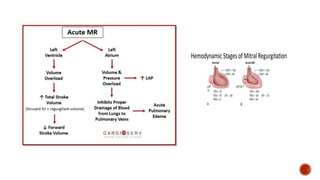
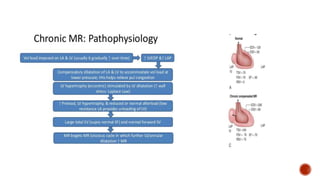
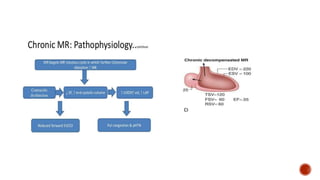
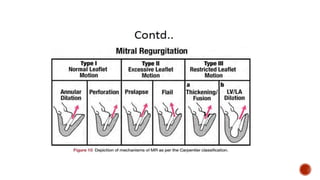
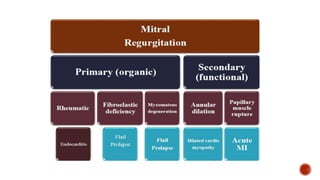
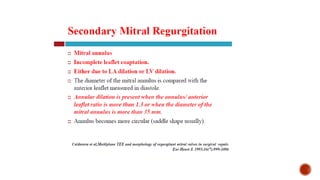
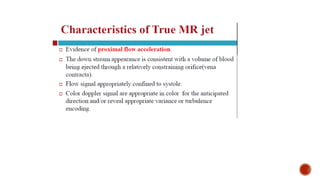
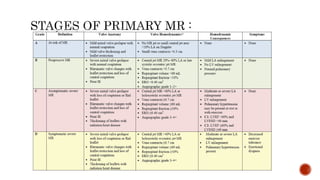
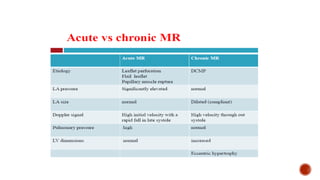
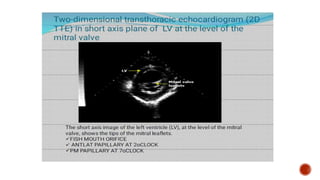
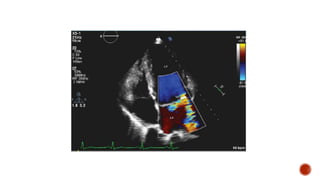
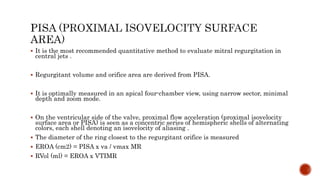
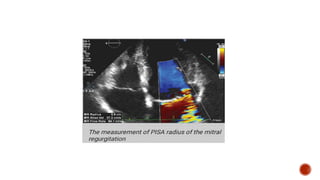
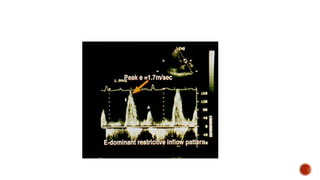
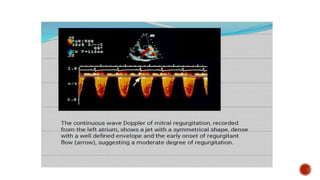
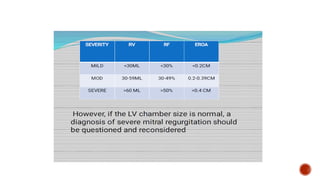
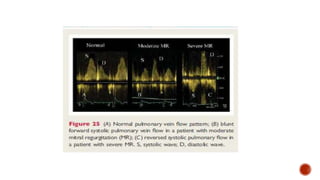
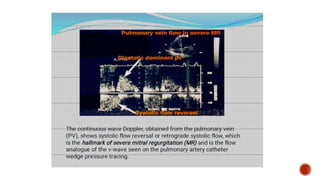
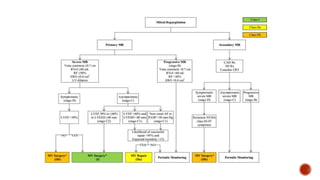
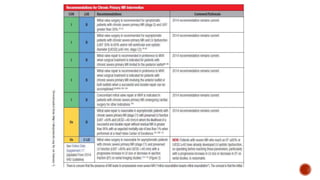
The document describes the anatomy and physiology of the mitral valve complex. It consists of the mitral valve annulus, two leaflets, chordae tendineae, and papillary muscles. Color Doppler and pulsed wave Doppler are used to assess mitral regurgitation. Severe chronic mitral regurgitation is associated with left atrial and left ventricular enlargement and abnormalities of the mitral apparatus. Proximal isovelocity surface area method using Doppler is the most recommended way to quantify central mitral regurgitation jets.