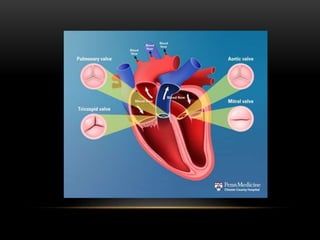
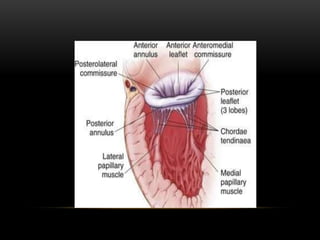
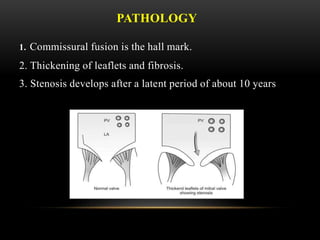
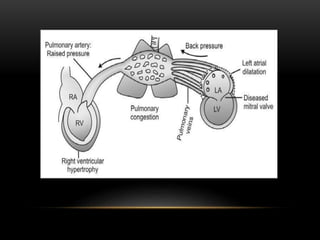
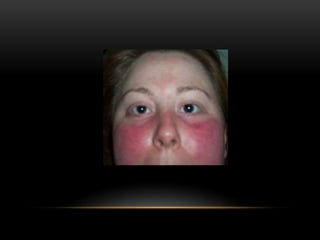
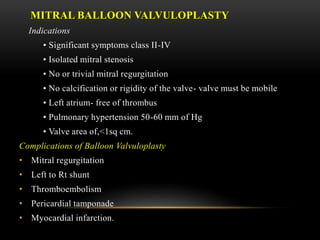
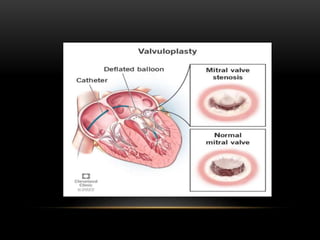
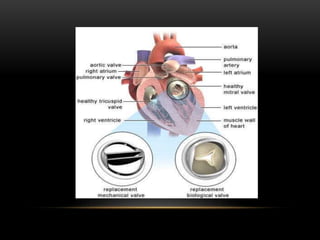
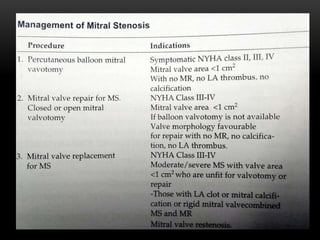
Mitral stenosis is a condition characterized by the narrowing of the mitral valve, commonly caused by rheumatic heart disease, leading to significant hemodynamic changes and clinical symptoms such as dyspnea and palpitations. Diagnosis involves auscultation revealing characteristic murmurs, echocardiography for severity assessment, and other imaging techniques, while treatments include medical management and interventions like balloon valvuloplasty or surgical options based on valve condition and patient symptoms. Complications can arise from both the valve condition and treatment interventions, necessitating careful monitoring and management.