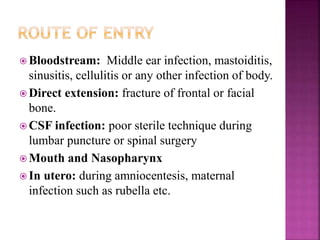
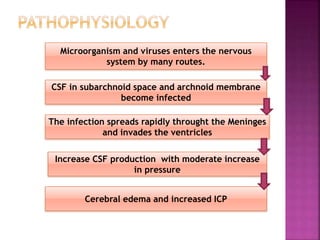
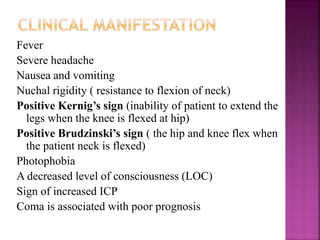
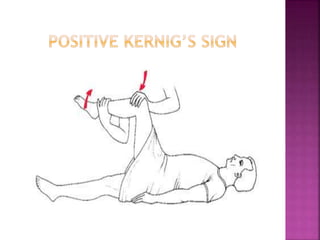
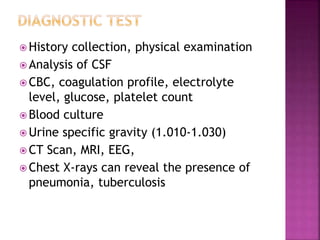
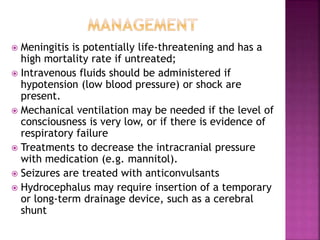
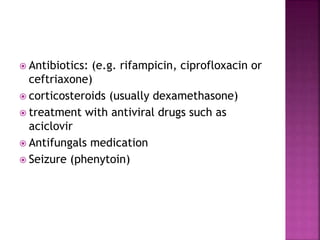
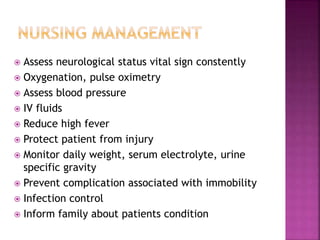
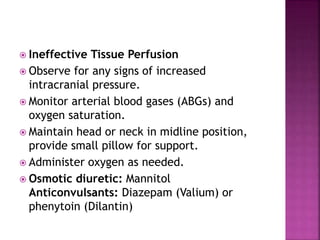
Meningitis is an inflammation of the meninges that covers the brain and spinal cord. It is usually caused by viral or bacterial infections, though fungi, drugs, and cancer can also cause meningitis. Symptoms include fever, headache, nausea, and neck stiffness. Diagnosis involves spinal fluid analysis, imaging, and culture tests. Treatment focuses on antibiotics, antivirals, or antifungals depending on cause, with supportive care like IV fluids and fever control. Complications can be serious if untreated and include long term neurological deficits.