This document provides an overview of abdominal trauma, including:
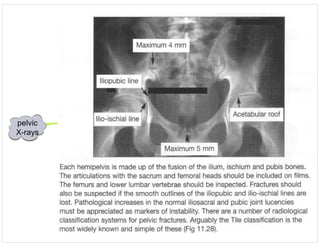
1) Initial assessment involves imaging like CXR, pelvis X-ray, and neck X-ray to identify injuries. Resuscitation focuses on airway, breathing, circulation, disability, and environment.
2) Further assessment includes inspection, palpation, FAST ultrasound, and CT scan. Blunt trauma most commonly injures the spleen and liver while penetrating trauma often injures the small intestine, liver, and colon.
3) Surgical intervention is usually required for gunshot wounds while most blunt solid organ injuries can now be managed non-operatively. Diagnostic peritoneal lavage can identify bleeding but does not locate the source.

![abdominal trauma
- assessment
[created by Paul
Young 28/10/07]
initial
assessment
imaging and
laboratory
studies
definitiontrauma series:
- CXR identifies haemothorax, pneumothorax and pulmonary contusion
- AP pelvis can confirm presence of significant pelvic fracture
- lateral c-spine can identify non-survivable neck injury
resuscitation &
comprehensive
assessment
Primary survey:
(i) Airway(ability of air to pass unobstructed to the lungs):
critical findings include:
- obstruction of the airway due to direct injury, oedema, foreign body or inability
to protect the airway because of depressed level of consciousnesss
key treatment is:
- establishment of airway
(ii) Breathing (ability to ventilate and oxygenate):
key clinical findings are:
- absence of spontaneous ventilation, absent or asymmetrical breath sounds, dyspnoea
hyperresonance, dullness, gross chest wall instability or defects that compromise ventilation
key conditions to identify are:
- pneumothorax, endotracheal tube malposition, tension
pneumothorax, haemothorax, sucking chest wounds, flail chest
key treatment is:
- chest tube
(iii) Circulation:
key clinical findings are:
- collapsed or distended neck veins, signs or tamponade, external sites of haemorrhage
key conditions identified are:
- hypovolaemia, cardiac tamponade, external haemorrhage
key treatment is:
- iv access, fluid resuscitation, compression of sites of bleeding
(iv) Disability:
key clinical conditions are:
- decreased level of consciousness, pupillary assymetry, gross weakness
key conditions identified are:
- serious head and spinal cord injury
key treatment is:
- definitive airway if indicated, emergency treatment of raised icp
(v) Exposure and control of immediate environment:
- expose patient and prevent hypothermia
Resuscitation phase:
- continues throughout primary and secondary survey and until treatments are complete
- fluids are required to sustain intravascular volume, tissue and organ perfusion and urine output
- administer blood for hypovolaemia that is unresponsive to crystalloid boluses
- end points are normal vital signs, absence of blood loss, adequate urine output and no evidence of end
organ dysfunction; blood lactate and base deficit on an ABG may be helpful in patients who are severely injured
Other procedures:
several monitoring and diagnostic adjuncts occur in concert with the primary survey:
(i) ECG and ventilatory monitoring and continous pulse oximetry
(ii) decompress stomach with NG or OG tube once airway is secured
(iii) insert a foley cather during resuscitation phase (foley catheter placement is contraindicated
if urethral injury is evident as identified by blood at the meatus, ecchymosis or scrotum or
labium majora or high riding prostate - retrograde urethrogram is required for these patients)
Secondary survey of abdominal trauma:
(i) inspection:
- examine for the presence of external signs of injury noting patterns of abrasion and/or ecchymotic areas
- lap belt bruising is positively correlated with rupture of the small intestine and increased incidence of other
intraabdominal injury (20-30% of patients with lap-belt marks have associated mesenteric or intestinal injuries)
- bradycardia may indicate free intraperitoneal blood
- Cullen sign (periumbillical ecchymosis) may indicate retroperitoneal
haemorrhage; however, this usually takes hours to develop
- flank bruising and swelling may raise suspicion for retroperitoneal injury
- inspect genitals and peritoneum
(ii) palpation:
- fullness may indicate haemorrhage
- crepitation of lower rib cage may indicate hepatic or splenic injury
- rectal and vaginal examination identify potential bleeding and injury
- signs of peritonitis soon after injury suggest leakage of intestinal contents;
peritonitis due to intra-abdominal haemorrhage may take several hours to develop
FAST:
- used to identify free fluid in the peritoneal cavity
- FAST has a sensitivity of 70-95%
- involves directing to ultrasound probe in four regions:
(i) the subxipoid location to determine whether there is fluid in the pericardial
space & to make a rough assessment of contractility & filling state
(ii) the right upper quadrant
(iii) the splenorenal recess
(iv) the pelvis
- problems with FAST:
(i) operator dependent
(ii) false negative rate in children is high
(iii) technically more difficult with obesity & sc empysema
CT abdo/pelvis:
- is the diagnostic modality of choice for haemodynamically stable patients
- the major reason not to obtain a CT scan is haemodynamic instability
- allows haemoperitoneum & its source to be identified & allows specific injuries to be graded
- CT also permits evaluation of retroperitoneal structures including the kidneys, major blood vessels & bony pelvis
- the majority of blunt solid organ injuries are now managed non-operatively in trauma centres; however, a
blush of intravenous contrast agent indicates active extravasation from a bleeding vessel and is strong predictor
of failure of non-operative management
- problems with CT scanning are:
(i) the need to transfer the patient to radiology
(ii) the time associated with transfer and scanning
(iii) risks associated with intravenous contrast agents
(iv) the fact hollow viscus, diaphragmatic & pancreatic injuries are frequently missed on initial scanning
abdominal trauma consists of blunt and penetrating trauma
Penetrating abdominal trauma:
- most commonly injured organs with stab wounds are small intestine, liver and colon
- only one third of abdominal stab wounds penetrate the peritoneum & only 50% of
these require surgical intervention
- 85% of abdominal wall gun shot wounds penetrate the peritoneum & 95% of these
require a surgical procedure for correction
Blunt abdominal trauma
- spleen and liver are the most commonly injured organs; small and large intestines are the next most commonly injured
DPL:
- has an accuracy of 98% for detection of haemoperitoneum but does not determine source
- generally performed in patients too unstable for CT
- involves performing a minilaparotomy with placement of a lavage catheter into the periotoneal
cavity directed towards the pelvis
- the return of gross blood is a positive result
- if DPL is grossly negative then 1L of warmed saline is instilled into the the abdominal cavity &
then drained back into the intravenous fluid bag by gravity. The effluent lavage is sent to the
laboratory for analysis.
- laboratory criteria for a positive DPL in blunt trauma are:
(i) >100000 RBCs/mm3
(ii) >500 WBC/mm3
(iii) presence of food particles
(iv) presence of bile
(v) presence of bacteria
- problems with DPL:
(i) an invasive procedure
(ii) 1/4 of patients with a positive DPL will have a non-therapeutic laparotomy
(iii) 5% false negative rate with retroperitoneal, hollow viscus or diaphragm injuries
- ongoing haemorrhage is the most likely cause of persistent or recurrent haemodynamic instability
- initial goal is not to diagnose specific abdominal organ injury but rather to determine wheter there are
signs & symptoms that indicate a need for immediate laparotomy
30% of patients with lumbar Chance fracture have associated bowel or mesenteric injuries
criteria
for
positive
DPL](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-2-320.jpg)



![acidosis
in kidney
disease
[created
by Paul
15/12/07]
Distal
(Type 1)
Renal
Tubular
Acidosis
General
- This is also referred to as classic RTA or distal RTA.
- The problem here is an inability to maximally acidify the urine. Typically
urine pH remains > 5.5 despite severe acidaemia ([HCO3] < 15 mmol/l).
- Some patients with less severe acidosis require acid loading tests
(eg with NH4Cl) to assist in the diagnosis. If the acid load drops the
plasma [HCO3] but the urine pH remains > 5.5, this establishes the diagnosis.
General Classification of Causes of type 1 RTA
(i)Hereditary (genetic)
(ii) Autoimminue diseases (eg Sjogren's syndrome, SLE, thyroiditis)
(iii) Disorders which cause nephrocalcinosis (eg primary hyperparathyroidism, vitamin D intoxication)
(iv) Drugs or toxins (eg amphotericin B, toluene inhalation)
(v) Miscellaneous - other renal disorders (eg obstructive uropathy)
Pathophysiological Mechanisms in Reduced H+ Secretion in Distal Tubule
(i) "Weak pump"
- Inability for H+ pump to pump against a high H+ gradient
(ii) "Leaky membrane"
- Back-diffusion of H+ [eg This occurs in RTA due amphotericin B]
(iii) "Low pump capacity"
- Insufficient distal H+ pumping capacity due to tubular damage.
Investigation
- Typical findings are an inappropriately high urine pH (usually > 5.5), low acid secretion
and urinary bicarbonate excretion despite severe acidosis. Renal sodium wasting is
common and results in depletion of ECF volume and secondary hyperaldosteronism with
increased loss of K+ in the urine.
- The diagnosis of type 1 RTA is suggested by finding a hyperchloraemic acidosis in
association with an alkaline urine particularly if there is evidence of renal stone
formation.
Note: If [HCO3 > 15 mmol/l, then acid loading tests are required to establish the diagnosis.
Treatment
- Treatment with NaHCO3 corrects the Na+ deficit, restores the extracellular fluid volume
and results in correction of the hypokalaemia. Typical alkali requirements are in the range
of 1 to 4 mmol/kg/day. K+ supplements are only rarely required. Sodium and potassium
citrate solutions can be useful particularly if hypokalaemia is present. Citrate will bind
Ca++ in the urine and this assists in preventing renal stones.
Proximal
(Type 2)
Renal
Tubular
Acidosis
General
- Type 2 RTA is also called proximal RTA because the main problem is greatly impaired
reabsorption of bicarbonate in the proximal tubule.
- At normal plasma [HCO3], more than 15% of the filtered HCO3 load is excreted in the
urine. When acidosis is severe and HCO3 levels are low (eg <17 mmols/l), the urine may
become bicarbonate free.
Features
- Symptoms are precipitated by an increase in plasma [HCO3]. The defective proximal
tubule cannot reabsorb the increased filtered load and the distal delivery of bicarbonate is
greatly increased. The H+ secretion in the distal tubule is now overwhelmed by
attempting to reabsorb bicarbonate and the net acid excretion decreases. This results in
urinary loss of HCO3 resulting in systemic acidosis with inappropriately high urine pH.
The bicarbonate is replaced in the circulation by Cl-.
- The increased distal Na+ delivery results in hyperaldosteronism with consequent renal
K+ wasting. The hypokalaemia may be severe in some cases but as hypokalaemia inhibits
adrenal aldosterone secretion, this often limits the severity of the hypokalaemia.
- Hypercalciuria does not occur and this type of RTA is not associated with renal stones.
- During the NH4Cl loading test, urine pH will drop below 5.5.
- Note that the acidosis in proximal RTA is usually not as severe as in distal RTA and the
plasma [HCO3] is typically greater than 15 mmol/l.
Causes
- There are many causes but most are associated with multiple proximal tubular defects
eg affecting reabsorption of glucose, phosphate and amino acids. Some cases are hereditary.
- Causes include vitamin D deficiency, cystinosis, lead nephropathy, amyloidosis and
medullary cystic disease.
Treatment
- Treatment is directed towards the underlying disorder if possible.
- Alkali therapy (NaHCO3) and supplemental K+ is not always necessary. If alkali
therapy is required, the dose is usually large (up to 10 mmols/kg/day) because of the
increased urine bicarbonate wasting associated with normal plasma levels.
- K+ loss is much increased in treated patients and supplementation is required.
- Some patients respond to thiazide diuretics which cause slight volume contraction and
this results in increased proximal bicarbonate reabsorption so less bicarbonate is needed.
Type 3
Renal
Tubular
Acidosis
- This term is no longer used.
- Type 3 RTA is now considered a subtype of Type 1 where there is
a proximal bicarbonate leak in addition to a distal acidification defect.
Type 4
Renal
Tubular
Acidosis
General
- A number of different conditions have been associated with this type but most patients
have renal failure associated with disorders affecting the renal interstitium and tubules. In
contrast to uraemic acidosis, the GFR is greater than 20 mls/min.
- a useful differentiating point is that hyperkalaemia occurs in type 4 RTA (but
NOT in the other types).
Pathophysiology
- The underlying defect is impairment of cation-exchange in the distal tubule with
reduced secretion of both H+ and K+.
- This is a similar finding to what occurs with aldosterone deficiency and type 4 RTA can
occur with Addison's disease or following bilateral adrenalectomy.
- Acidosis is not common with aldosterone deficiency alone but requires some degree of
associated renal damage (nephron loss) esp affecting the distal tubule.
- The H+ pump in the tubules is not abnormal so patients with this disorder are able to
decrease urine pH to < 5.5 in response to the acidosis.
comparison
of RTA types
uraemic
acidosis
- The acidosis occurring in uraemic patients is due to failure of excretion of acid anions (particularly
phosphate and sulphate) because of the decreased number of nephrons. There is a major decrease
in the number of tubule cells which can produce ammonia and this contributes to uraemic acidosis.
- Serious acidosis does not occur until the GFR has decreased to about 20 mls/min. This
corresponds to a creatinine level of about 0.30-0.35 mmols/l.
- The plasma bicarbonate in renal failure with acidosis is typically between 12 & 20
mmols/l. Intracellular buffering and bone buffering are important in limiting the fall in
bicarbonate. This bone buffering will cause loss of bone mineral (osteomalacia).
- Most other forms of metabolic acidosis are of relatively short duration as the patient is either treated
with resolution of the disorder or the patient dies. Uraemic acidosis is a major exception as these patients
survive with significant acidosis for many years. This long duration is the reason why loss of bone mineral
is significant in uraemic acidosis but is not a feature of other causes of metabolic acidosis.
general
- Metabolic acidosis occurs with both acute and chronic renal failure and with
other types of renal damage. The anion gap may be normal or may be elevated.
- If the renal damage affects both glomeruli and tubules, the acidosis is a high-anion
gap acidosis. It is due to failure of adequate excretion of various acid anions due to
the greatly reduced number of functioning nephrons.
- If the renal damage predominantly affects the tubules with minimal glomerular damage,
a different type of acidosis may occur. This is called Renal Tubular Acidosis (RTA) and
this is a normal anion gap or hyperchloraemic type of acidosis. The GFR may be normal
or only minimally affected.
- Renal tubular acidosis is a form of hyperchloraemic metabolic acidosis which occurs
when the renal damage primarily affects tubular function without much effect on
glomerular function. The result is a decrease in H+ excretion which is greater than can be
explained by any change in GFR. If glomerular function (ie GFR) is significantly
depressed, the retention of fixed acids results in a high anion gap acidosis.
- Three main clinical categories or 'types' of renal tubular acidosis (RTA) are now
recognised but the number of possible causes is large. The mechanism causing the defect
in ability to acidify the urine and excrete acid is different in the three types.
- Incomplete forms of RTA also occur. The arterial pH is normal in these patients and
acidosis develops only when an acid load is present.
ComparisonofMajorTypesofRTA
Type1 Type2 Type4
Hyperchloraemic
acidosis
Yes Yes Yes
MinimumUrinepH >5.5 <5.5(butusually>5.5
beforetheacidosis
becomesestablished)
<5.5
PlasmapotassiumLow-normal Low-normal high
Renal stones Yes No No
Defect ReducedH+
excretionin
distal tubule
ImpairedHCO3
reabsorptioninproximal
tubule
Impairedcation
exchangein
distal tubule](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-6-320.jpg)
![Acinetobacter
[created by
Paul Young
02/10/07]
General
- levels of environmental contamination with A. baumannii
correlate with patient colonization and infection. This organism
is very hardly and survives dessication.
- Acinetobacter are non-lactose fermenting, Gram-negative
coccobacilli that are strictly aerobic and non-motile.
- Acinetobacter baumanii is the most important species
associated with infections and nosocomial outbreaks
resistance
- Acinetobacter isolates are typically even more resistant than
Pseudomonas spp. to most antimicrobials, including broad-spectrum
cephalosporins, penicillins, fluoroquinolones and aminoglycosides.
infections
- It causes a wide range of nosocomial infections including
ventilator-associated pneumonia, bacteraemia, urinary tract
infections, skin and wound infections and meningitis
colonisation
- Acinetobacters form part of the normal bacterial flora of
the skin, particularly in moist regions such as the axillae,
groin and toe webs.
- Up to 25% of normal individuals carry cutaneous Acinetobacter,
and it is the most common gram-negative organism isolated from
the skin of hospital personnel.
transmission
- Dissemination of Acinetobacter in the environment can be a major
problem.
- It has been recovered from respiratory equipment, bed linen,
tables, patients' charts, sink traps, the floor and atmosphere,
especially in the vicinity of an infected or colonized patient
- Furthermore, Acinetobacter is able to persist in the environment
for several days, even in dry conditions, on particles and dust.
- Some strains are tolerant to soaps and disinfectants.
- The nosocomial spread of Acinetobacter is most often attributed
to exogenous contamination from equipment, environmental
surfaces and the hands of hospital personnel rather than endogenous
infection.
- Known resistance mechanisms include plasmid-mediated beta-lactamases,
which are also frequently associated with resistance to fluoroquinolones
and aminoglycosides.
- Chromosomal cephalosporinases may be responsible for the high
prevalence of ceftazidime resistance. However, the relationship
between observed antibiotic resistance patterns in vitro and the presence
of these beta-lactamases remains unclear. It is suggested that altered
penicillin-binding proteins and membrane impermeability may be the
major cause of high level resistance to beta-lactams, including imipenem
treatment
- Carbapenems are currently considered the antimicrobials of choice, although
epidemic outbreaks and endemic situations involving carbapenem-resistant
Acinetobacter species have been described
- Colistin, polymyxin B & ampicillin-sulbactam have all been
described in treatment of carbapenem-resistant strains](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-7-320.jpg)
![acute
coronary
syndromes
[created by
Paul Young
06/10/07]
general - coronary artery disease accounts for over 30% of deaths in Western countries.
classification
Unstable angina:
- ischaemic chest pain with is recent in origin, is more frequent, severe, or
prolonged than the patient's usual angina; is more difficult to control with drugs;
or is occurring at rest or with minimal exertion
- cardiac biomarkers are not elevated
Myocardial infarction:
- ischaemic symptoms with raised cardiac biomarkers
- STEMI: ST elevation
- NSTEMI: no ST elevation
risk
factors
modifiable:
(i) by life-style
- smoking
- obesity
- physical inactivity
(ii) by pharmacotherapy or lifestyle
- hypertension
- dyslipidaemia
- diabetes
- hyperhomocysteinaemia
non-modifiable:
- increasing age
- male gender
- family history
ECG
changes
in AMI
hyperacute (0-20 minutes)
- tall peaking T waves & progressive upward curving & elevation of ST segments
acute (minutes - hours)
- persistent ST elevation with gradual loss of R wave in the infarcted area.
ST segments begin to fall & there is progressive inversion of T waves
early (hours to days)
- loss of R wave and development of pathological Q waves in the area of ischaemia.
Return of ST segments to baseline with persistence of T wave inversion
indeterminate (days to weeks)
- pathological Q waves with persisting T wave inversion.
ST segments normalise (unless there is aneurysm)
old (weeks to months)
- persisting deep Q waves with normalised ST segments
anatomical
patterns of
myocardial
injury
biomarkers
in ACS
Troponin I or T:
- troponin rise indicates myonecrosis & is a high risk feature in non ST elevation acute coronary syndrome
- troponin remains elevated for 5-14 days and therefore may not be useful for identifying early reinfarction
-troponin elevation is often delayed by 4-6 hours after infarction
CK:
- should be monitored for 48 hours serially & can be measured subsequently if there is suspected reinfarction
CK-MB:
- more specific than CK for myocardial infarction & may be used to confirm a reinfarction
management
of ST
elevation AMI
reperfusion therapy:
- reperfusion can be obtained with fibrinolytic therapy or PCI
- a combination of fibrinolysis and PCI can also be used
- CABG surgery may occasionally be more appropriate with particular anatomy
& may be considered as rescue therapy in patients who fail revascularisation
- PCI is the best available treatment; however, benefit depends on prompt access to service and
if delay is longer than 90 minutes until balloon inflation thrombolysis should be administered.
- PCI is clearly better in the presence of cardiogenic shock
antiplatelet therapy:
- aspirin 300mg should be given to all patients with STEMI unless contraindicated
- both the VA Cooperative Study Group and the Canadian Multicentre Trial showed that aspirin reduces the
risk of death or myocardial infarction by 50% in patients with unstable angina or non-Q wave infarction
- clopidogrel should be given as a load 600mg to all patients who require a stent
& should be continued for at least 12 months; clopidogrel should be given to selected
patients given fibrinolysis. If urgent CABG is likely, clopidogrel should be withheld
- in the CURE trial, clopidogrel given in addition to aspirin within 24hrs of unstable angina symptoms led to significantly
reduced of cardiovascular death from 11.4% to 9.3% but was associated with a 1% absolute increase in major, non
life threatening bleeds as well as a 2.8% increase in major bleeds associated with CABG within 5 days
- ticlopidine & clopidogrel (thienopyridins) are second generation platelet inhibitors acting independently
& theoretically synergistically with aspirin
antithrombin therapy:
(i) with PCI: unfractionated heparin should be administered with dose dependent or whether IIb/IIIa
inhibitors are used; the role of enoxaparin in acute STEMI following PCI remains to be determined
(ii) with fibrinolysis: heparin or enoxaparin should be used fibrin-specific fibrinolytic
agents. The use of antithrombin therapy in conjuction with streptokinase is optional.
glycoprotein IIb/IIIa inhibitors:
- reasonable to use post primary PCI although data are conflicting regarding efficacy. They reduce mortality
the 30-day risk of non-fatal AMI by 38& in NSTEMI in patients undergoing PCI. They have not been shown to
be beneficial in the routine management of medically treated patients (GUSTO-IV-ACS)
- there are two classes of glycoprotein IIb/IIIa inhibitors
(i) murine monoclonal (eg abciximab)
(ii) 'small molecule' inhibitors (eg tirofiban & eptibatide)
- should be avoided with fibrinolytic therapy because of risk of bleeding; platelet infusion may treat significant
bleeding in patients receiving abciximab but not in those receiving tirofiban or eptifibatide)
risk stratification of
non ST elevation
acute coronary
syndromes
(i) high risk consists of clinical features of ACS with any of the following:
- repetitive or prolonged (>10mins) ongoing CP
- elevated cardiac biomarkers
- persistent or dynamic ECG changes (ST depression or TWI)
- transient ST elevation
- cardiogenic shock
- sustained VT
- syncope
- EF<40%
- prior CABG
- percutaneous coronary intervention within 6 months
- presence of known diabetes with typical ACS features
- chronic renal failure with typical ACS features
(ii) intermediate risk consists of clinical features with any of the following:
- resolved chest pain that occurred at rest or was repetitive or prolonged
- age >65
- known CAD
- two or more of the following risk factors (hypertension, family history, active smoking or hyperlipidaemia)
- presence of known diabetes mellitus with atypical ACS features
- presence of chronic renal failure with atypical ACS features
- prior aspirin use
(iii) low risk
- presentation with clinical features of an acute coronary syndrome without intermediate or high risk features
management of
non ST elevation
acute coronary
syndromes
- high risk patients require aggressive medical management and coronary angiography
- intermediate risk patients require inpatient monitoring and investigation and provocative testing
- low risk patients can be discharged with follow-up
- earliest rise of CK & CK-MB occurs at 3-4 hours with a peak at 12-24 hours and normalisation by 48 hours
criteria for AMI in LBBB
(i) new LBBB
(ii) concordant ST elevation of >1mm
(iii) concordant ST depression of >1mm in V1, V2 or V3
(iv) discordant ST elevation of >5mm
nitrates:
- reduce myocardial oxygen demand through afterload reduction and may on improve myocardial
oxygen delivery through coronary vasodilation
- may lead to dramatic resolution of ischaemia in coronary vasospasm
- GISSI-3 and ISIS-4 trials failed to demonstrate mortality reduction from acute or chronic nitrates; nevertheless,
they remain first line therapies for symptomatic angina and when myocardial infarction is complicated by CCF
beta blockers:
- iv beta blockers should be considered for patients with tachycardia or hypertension post infarct in the acute setting
- oral beta blockers decrease mortality after myocardial infarction and should be administered to all patients who can tolerate them
ACEIs:
- SAVE trial showed that captopril in patients with EF<20% post AMI lead to a 21% reduction in mortality
- ISIS-4 showed a smaller reduction in mortality for all patients treated with captopril post AMI
- HOPE showed patients with vascular disease or high risk of atherosclerosis benefited from ramipril
statins:
- decrease risk of adverse ischaemic events in patients with CAD thrombolysis
contraindications
absolute contraindications:
(i) active bleeding or bleeding diasthesis (excluding menses)
(ii) significant closed head injury or facial trauma within 3 months
(iii) suspected aortic dissection
(iv) risk of intracranial haemorrhage (any prior ICH, ischaemic
stroke within 3 months, cerebral vascular lesion, brain tumour)
relative contraindications:
- risk of bleeding
(i) current use of anticoagulants (the higher the INR the higher the risk)
(ii) non-compressible vascular punctures
(iii) recent major surgery
(iv) prolonged CPR >10 minutes
(v) internal bleeding within 4 weeks
(vi) active peptic ulcer
- risk of ICH
(i) history of chronic, severe, poorly controlled hypertension
(ii) severe uncontrolled HTN on presentation (>180mmHg systolic; or >110mmHg diastolic)
(iii) ischaemic stroke more than 3 months previously
- other
(i) pregnancy
- ESSENCE trial showed that low molecular weight heparin (enoxaparin) reduced the combined
end point of death, MI or recurrent ischaemia at both 14 & 30 days when compared with heparin
heart
block
in AMI
- 8% of patients with MI will only display ST elevation in posterior or right precordial leads](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-8-320.jpg)
![Acute
Pancreatitis
[created by
Paul Young
02/10/07]
classification
& definitions
- The widely used Atlanta classification categorizes acute
pancreatitis as mild or severe.
- pancreatitis is classified as severe any of the following 4 criteria are met:
(1) Organ failure with 1 or more of the following:
-shock systolic blood pressure <90 mm Hg),
- pulmonary insufficiency (PaO2 <60 mm Hg),
renal failure (serum creatinine level >176.8 ìmol/L after rehydration, and
gastrointestinal tract bleeding (>500mL in 24 hours);
(2) local complications such as:
- necrosis,
- pseudocyst,
- or abscess;
(3) at least 3 of Ranson’s criteria
(4) at least 8 of the APACHE II criteria.
Pancreatic necrosis:
- Pancreatic necrosis is the presence of a diffuse or focal area of nonviable
pancreatic parenchyma, often associated with peripancreatic necrosis.
- Severe acute pancreatitis with pancreatic or peripancreatic necrosis is also
referred to as necrotizing pancreatitis.
Infected pancreatitis:
- Initially a sterile necrosis (mortality, 10%), necrotizing pancreatitis becomes
infected with bacteria of gut origin in 40% to 70% of cases2 and is then called
infected necrosis (mortality, 25%).
Pancreatic pseudocyst:
- Pancreatic pseudocyst is a collection of pancreatic juice enclosed by
a wall of fibrous or granulation tissue that develops as a result of a persistent
leak of pancreatic juice from the pancreatic duct.
Pancreatic abscess:
- Pancreatic abscess is a circumscribed intra-abdominal collection of pus
that sometimes contains gas.
- It follows infection of a limited area of pancreatic or peripancreatic necrosis
and usually takes 4 to 6 weeks to evolve.
Aetiology
- From several large studies describing patients with severe
acute pancreatitis, the 2 most common causes of SAP are:
(i) chronic heavy alcohol use (approximately 40% of patients) and
(ii) gallstones (approximately 35% of patients).
- Less common causes of severe acute pancreatitis are:
(i) trauma to the pancreas,
(ii) hypercalcemia,
(iii) hypertriglyceridemia,
(iv) complications from ERCP or surgery.
(v) cystic fibrosis
(vi) infectious causes including HIV, EBV, CMV & viral
hepatitis as well as mycoplasma & campylobacter
(vii) drugs, poisons & toxins including organophosphates
- azathiprine, thiazides, mercaptopurine, valproate,
didanosine, pentamidine, cotrimoxazole & scorpion
envenomation
- In about 20% of patients, no cause can be identified.
Epidemiology
- Severe acute pancreatitis occurs in men more often than in women.
- Alcoholic pancreatitis is more common among men;
gallstone pancreatitis is more common among women.
Diagnosis
- Patients with SAP typically complain of fairly sudden onset of severe upper
abdominal pain, radiating to the back, often associated with nausea and vomiting.
- Marked elevations in serum amylase and/or lipase (>3 times the upper limit
of normal) support the diagnosis of pancreatitis in a patient with severe abdominal
pain. However, modest elevations of pancreatic enzymes may be observed in other
intra-abdominal emergencies.
- In the presence of pancreatitis, an increase in liver enzyme values, especially
of alanine aminotransferase to more than 3 times normal, suggests a biliary cause.
Imaging
Ultrasound
Abdominal ultrasonography can be used to detect gallstones,
although bowel gas may limit its accuracy in the acute setting.
CT
Contrast enhanced computed tomography (CT) is useful for differentiating SAP from
other conditions presenting with abdominal pain and elevated pancreatic enzymes.
It also helps to delineate local complications associated with SAP:
- Pancreatic or peripancreatic necrosis is diagnosed when some or all
of the pancreas or surrounding area fails to enhance with contrast.
- To determine whether a necrotic area is infected, it can be sampled by fine-needle
aspiration under CT guidance and analyzed with Gram stain and culture for evidence
of gut-derived bacteria and/or fungal organisms.
MRI
Magnetic resonance imaging is better than CT for distinguishing between
an uncomplicated pseudocyst and one that contains necrotic debris
MRCP and ERCP
Magnetic resonance cholangiopancreatography and endoscopic ultrasonography
can detect small bile duct stones as a cause of SAP.
Treatment
General:
- The initial treatment of SAP is supportive. Aggressive fluid resuscitation,
oxygen supplementation, and pain relief are critical.
- Interventions used in the past aimed at resting the pancreas (nasogastric suction and
acid suppression), diminishing secretion of enzymes (glucagon and somatostatin
administration), and countering the damaging effects of enzymes (use of
aprotinin, gabexate, or lexipafant) do not improve outcomes
Nutrition:
- In the past, patients with severe acute pancreatitis were administered parenteral nutrition
in an effort to avoid stimulation of the pancreas. More recently, it has been shown in animal
models that enteral nutrition prevents intestinal atrophy and improves the barrier function of
the gut mucosa.
- Three RCTs have demonstrated that enteral feeding is not only safe and feasible but
is also associated with fewer infectious complications, and is less expensive than TPN.
- Enteral feeding should be commenced whereever possible
Prevention of Pancreatic Infection:
- Pancreatic or peripancreatic infection develops in 40% to 70% of patients
with pancreatic necrosis and is the leading cause of morbidity and mortality
- Infection usually occurs at least 10 days after the onset of SAP.
- Methods to reduce the incidence of infection in patients with SAP include:
(i) selective gut decontamination - unproven
(ii) prophylactic systemic antibiotics - use of broad spectrum antibiotics is
supported by metanalysis data but may lead to fungal superinfection
- If fever or leukocytosis persists or develops beyond 7 to 10 days without an obvious
source of infection, fine-needle aspiration of the necrotic area should be performed
to rule out infection.
ERCP:
- A metaanalysis of 4 RCTs of endoscopic sphincterotomy
in patients with severe biliary pancreatitis showed that sphincterotomy
reduced complications and mortality of SAP in patients with biliary obstruction
or cholangitis.
- The role of early ERCP in patients without biliary obstruction or cholangitis is unclear.
One study reported higher mortality after ERCP in such patients.
- An accepted practice is to perform endoscopic sphincterotomy in patients with
evidence of biliary obstruction (cholangitis, jaundice) or elevated liver test results
except in those with rapidly normalizing test results.
Surgery:
- Debridement by surgery or a less invasive technique is indicated in
patients with infected necrosis. Outcomes are better if surgery is delayed
until the necrosis has organized, usually about 4 weeks after disease onset.
- The preferred surgical procedure for SAP is necrosectomy (debridement) with
the placement of wide-bore drains for continuous postoperative irrigation.
- For patients who are poor surgical candidates or who have well-contained infection,
minimal-access necrosectomy by either percutaneous or endoscopic routes
has shown encouraging results.
- For patients with biliary pancreatitis, cholecystectomy should be performed during
the initial hospitalization or after the resolution of intraabdominal inflammation to
prevent recurrence. In patients too ill to undergo cholecystectomy, endoscopic
sphincterotomy is an alternative.
CT grading
Prognosis
- mild acute pancreatitis has a mortality rate of less than 1%
- the death rate for severe acute pancreatitis is 10% with sterile
and 25% with infected pancreatic necrosis.
- Approximately half the deaths of patients with SAP occur within 2 weeks of
onset. Early morbidity and mortality in patients with SAP are attributable to
organ failure secondary to systemic inflammatory response syndrome.
- The remaining deaths occur because of later complications of infected necrosis.
indications for CT
indications for surgery
Ranson's criteria](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-9-320.jpg)
![acute renal
failure
[created by
Paul Young
30/12/07]
definition
- Numerous papers highlight the lack of a universal definition for ARF in ICU. One
review of the subject found 26 different definitions of postoperative ARF in 26 studies
- Even a consensus conference of intensivists and nephrologists on the subject in 2000
could not provide an adequate, universal definition. This makes it difficult to draw
conclusions from all the individual trials that are published.
epidemiology
- Acute renal failure (ARF) is a common problem in intensive care. It is said to have an
incidence of 10-25%. The diagnosis of ARF is not difficult, although the term ARF
encompasses a broad range of definitions with no universally accepted definition
- A specific definition of disease with tight exclusion criteria is essential in the design of
clinical studies of a heterogeneous syndrome
Particular issues around definition include
(i) Biochemistry:
- Is the absolute increase or the rate of increase of serum creatinine and urea important for
the definition? Are acid-base imbalance, serum potassium level and urine output
significant in the diagnosis?
(ii) Chronic renal impairment:
- How is this incorporated into the definition and what impact does it have on diagnosis,
management and outcome?
(iii) Resuscitation:
- Should reversible elements be corrected before the definition is applied? For example, is
the correction of mean arterial pressure and filling pressures to normal physiological
values necessary before ARF can be diagnosed?
(iv) Nephrotoxic drugs:
- what are the implications of nephrotoxic drugs, e.g. gentamicin or non-steroidal anti-
inflammatory drugs, for the definition and the aetiology?
(v) Pathophysiology:
- The underlying pathophysiological process is thought to be important to outcome.
Should this be included if it is known or should it be categorized according to aetiology?
(vi) Post-renal ARF:
- Causes of postrenal ARF often have a very different natural history and outcome; if this
is identified, should they be excluded?
(vii) Confounding factors:
- does an upper gastrointestinal haemorrhage or rhabdomyolysis need to be ruled out?
- The combined published results for ARF, its incidence and outcome are:
o An incidence of 10-25%.
o Patients who are admitted with or develop ARF on the ITU have an overall mortality of 23-80%
o Patients with ARF not requiring RRT have a mortality of 10-53%
o Patients who develop ARF that requires RRT have a higher mortality of 57-80%
o Of those patients with ARF who receive RRT and survive, only 5-30% require longer-term dialysis.
o The mortality of patients who are admitted to ITU with ARF, or who go on to develop ARF, remains high.
- This wide variation in published results (up to six-fold) is due in part to the following
problems that are not specifically addressed in the majority of studies:
(i) Inclusion criteria vary between studies because the definition of what constitutes ARF is so variable.
(ii) There is significant heterogeneity of the population in terms of severity of illness and demographics.
(iii) Many different disease processes can cause ARF, so one may not be comparing like with like.
Is it the incidence of ARF that varies or the incidence of the disease process in different centres?
(iv) Different disease processes have different incidences of renal damage and mortality.
(v) Some centres are moving to the early initiation of RRT, often prior to the
development of 'criteria' to define ARF. Should this group be considered separately?
(vi) Outcome analysis varies: 14-day, 15-day, 28-day and 30-day mortality have all been used
as endpoints. Alternatively, ICU, in-hospital or 1-year mortality figures have been used.
parenchymal
renal failure
general:
- this is used to define a syndrome where the principle source of damage is within
the kidney and where typical structural changes can be seen on microscopy
- pathogenesis of parenchymal renal failure is generally immunological and varies
from vasculitis to interstitial nephropathy
aetiology
- more than 1/3rd of patients who develop ARF in ICUs have chronic renal dysfunction
due to factors such as age related changes, long-standing changes, long-standing
hypertension, diabetes or renal vascular disease
drug-induced renal failure
- many cases of drug-induced renal failure improve rapidly on removal of the offending
agent and accordingly a drug history is important in all cases of renal failure
hepatorenal failure
(i) general:
- a form of ARF that occurs in the setting of severe liver dysfunction in the absence of other
known causes of ARF. Typically, it presents as progressive oliguria with a very low urinary
sodium (<10mmol/L)
- pathogenesis is not well understood but it is thought to involve severe vasoconstriction
(ii) differential diagnosis:
- other causes of acute renal failure are more common than hepatorenal syndrome in severe
liver disease. They include sepsis, paracentesis-induced hypovolaemia, alcoholic cardiomyopathy
or any combination of these
(iii) prevention and treatment:
- the use of albumin in patients with SBP has been shown to reduce renal failure in an RCT
- studies suggest vasopressin derivatives (terlipressin) may improve GFR
rhabdomyolysis-associated ARF
- accounts for 5-10% of cases of ARF in ICU depending on the setting
- pathogenesis involves pre-renal, renal and post renal factors
- typically seen following major trauma, drug overdose & vascular embolism
- treatment principles are based on retrospective data and include aggressive fluid resuscitation,
elimination of causative agents, correction of compartment syndromes, alkalinisation of urine
(pH>6.5), and maintenance of polyuria
prognosis
- Renal replacement therapy (RRT) is now a routine element of organ support in the
intensive therapy unit (ITU). Yet despite great improvements in the recognition
and management of ARF, including RRT, the mortality of patients who are admitted to
ITU with ARF, or who subsequently develop ARF, remains high at 23-80%.
- if the cause of ARF has been removed and he patient has become physiologically stable slow recovery
occurs over 4-5 days to 3-4 weeks; in some cases the urine output can be above normal for several days
prevention
general:
- the fundamental principle of acute renal failure is to treat its cause.
- if pre-renal factors contribute these must be identified and haemodynamic
resuscitation quickly instituted
resuscitation:
- intravascular volume must be maintained or rapidly restored & oxygenation must
be maintained; an adequate haemoglobin concentration should be maintained
- once intravascular volume has been restored, some patients remain hypotensive.
In these patients autoregulation of renal blood flow may be lost & increasing MAP
with vasopressors may increase GFR; the role of additonal fluid in a patient with
normal blood pressure and cardiac output is questionable
- despite the above measures pre-renal renal failure may develop if cardiac output
is inadequate
nephroprotective drugs:
(i) 'low dose' dopamine
- evidence of efficacy or safety is lacking; however, this agent is a tubular diuretic
and occasionally increases urine output
- randomised controlled trial evidence in critically ill patients shows that low-dose
dopamine is no more effective than placebo in prevention of renal dysfunction; however,
in patients with low cardiac output dopamine may increase cardiac output, renal blood
flow and GFR (as would dobutamine or milrinone)
(ii) mannitol
- animal experiments offer some encouraging findings; however, no human data exist to
support its clinical use
(iii) loop diuretics
- these agents may protect the loop of Henle from ischaemic from decreasing its transport
related workload; however, there are no double blind randomised controlled trials proving
that these agents reduce the incidence of renal failure
- several studies support the view that loop diuretics may decrease the need for dialysis
in patients developing acute renal failure. They appear to achieve this by inducing polyuria
which results in the prevention or easier contorl of volume overload, acidosis & hyperkalaemia
- because avoiding dialysis simplifies treatment and reduces the cost of care, loop diuretics
may be useful
(iv) other agents
- other experimental agents include theophylline, urodilatin and anaritide (a synthetic atrial
natriuretic factor)
investigation
general investigations include:
(i) examination of urinary sediment and exclusion of a urinary tract infection (most if not all patients)
(ii) careful exclusion of nephrotoxins (all patients)
(iii) exclusion of obstruction (some patients)
special investigations may include:
(i) CK and myoglobin (for rhabdomyolysis)
(ii) chest x-ray, blood film
(iii) specific antibodies (anti-GBM, antidsDNA, anti-smooth muscle etc)
(iv) LDH, haptoglobin, unconjugated bilirubin
(v) cryoglobulins
(vi) Bence Jones Proteins
(vii) renal biopsy
- differentiation of prerenal and renal failure has limited clinical implication
because they are part of the same continuum and treatment is the same
post-renal
failure
general:
- obstruction to urine outflow is the most common cause of functional
renal impairment in the community but is uncommon in the ICU
- involves humoral and mechanical factors
aetiology:
- typical causes include bladder neck obstruction from an enlarged prostate, ureteric obstruction
from pelvic tumours or retroperitoneal fibrosis, papillary necrosis or large calculi
clinical presentation:
- clinical presentation may be acute or acute on chronic in patients with long standing calculi.
It may not always be associated with oliguria.
diagnostic criteria for hepatorenal syndrome
pre-renal
renal
failure
general:
- this form of ARF is the most common in ICUs
- indicates that the kidney malfunctions predominantly because of the systemic factors which
diminish renal blood flow and decrease GFR or by alteration of intraglomerular haemodynamics
pathophysiology:
- renal blood flow is decreased by:
(i) decreased cardiac output
(ii) hypotension
(iii) raised intraabdominal pressure (decompression should be considered when
the intrabdominal pressure is greater than 25-30mmHg above the pubis)
- in septic patients with hyperdynamic circulations there may be adequate global blood flow to the kidney but intrarenal shunting
away from the medullar causing medullary ischaemia or efferent arteriolar dilation thus decreasing GFR
- if the systemic cause of renal failure is rapidly removed renal function improves relatively rapidly
- several mechanisms are involved in the development of renal injury in pre-renal failure:
(i) ischaemia of the outer medulla with activation of tubuloglomerular feedback
(ii) tubular obstruction from casts of exfoliated cells
(iii) interstitial oedema secondary to back diffusion of fluid
(iv) humorally mediated afferent arteriolar renal vasoconstriction
(v) inflammatory response to cell injury and local release of mediators
(vi) disruption of normal cellular adhesion to the basement membrane
(vii) radical oxygen species induced apoptosis
(viii) mitogen-activated protein kinases-induced renal injury](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-10-320.jpg)
![acute right
ventricular
dysfunction
[created by
Paul Young
22/10/07]
causes
general
pathophysiology
imaging
biochemistry
- Right heart failure is characterized by a low cardiac output, hypotension, hepatic enlargement and raised JVP.
- Cardiogenic shock due to right ventricle failure has a mortality rate comparable to left ventricle failure
Right ventricular function:
- In systole, because of the constraints imposed by the pericardium, the high pressure in the left ventricle
and the heart's anatomical configuration, the septum intrudes into the right ventricular cavity.
- The right ventricle is better suited to volume overload than the left, but increased afterload is more detrimental.
- The low pressures in the right side of the heart arise as a result of the thin walled ventricle and highly compliant pulmonary circulation.
- The lack of myocardial bulk means that contractility cannot be maintained in the face of increased pulmonary resistance.
- In pulmonary hypertension, dilatation occurs as a compensating mechanism.
Right heart failure:
- In all cases, there is a critical point at which ventricular dilatation cannot compensate.
- Consequently, there is reversal of the ventricular septal pressure gradient, abnormal septal movement, rising atrial pressures and TR.
- The abnormal volume and pressure loading stress the right side of the heart, resulting in increased oxygen demand, decreased
coronary driving pressures and worsening right ventricle output. The global reduction in left sided preload contributes to systemic
hypotension exacerbated by septal dyskinesia and reversal of the interventricular dependence pressures. This in turn further lowers
coronary perfusion pressures. This vicious cycle has been termed auto-aggravation.
clinical
diagnosis
problems with clinical diagnosis:
(i) right ventricular failure may exist in the absence of peripheral oedema.
(ii) peripheral oedema is not discriminatory for right heart failure.
(iii) elevated jugular venous pressures and abnormal waveforms may be distorted by
mechanical ventilation, body habitus and lung hyperinflation in COPD patients.
(iv) signs such as hypotension, tachycardia, tachypnoea & hepatomegally are nonspecific.
CXR
- Changes in the pulmonary vasculature and the cardiac shadow may allow the diagnosis of underlying
pathology potentially associated with pulmonary hypertension and, by inference, right ventricular involvement
Echocardiography
- Echocardiography can show structural change, dynamic responses to intervention and
allows quantitative and qualitative measurements to refine the significance of findings.
- With transthoracic echocardiography (TTE) multiple measurements, ratios and estimates
have been used to assess quantitative and qualitative parameters including:
(i) tricuspid regurgitation;
(ii) long axis cavity size,
(iii) short axis septal kinetics,
(iv) apex loses triangle shape;
(v) right ventricular end-diastolic area/left ventricular end-diastolic area (>0.6 or >1);
(vi) left inferior hypokinesis;
(vii) right ventricle size in comparison to left ventricle;
(viii) right ventricular end diastolic volume diameter >30mm at level of mitral valve from left precordial view;
(ix) loss of inspiratory collapse of inferior vena cava
(x) dilation of pulmonary artery,
(xi) tricuspid regurgitation;
Right heart catherisation
- Right heart catheterisation and thermodilution are invasive but can provide nearly continuous values, in
contrast to other modalities, for right heart cardiac output and continuous right heart pressures.
- Natriuretic peptides induced by myocardial stress and dilatation are an attractive means to detect heart failure and to monitor
response to treatment. They have been used to stratify outcome in acute pulmonary embolismand in long-term follow-up for
patients with surgically corrected tetralogy of Fallot, and also as predictors of mortality in hypertension, renal failure, amyloidosis,
sepsis and diabetes.
- Plasma levels of natriuretic peptides have been shown to be proportional to the magnitude
of right ventricle dysfunction and correlate negatively with the ejection fraction.
- Levels vary in populations, sex, age groups and between various disease states. In the critically ill patient population natriuretic
peptides may be elevated due to underlying or coexisting heart disease or lung disease.
inotropes
& vasopressors
- No selective right heart inotrope exists.
- Augmentation of contractility can be achieved by b-mimetics, calcium sensitizers and phosphodiesterase
inhibitors. The problem is that without afterload manipulation, increasing right heart contractility and hence output,
increases myocardial oxygen consumption but without a systemic benefit.
general
treatment
aims
- The aim in the management of right ventricular dysfunction is to disrupt the cycle of auto-aggravation.
- For a given contractile state, reducing afterload will increase the ejection fraction.
- Similarly in a normal afterload state, augmentation of contractility raises the right ventricular ejection fraction.
- Volaemic status is difficult to judge. In a dilated decompensated ventricle with elevated atrial pressures, volume reduction is most likely to
improve the right ventricular ejection fraction. In the absence of elevated right atrial pressure then monitored volume challenges are justified.
- Reduction in myocardial oxygen demand or improvements in coronary perfusion must also be considered.
volume
optimisation
- Failure can be defined as the point at which the right ventricle fails to compensate for an increased ventricular volume, as each fibre
has an optimal stretch to allow maximal pressure generation, which, when exceeded, results in dilatation and eventually ventricular failure.
- Determination of preload is problematical but the presence of high right atrial filling pressures is indicative of elevated right ventricular pressures,
which extrapolates to a raised ventricular volume. This may not necessarily be true in all cases and depends on the compliance of the ventricle.
- In chronic elevation of right atrial pressures the pressure may be high, but this is a poor predictor of volume response, the patient may
therefore still be volume recruitable and sequential monitored fluid challenges are justified.
- The appearance of a dilated right ventricle with a reduced ejection fraction, however, should prompt a reduction in preload in a patient who is
not volume responsive (as defined by lack of alteration in heart rate, blood pressure, cardiac and urine output).
- The effect of therapy can be monitored by sequential echocardiography or by using right heart catheterization and, ideally, continuous measurement.
The converse is true though: sequential volume challenges monitored by pulmonary artery pressure changes in the absence of reversed right ventricle
interdependence will increase cardiac output, up to the individualized optimal filling point.
- The calcium sensitizing, lusitropic agent, levosimendan has been shown to provide a survival advantage in
heart failure trials. In a pilot study of levosimendan in early ARDS, Morelli et al. demonstrated that a reduction
in the pulmonary vascular resistance by levosimendan improved right ventricular function.
- Inotropes may provide a benefit in instances where ischaemia related to hypotension is a problem.
- They elevate the mean arterial pressure, coronary artery perfusion and may, consequently, reduce myocardial work.
- Vasotropic agents such as noradrenaline, phenylephrine and vasopressin may elevate diastolic pressures and
thus improve myocardial oxygenation. The benefit is lost once the right ventricle consumes more oxygen, to maintain
output, in the face of the elevated afterload.
- Phosphodiesterase inhibitors such as milrinone and amrinone inhibit the phosphodiesterase
enzymes responsible for cAMP/cGMP breakdown, augmenting myocardial contractility.
- The advantage of this drug class is that the mechanism is independent of b-adrenoceptor states and does not
increase myocardial oxygen demand. Nebulized milrinone, interestingly, has been shown to have an additive
effect with prostaglandin I2 in terms of pulmonary vasodilation.
- Hypoxaemia and hypercarbia worsen pulmonary artery pressures as does positive end expiratory pressure (PEEP), intrinsic PEEP
and high tidal volumes. Optimization of these variables needs to occur before pharmacological manipulation is undertaken.
afterload
reduction
General
- The poor contractile reserve of the right ventricle means that the primary modality for treatment of acute right ventricle
dysfunction secondary to elevated pulmonary artery pressures is by means of selective pulmonary vasodilation.
- Acutely, afterload reduction may be effected by using localized (inhaled) or systemic vasodilators. The consequences
of selected pulmonary vasodilation are of decreased resistance (and consequently afterload), improved VQ matching
and decreased arterial hypoxaemia.
Prostaglandins
- Prostaglandins can be given by inhalation, systemically or subcutaneously.
- The vasodilatory effects are mediated by nitric oxide release and interaction at a local level with the vascular endothelial smooth
muscle. Prostaglandin E1 systemically undergoes significant first pass pulmonary metabolism but with lower systemic pressures
and resistance, adversely altering the ventilation-perfusion matching and subsequently arterial oxygenation.
- When infused or as an aerosolized agent it is less effective than nitric oxide or aerosolized prostaglandin I2. Iloprost is
a stable carbacycline analogue of prostaglandin I2, a short acting natural prostaglandin. The vascular spillover of inhaled
iloprost, in combination with its prolonged plasma half-life, results in its systemic actions of lowered mean arterial pressure
and systemic vascular resistance.
- Nebulized prostaglandins are attractive in that they have limited systemic effects, are cheap and do not require specialized
delivery systems. The particle size, however, cannot easily be controlled and hence inefficiency of delivery may be significant
resulting in higher doses with potential systemic spillover.
Nitric oxide
- Inhaled nitric oxide (iNO), by virtue of its localized vascular endothelial action, through cGMP generation and its interaction
with calcium gated potassium channels and protein kinase G as well as cGMP independent paths, acts as pulmonary vasodilator.
Its effects are limited to the ventilated areas of the lung, with minimal
systemic overspill because of its rapid inactivation by haemoglobin
- No outcome benefit has yet been demonstrated in responders,
however, although oxygenation and pulmonary resistance do improve.
- Withdrawal of nitric oxide has been shown to result in rebound pulmonary hypertension
- Inhaled nitric oxide requires specialized delivery systems and the side-effect profile is significant, with platelet dysfunction,
myocardial depression, renal failure and the formation of toxic compounds such as peroxynitrites. The side effects are dose
dependent and although recommended doses are under 10 ppm quantities up to 80 ppm have been used.
Sildenafil
- Sildenafil is a phosphodiesterase V enzyme, whose inhibition prolongs the
action of cGMP, with the overall effect of reducing pulmonary vascular tone.
- Tadalafil and vardenafil, members of the same class of phosphodiesterase inhibitors, have similar effects but of different
magnitude and duration. Sildenafil has been evaluated in decompensated right ventricular dysfunction, but its lack of an
intravenous preparation limits its use.
Systemic vasodilators
- Systemic vasodilators such as sodium nitroprusside, glyceryl trinitrate and hydralazine all reduce pulmonary afterload but at the expense
of systemic hypotension,decreasing coronary ostial perfusion pressures and potentially leading to a deleterious preload reduction,
exacerbating the dysfunction of the right ventricle, already compromised because of high right ventricular end diastolic pressure, through
ischaemia. Hence selective pulmonary vasodilators are more desirable in reducing afterload than global agents.
Recombinant BNP
- Neseritide is a recombinant version of BNP. Its actions, when infused, are identical to the in-vivo effects of BNP (natriuresis,
sympathetic dampening and suppression of the renin- angiotensin axis by increasing cGMP). It reduces both preload and afterload,
consequently improving cardiac output without inotropy. Concerns exist over the decreased 30-day survival and its adverse impact
on renal function.
- In addition the systemic side effect can be that of hypotension and subsequently, decreased coronary perfusion pressures.
- To date it has not been evaluated in pure right heart failure.
Mechanical
ventilation
& PEEP
- The distending alveolar pressure, when transmitted through the pulmonary capillary bed, determines the opening pressure
of the pulmonary artery valve.
- The greater the tidal volume the greater the impedance and hence the myocardial power generation has to be increased.
- Pleural pressure is transmitted to the myocardium because of the constricting pericardium, which limits the extent of
ventricular distension. Thus for an increase in pleural pressures a consequently higher preload is required to maintain the
right ventricular end diastolic volume
- A right ventricular friendly strategy is to set PEEP to limit gas trapping with prolonged expiratory times and to utilize as low a tidal
volume and respiratory rate as possible without deleterious ventilatory consequences
Surgical,
interventional
and right
ventricular
support
- The management of acute right ventricular infarction should follow standard guidelines for the reperfusion of occluded coronary arteries.
- Pacing, where indicated, has been shown to reduce mortality in biventricular failure and
should be considered in order to restore atrioventricular synchrony to ensure adequate preload
- Right ventricular assist devices may be appropriate in particular circumstances](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-11-320.jpg)
![additional
indices in
analysis
of metabolic
acidosis
[created by
Paul Young
13/12/07]
urinary
anion
gap
General
- The cations normally present in urine are Na+, K+, NH4+, Ca++ and Mg++.
- The anions normally present are Cl-, HCO3-, sulphate, phosphate and some organic anions.
- Only Na+, K+ and Cl- are commonly measured in urine so the other charged
species are the unmeasured anions (UA) and cations (UC).
Urinary Anion Gap = [Na+]+ [K+] - [Cl-]
Clinical Use
- The urinary anion gap can help to differentiate between GIT and renal causes of a
hyperchloraemic metabolic acidosis.
- It has been found experimentally that the Urinary Anion Gap (UAG) provides a rough
index of urinary ammonium excretion. Ammonium is positively charged so a rise in its
urinary concentration (ie increased unmeasured cations) will cause a fall in UAG
Pathophysiology
- Hyperchloraemic acidosis can be caused by:
(i) Loss of base via the kidney (eg renal tubular acidosis)
(ii) Loss of base via the bowel (eg diarrhoea).
(iii) Gain of mineral acid (eg HCl infusion).
- If the acidosis is due to loss of base via the bowel then the kidneys can respond
appropriately by increasing ammonium excretion to cause a net loss of H+ from the body.
The UAG would tend to be decreased, That is: increased NH4+ (with presumably
increased Cl-) => increased UC =>decreased UAG.
- If the acidosis is due to loss of base via the kidney, then as the problem is with the kidney
it is not able to increase ammonium excretion and the UAG will not be increased.
- Experimentally, it has been found that patients with diarrhoea severe enough to cause
hyperchloraemic acidosis have a negative UAG (average value -27 +/- 10 mmol/l) and
patients with acidosis due to altered urinary acidification had a positive UAG.
Osmolar
Gap
general
- An osmole is the amount of a substance that yields, in ideal solution, that number of
particles (Avogadro's number) that would depress the freezing point of the solvent by 1.86K
- Osmolality is measured in the laboratory by machines called osmometers. The units of
osmolality are mOsm/kg of solute
- Osmolarity is calculated from a formula which represents the solutes which under ordinary
circumstances contribute nearly all of the osmolality of the sample. There are many such
formulae which have been used. One is:
Calculated osmolarity = (2 x [Na+]) + [glucose] + [urea]
- The osmolar gap is the difference between the 2 values: the (measured) osmolality and
the (calculated) osmolarity (which is calculated):-
Osmolar gap = Osmolality - Osmolarity
- An osmolar gap > 10 mOsm/l is often stated to be abnormal.
Importance of the type of osmometer
- Only osmometers using freezing point depression method should be used for determining
this calculation because they are the only type of osmometer that can detect all the volatile
alcohols which can abnormally increase the osmolar gap. Vapour pressure osmometers can't do this
Significance of an elevated osmolar gap
- An elevated osmolar gap provides indirect evidence for the presence of an abnormal
solute which is present in significant amounts. To have much effect on the osmolar gap,
the substance needs to have a low molecular weight and be uncharged so it can be present
in a form and in a concentration (measured in mmol/l) sufficient to elevate the osmolar
gap.
- Ethanol, methanol & ethylene glycol are three such solutes that, when present in
appreciable amounts, will cause an elevated osmolar gap. If you suspect that your patient
may have ingested one of these substances than you should determine the osmolar gap.
- if the ethanol levels are measured they can be added to the calculated osmolarity to
exclude the presence of an additional contributer to the osmolar gap. [NB: To convert
ethanol levels in mg/dl to mmol/l divide by 4.6. For example, an ethanol level of 0.05% is
50mg/dl. Divide by 4.6 gives 10.9mmols/l]
delta
ratio
Definition
- The Delta Ratio is sometimes useful in the assessment of metabolic acidosis.
- The Delta Ratio is defined as:
Delta ratio = (Increase in Anion Gap / Decrease in bicarbonate)
Use
- In order to understand this, consider the following:
- If one molecule of metabolic acid (HA) is added to the ECF and dissociates, the one H+
released will react with one molecule of HCO3- to produce CO2 and H2O. This is the
process of buffering. The net effect will be an increase in unmeasured anions by the one
acid anion A- (ie anion gap increases by one) and a decrease in the bicarbonate by one.
- if all the acid dissociated in the ECF and all the buffering was by bicarbonate, then the
increase in the AG should be equal to the decrease in bicarbonate so the ratio between
these two changes (which we call the delta ratio) should be equal to one. The delta ratio
quantifies the relationship between the changes in these two quantities.
- the above assumptions about all buffering occurring in the ECF and being totally by
bicarbonate are not correct. Fifty to sixty percent of the buffering for a metabolic acidosis
occurs intracellularly. This amount of H+ from the metabolic acid (HA) does not react
with extracellular HCO3- so the extracellular [HCO3-] will not fall as far as originally
predicted. The acid anion (ie A-) however is charged and tends to stay extracellularly so
the increase in the anion gap in the plasma will tend to be as much as predicted.
- Overall, this significant intracellular buffering with extracellular retention of the
unmeasured acid anion will cause the value of the delta ratio to be greater than one in a
high AG metabolic acidosis.
Sources of error:
- Inaccuracies can occur for several reasons, for example:
(i) Calculation requires measurement of 4 electrolytes, each with a measurement error
(ii) Changes are assessed against 'standard' normal
values for both anion gap and bicarbonate concentration.
Assessment
< 0.4
- Hyperchloraemic normal anion gap acidosis
- A low ratio occurs with hyperchloraemic normal anion gap acidosis. The reason here is
that the acid involved is effectively hydrochloric acid (HCl) and the rise in plasma
[chloride] is accounted for in the calculation of anion gap (ie chloride is a 'measured
anion').
- The result is that the 'rise in anion gap' (the numerator in the delta ration calculation)
does not occur but the 'decrease in bicarbonate' (the denominator) does rise in numerical
value.
- The net of of both these changes then is to cause a marked drop in delta ratio,
commonly to < 0.4
0.4 - 0.8
- Consider combined high AG & normal AG acidosis BUT note
that the ratio is often <1 in acidosis associated with renal failure
1 to 2
- Usual for uncomplicated high-AG acidosis.
- Lactic acidosis: average value 1.6
- DKA more likely to have a ratio closer to 1 due to urine ketone loss
(esp if patient not dehydrated)
> 2
- A high delta ratio can occur in the situation where the patient had quite an elevated
bicarbonate value at the onset of the metabolic acidosis. Such an elevated level could be
due to a pre-existing metabolic alkalosis, or to compensation for a pre-existing
respiratory acidosis (ie compensated chronic respiratory acidosis).
anion
gap
General:
- The term anion gap (AG) represents the concentration of all the unmeasured anions in
the plasma. The negatively charged proteins account for about 10% of plasma anions and
make up the majority of the unmeasured anion represented by the anion gap under normal
circumstances.
- the AG = [Na+] + [K+] - [Cl-] - [HCO3-] and a the upper range of normal is about 15
Major Clinical Uses of the Anion Gap
(i) To signal the presence of a metabolic acidosis and confirm other findings
- If the AG is greater than 30 mmol/l, than it invariably means that a metabolic acidosis is
present. If the AG is in the range 20 to 29 mmol/l, than about one third of these patients
will not have a metabolic acidosis.
(ii) Help differentiate between causes of a metabolic acidosis:
-high anion gap versus normal anion gap metabolic acidosis.
The effect of albumin & phosphate
- Albumin is the major unmeasured anion and contributes almost the whole of the value
of the anion gap.
- Every one gram decrease in albumin will decrease anion gap by 2.5 to 3 mmoles. A
normally high anion gap acidosis in a patient with hypoalbuminaemia may appear as a
normal anion gap acidosis.
- This is particularly relevant in Intensive Care patients where lower albumin levels are
common.
- the 'normal anion gap depends on the serum phosphate and the serum albumin.
anion gap = 0.2 x [albumin] (g/L) + 1.5 x [phosphate] (mmol/L)
metabolic acidosis with increased anion gap:
Methanol, metformin
Uraemia
DKA
Phenformin, paraldehyde, propylene glycol, pyroglutamic acidosis
Iron, isoniazid
Lactic acidosis
Ethanol ketoacidosis, ethylene glycol
Salicylates, starvation ketoacidosis, solvent
metabolic acidosis with normal anion gap:
Ureteroenterostomy (K+ decreased)
Small bowel fistula (K+ decreased)
Extra chloride (K+ increased)
Diarrhoea (K+ decreased)
Carbonic anhydrase (K+ decreased)
Renal tubular acidosis (K+ decreased - type 1)
Addison's disease (K+ increased)
Pancreatic fistula (K+ decreased)](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-12-320.jpg)


![adrenal
insufficiency
in sepsis &
septic shock
[created by
Paul Young
10/12/07]
guidelines
- international guidelines recommend the use of low dose corticosteroids for the treatment
of septic shock. However, there are some discrepancies in these recommendations.
(i) the Surviving Sepsis Campaign recommended the use of stress dose of corticosteroids
for septic shock regardless of adrenal function.
(ii) the American College of Critical Care Medicine Task Force recommended that stress
dose of corticosteroids should be used only in refractory septic shock or in adrenal
insufficient patients.
mechanisms
of action of
corticosteroids
genomic actions
- Cells from most tissues are responsive to corticosteroids, which freely cross cell
membranes. The glucocorticoids receptor forms an inactive intracytosolic complex with
chaperone proteins like heat shock protein (HSP) 40, HSP56, HSP70, and HSP90,
immunophillins, P23, and other unknown proteins
- The receptor contains three domains: one binds corticosteroids, one binds to DNA, also
involved in dimerization; and one activates the promoters within the genes.
- Binding of corticosteroids to the glucocorticoids receptor induces the release of
chaperone proteins and the dimerization of the complex, which then, enters into the
nucleus and interacts with specific binding sequences, the glucocorticoid responsive
element (GRE).
- Subsequently, transcription of some genes (e.g.most cytokines, adhesionmolecules,
lipoxygenase, etc.) initiated by various transcriptional factors such as AP1, NF-AT and
NF-kB are prevented. In addition, glucocorticoids receptor dimers induce the inhibitor of
NFkB (IkB).
- Other GRE sites upregulate the transcription of numerous other genes (e.g. lipocortin-1,
thymosin-b4 sulfoxide).
Nongenomic interactions
- Physicochemical interactions occur in-between the cell's membrane and corticosteroids
inducing very rapid (within seconds), nonspecific, nongenomic effects.
- Some of these effects might be part of the host response to sepsis. For example, loss in
the corticosteroids physicochemical interaction with hypothalamic synaptosomes], may
partly explain the loss in circadian rhythm of cortisol synthesis during sepsis.
- non genomic effects of cortisol are thought to control immediate catecholamine release
from sympathetic cells. Such neural modulation by corticosteroids may explain the rapid
restoration of sympathetic modulation on heart and vessels, and may account for the
hydrocortisone induced rapid pressure sensitization to exogenous catecholamine in septic
shock.
corticosteroid
induced
immune
modulation
- by interacting with NF-IL6, corticosteroids enhance the synthesis of the acute phase
reactants; with AP-1 and NF-kB, they inhibit the synthesis of various proinflammatory
factors.
- corticosteroids prevent the migration of inflammatory cells from circulation to tissues
by blocking the synthesis of various chemokines and chemotactic cytokines. They
prevent the synthesis of almost all proinflammatory cytokines including several
interleukins (interleukin-1, interleukin-2, interleukin-3, interleukin-6), interferon-g (IFN-
g), granulocyte macrophage colony stimulating factor, and tumor necrosis factor-a (TNF-
a). They also enhance the production of the macrophage migration inhibitory factor
(MIF).
- by stimulating the synthesis of lipocortin-1, corticosteroids inhibit the synthesis of
soluble phospholipase A2 (PLA2) and the subsequent arachidonic acid cascade, reducing
the production of leukotrienes, the main inflammatory mediators in humans.
- corticosteroids also inhibit the synthesis of inducible cyclooxygenase-2 (COX2) and of
inducible but not constitutive nitric oxide synthase (NOS).
corticosteroid
induced
cardiovascular
modulation
- Chronic corticosteroid excess induces hypertension, whereas adrenal insufficiency
induces hypotension.
- corticosteroids regulate vascular responses to norepinephrine and angiotensin II, but not
to vasopressin. The underlying mechanisms remained unclear, and may involve multiple
pathways like iNOS and COX-2 inhibitions or the stimulation of the phosphoinositide
system.
human
studies
- in healthy volunteers, a 6-hour infusion of 3 mg/kg/min hydrocortisone, either immediately before or
concomitantly to endotoxin exposure, prevented LPS-induced fever, tachycardia, increase in plasma
levels of epinephrine, CRP, and TNF-a, but not interleukin-6.
conclusion
- In septic shock, intravenous hydrocortisone (about 300 mg for 5 days) decreases core temperature,
heart rate, and plasma levels of PLA2 and C-reactive protein.
- In a French multicenter trial on low dose corticosteroids in septic shock, it was shown that the
systemic inflammatory response to sepsis, assessed by interleukin-6 levels, was significantly
altered by corticosteroids only in adrenal insufficient patients
- nonresponders (increment in cortisol of 9 mg/dl or less) to 250 mg of corticotropin. In that study,
the adrenal insufficient septic shock had higher TNFa, interleukin-6 and interleukin-8 levels than
the remainders.
- In another placebo-controlled, randomized trial, 41 patients with septic shock received 50mg bolus
followed by a continuous infusion of 0.18 mg/kg/h of hydrocortisone until shock reversal. In that study,
as compared with the placebo, interleukin-6 levels were also significantly decreased by hydrocortisone
infusion, whereas interleukin-10 levels remained unaltered.
- low dose of hydrocortisone has been shown to downregulate sepsis-associated overexpression of
the 'late' inflammatory mediator, MIF by peripheral blood monocytes
- In a recent randomized study, the acute vascular effects of hydrocortisone (200 mg intra-arterial over
3 hours) were investigated in healthy adult male volunteers. This study elegantly demonstrated that
hydrocortisone did not affect biochemical or physiologic markers of nitric oxide activity. Thus, one can
conclude that any early (within 3 h) vascular effect of hydrocortisone is not mediated through the NO
pathway.
- In septic shock, several placebo-controlled randomized studies have reported the cardiovascular
effects of low dose of corticosteroids (about 200-300 mg/day) given for a prolonged period. These
studies consistently showed that corticosteroids increased systemic vascular resistance with little
effects on the cardiac index and pulmonary hemodynamics.
- trials consistently show that corticosteroids reduce the duration of shock. The
probability of being weaned from vasopressor at one week was greater in corticosteroid-
treated septic shock than in placebo-treated septic shock and the relative risk was 1.60
- Only three trials have subgroup analyses based on adrenal insufficiency. However, only two studies
used the same definition for adrenal insufficiency. In both of them, the favorable effects of corticosteroids
on shock reversal were observed only in the adrenal insufficient patients (nonresponders to corticotropin).
- In the first study of 300 patients with septic shock, the median time to weaning from vasopressors was
reduced by 3 days in the corticosteroid-treated adrenal insufficient patients compared with the placebo
group (P = 0.001), while there were no difference between corticosteroids and placebo in the responders
to corticotropin. In the second study, hydrocortisone significantly shortened the duration of shock (P = 0.02).
This effect was seen only in the adrenal insufficient septic shock (n=26; P=0.06), and not in the
responders to corticotropin (n = 15; P = 0.90).
- Confalonieri et al. have investigated the efficacy and safety of a 7-day treatment with intravenous
hydrocortisone (240 mg/day) in community-acquired pneumonia associated sepsis. In their study, treatment
with hydrocortisone significantly prevented onset of shock (P =0.001), reduced multiple organ dysfunction
score (P =0.003), hospital length of stay (P = 0.03), and in-hospital mortality (P = 0.009).
- In septic shock, evidence from five randomized trials suggested that prolonged treatment with
low dose corticosteroids reduced 28-day mortality (relative risk = 0.80, 95% confidence interval 0.67-0.95),
in-hospital mortality (relative risk = 0.83, 95% confidence interval 0.71-0.97), and ICU mortality (relative
risk = 0.83, 95% confidence interval 0.70-0.97). It is important, however, to note that one study accounted
for 70% of patients included in that meta-analysis. In this study, corticosteroids improved survival only in
adrenal insufficient septic shock.
- In a meta-analysis of all published randomized trials that evaluated the effects of high or low doses of
corticosteroids for short or long periods of time, there was no evidence for significant increases of
super-infection, gastroduodenal bleeding, or hyperglycemia.
- Corticosteroids could be a valuable treatment for septic shock, depending upon the way they are used.
- There is no evidence to support the use of short courses of high doses of corticosteroids in patients with
severe sepsis.
- Current evidence suggests that, in septic shock, one-week treatment with 200-300 mg of hydrocortisone
alleviates the symptoms of systemic inflammatory response, reduces the duration of shock, and
increases survival. Corticosteroids favorable effects on inflammation, hemodynamics, and survival
are more marked in patients with an increment in cortisol of 9 mg/dl or less after 250 mg of corticotrophin
(nonresponders or adrenal insufficient).](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-15-320.jpg)
![adrenocortical
insufficiency
[created by
Paul Young
03/12/07]
aetiology
diagnosis
of acute
adrenal
crisis
physiology
- The adrenal gland is a mixture of the steroid hormone-producing adrenal cortex and the
adrenal medulla, which is responsible for the secretion of catecholamines.
- The secretion of cortisol and aldosterone is controlled by different mechanisms,
whereby the pituitary axis (corticotropin-releasing hormone [CRH] or corticotropin) is
vital for cortisol secretion and the renin-angiotensin system is vital for aldosterone
secretion.
- Cortisol regulates a wide variety of genes involved in energy metabolism
(eg, glucose-protein-fatty acid metabolism), mineral homeostasis, and immune
function and influences many more cellular functions.
- Aldosterone has a more focused action on mineral homeostasis
- Although adrenal insufficiency has been known as a clinical syndrome for a long time,
new risk groups have been identified, because as many as 20% of AIDS patients
eventually develop adrenal insufficiency. Moreover, patients with head trauma develop
pituitary insufficiency much more frequently than previously recognized.
symptoms
of adrenal
insufficiency
epidemiology
- Primary and secondary adrenal insufficiency (excluding critical illness adrenal
insufficiency and adrenal insufficiency secondary to acute interruption of chronic
glucocorticoid therapy) are rare diseases, affecting less than 0.1% of the population
- usually present slowly over time with nonspecific symptoms of chronic fatigue,
weakness and lethargy, anorexia and weight loss, postural hypotension, abdominal
complaints (eg, nausea, vomiting, diffuse abdominal pain), and loss of libido as well as
loss of axillary and pubic hair in women.
- Hyperpigmentation (attributable to excess proopiomelanocortin and melanocyte-
stimulating hormone), especially of non-sunlight-exposed skin areas, is an imported
clinical hallmark for the attentive and suspicious physician.
- Abnormal serum electrolytes with low sodium, high potassium, and, occasionally,
hypercalcemia and fasting hypoglycemia, and especially this combination are highly
suspicious for adrenal insufficiency.
- Acute adrenal insufficiency (adrenal crisis) is mainly attributable to mineralocorticoid
deficiency; thus, the clinical presentation is dominated by hypotension or hypotensive shock.
treatment
- If adrenal insufficiency is confirmed or highly likely based on the acute screening
results, replacement therapy should be continued by the intravenous or intramuscular
route (at 150-300 mg/d for 2 to 3 days) until full clinical recovery. High dose cortisol
replacement has major mineralocorticoid effects therefore no additional mineralo-
corticoid therapy is needed in the acute phase.
- The 150- to 300-mg/d replacement dose of hydrocortisone is frequently considered to
be a physiologic stress dosage. However, serum cortisol levels measured after such so-
called ''acute replacement'' dosages exceed several times the maximal stress cortisol
levels found in healthy or even critically ill patients thereby questioning the need for
maintaining such high acute emergency replacement dosages.
- In contrast to the rather generous replacement dosage used in emergency situations, the
chronic replacement dosage for patients with adrenal insufficiency should be as low as
possible with clear instructions for dosage adjustments in case of stress or acute emergencies.
- Detailed information about and education of the patient and of his or her family and a
medical emergency alert card as well as appropriate follow-up should be initiated.
pathophysiology
- adrenal insufficiency is a hormone deficiency syndrome attributable to primary adrenal
diseases or caused by a wide variety of pituitary-hypothalamic disorders.
- if such diseases evolve gradually over time, they rarely cause an abrupt-onset adrenal
insufficiency crisis, whereas acute destruction of the adrenal or pituitary gland or
acute interruption of glucocorticoid therapy is more likely to cause an acute onset
adrenal failure crisis.
- there is increasing attention to relative adrenal insufficiency in patients with acute
(nonadrenal or pituitary) critical illness. Such patients still secrete cortisol (and
corticotropin in the early phases of critical illness) but less than expected during acute
stress, and the survival of such patients can be improved by pharmacologic doses of
glucocorticoids.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-16-320.jpg)




![airway
problems
in pregnancy
[created by
Paul Young
02/10/07]
general
changes
in airway in
pregnancy
- Anatomic and physiologic changes in pregnancy place parturient
patients at a greater risk for airway related complications.
- Early in pregnancy, increasing hormone levels have a major role in the
anatomic and physiologic changes of pregnancy.
- As pregnancy progresses, the gravid uterus has a significant role in the
alterations of respiratory, cardiovascular-system, and gastrointestinal functions.
(i) Weight gain
(ii) Upper airway mucosal edema
(iii) Respiratory changes with lower FRC and increased
oxygen requirements leading to decreased respiratory reserve
(iv) Breast enlargement
(v) Cardiovascular-system changes
(vi) Gastrointestinal anatomy and physiology
- Other risk factors for difficult intubation in pregnancy:
(i) Patients with preeclampsia have narrower
upper airways than do normal pregnant women
because of significant tissue edema and soft tissue
deposition in the neck
(ii) Morbid obesity](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-21-320.jpg)



![amniotic
fluid
embolism
[created by
Paul Young
02/10/07]
general
epidemiology
pathogenesis
clinical
manifestations
treatment
- Amniotic fluid embolism is a rare syndrome that can have debilitating and
lethal consequences.
- First was reported in 1926 by Meyer who described fetal cellular debris in
the maternal circulation that was associated with symptoms of hypotension
and dyspnea.
-Reported incidence ranges from as high as 1 case in 8000 deliveries to
as low as 1 case in 80,000 deliveries.
- The reported mortality rate was as high as 86% in some earlier reports;
later studies demonstrated a mortality rate of approximately 26%.
- Only 15% of survivors are neurologically intact
- It has been a common belief that the spillage of amniotic fluid in the blood
stream results in embolization of this fluid to the pulmonary vasculature, causing
acute cor pulmonale. It was believed that the microembolization of fetal products to
the pulmonary vasculature caused sudden hypoxia and cardiovascular collapse.
Evidence in the literature, however, suggests that it is not as simplistic.
- The pathophysiology of this syndrome is believed to be humoral. The clinical
picture of cardiovascular collapse, left ventricular failure, coagulopathy, and
disseminated intravascular coagulation (DIC) is believed to share common
pathways with sepsis and anaphylaxis, hence the suggested term anaphylactoid
syndrome of pregnancy.
- It is postulated that exposure to fetal products incites an immunologic response
in the mother that unleashes a cascade of mechanisms, leading to profound shock.
- Hemodynamic data corroborate the premise of a humoral cause rather than
an embolic cause. In amniotic fluid embolism, the pulmonary artery occlusion
pressure is elevated, the left ventricular stroke work index is low, the mean
pulmonary arterial pressure is increased only moderately, and the change in
central venous pressure is variable.
- The first response is an intense vasoconstriction of the pulmonary vasculature,
causing severe hypoxia, respiratory acidosis, and right heart failure. Little concrete
evidence supports this initial event, as pulmonary artery catheters may not be inserted in
this early phase. Animal studies have demonstrated this model of intense vasoconstriction
and hypoxia.
- The second phase is believed to consist of left heart failure and hemodynamic
collapse with pulmonary edema.
- The third phase in the continuum of events is neurologic dysfunction, including
seizures and coma. There may be overlapping coagulopathy and DIC.
- The clinical picture can be dramatic, with sudden acute dyspnea quickly progressing
to asystole or pulseless electrical activity. Patients who are diagnosed early enough to be
resuscitated may develop life-threatening hematologic abnormalities.
- No laboratory assays or bedside investigations can confirm the diagnosis. The
hematologic picture may show DIC, or the chest radiograph may show a diagnosis
of acute respiratory distress syndrome, but these conditions occur usually late in
the course of the illness and are not specific
- Various investigators have proposed the use of laboratory assays, such as
zinc-coproporphyrin I and monoclonal TKH-2 antibodies, but these reports are
anecdotal. There is no established role of these assays in confirming the diagnosis.
- The life-threatening evolution of an amniotic fluid embolism requires prompt
resuscitation, with airway and hemodynamic support in the critical care setting
- Less severe scenarios may present with hypotension and acute
respiratory failure. In such cases, supplemental oxygenation should be given,
and early intubation should be performed with high oxygen concentrations and
positive end-expiratory pressure, if needed, to treat refractory hypoxemia.
- The principles of treating hemodynamic collapse are similar to those of
treating sepsis. Crystalloids and vasopressors should be used to maintain an
adequate mean arterial pressure to ensure organ perfusion.
- Use of a pulmonary artery catheter may be beneficial in fluid management,
because the cardiovascular dynamics change from right-sided to left-sided
ventricular failure as the syndrome evolves.
- Hematologic manifestations are best treated by serial and frequent monitoring
of laboratory parameters, such as blood counts, fibrinogen, and coagulation &
correction of coagulopathy
- Other interventions, like steroids, antithrombin III infusion, and leukotrine
inhibitors, have been tried, but the data to support their routine use are lacking.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-25-320.jpg)
![anaemia
& blood cell
transfusion
in critical illness
general
- Anemia is a common problem in critically ill patients admitted to ICUs.
- Decisions concerning the use of RBC transfusion in the treatment of anemia and hemorrhage
require a clear understanding of the risks and the benefits of both the condition and its treatment.
- Although we have developed a much clearer appreciation of the infectious and immunomodulatory
risks of RBC transfusion over the past two decades, the risks of anemia in many clinical settings and
the benefits of RBC transfusion are still inadequately characterized.
RCTs
TRICC
- The TRICC Study documented an overall nonsignificant trend toward decreased 30-day
mortality (18.7 versus 23.3%; P = .11)
- The investigators also noted that the 30-day mortality rates were significantly lower
with the restrictive transfusion strategy among patients who were less acutely ill
(APACHE II scores less than 20) and among patients who were younger than 55 years of
age
- A number of additional questions arose from the TRICC trial. The investigators were
particularly interested in the risks and benefits of anemia and transfusion in patients with
cardiovascular disease and in patients attempting to wean from mechanical ventilation.
- In the first of these subgroup analyses, 357 patients (43%) were identified with cardiovascular
disease.
- Of these, 160 had been in the restrictive RBC transfusion group and 197 in the liberal transfusion
group.
- The two groups were fairly equally balanced with regard to baseline characteristics and
concurrent therapies, with a few exceptions: there was less frequent diuretic use in the
restrictive group (43% vs 58%; P < .01) and the use of epidural anesthetics was greater in
the restrictive group (8% vs 2%; P < .01).
- Overall, in this subgroup analysis, there was no significant difference
in the mortality rate betweenthe two treatment groups.
- However, there was a nonsignificant (P = .3) decrease in overall survival rate in the
restrictive group for patients with confirmed ischemic heart disease, severe
peripheral vascular disease, or severe comorbid cardiac disease.
- The subgroup analysis of patients receiving mechanical ventilation was limited to 713 (85%
of the 838 patients in the TRICC trial who required invasive mechanical ventilatory support).
- Of these, 357 had been in the restrictive RBC transfusion group and 356 in the liberal group.
- The mean duration of mechanical ventilation was 8.3 ± 8.1 days in the restrictive group
and 8.8 ± 8.7 days in the liberal group (P = .48). Ventilator-free days were 17.5 ± 10.9
and 16.1 ± 11.4 in the restrictive and liberal RBC transfusion groups, respectively (P = .09).
- Complications, including pulmonary edema and acute respiratory distress syndrome, were
increased in patients in the liberal strategy group
Rivers
- Subsequent to the publication of the TRICC trial, a study published by Rivers and
colleagues documented that the use of early goal-directed care based on a mixed central
venous saturation decreased mortality from 46.5% in the control group to 30.5% in the
goal-directed therapy group (P = .009).
- As one of the many interventions in patients with early septic shock, hematocrit concentrations
were increased to greater than 30% if the central venous saturations fell to less than 70%.
- As a consequence of goal-directed therapy, 64% of patients as compared with 18.5% of
the control group received RBC transfusions (P < .0001).
- The significant differences in patient populations studied by Rivers and colleagues and
the TRICC trial may account for the apparently conflicting results between the studies.
- The new finding from the early goal-directed therapy study does highlight the need to
perform additional studies in subpopulations of critically ill patients.
observational
studies
- Four large observational studies that were specifically designed to compare clinical
outcomes at varying hemoglobin concentrations in transfused and nontransfused patients
have been conducted in various clinical settings.
- In the first of these, Hébert and colleagues used a combined retrospective and
prospective cohort design to examine 4470 critically ill patients admitted to six Canadian
tertiary-level ICUs during 1993.
- In patients with cardiac diagnoses (ischemic heart disease, arrhythmia, cardiac arrest, or
cardiac and vascular surgical procedures), there was a trend toward increased mortality
when hemoglobin concentrations were less than 95 g/L.
- analysis of a subgroup of 202 patients with anemia, an Acute Physiology and Chronic
Health Evaluation (APACHE) II score greater than 20, and a cardiac diagnosis revealed
that transfusion of 1 to 3 units or 4 to 6 units of RBCs was associated with a significantly
lower mortality rate as compared with those patients who did not receive a transfusion
(55% [no transfusions] versus 35% [1 to 3 units] or 32% [4 to 6 units]; P = .01).
- Wu and associates retrospectively studied Medicare records of 78,974 patients older
than 65 years who were hospitalized with a primary diagnosis of acute myocardial
infarction.
- The authors then categorized patients according to their admitting hematocrit. Although
anemia, defined in the study as a hematocrit less than 39%, was present in nearly half the
patients, only 3680 patients received an RBC transfusion.
- Lower admission hematocrit values were associated with increased 30-day mortality
rate with a mortality rate approaching 50% among patients with a hematocrit of 27% or
lower who did not receive an RBC transfusion.
- RBC transfusion was associated with a reduction in 30-day mortality for patients who
received at least one RBC transfusion if their admitting hematocrit was less than 33%,
whereas RBC transfusion was associated with increased 30-day mortality for patients
whose admitting hematocrit values were 36.1% or higher.
- In the only study exclusively focusing on the perioperative period, Carson and associates attempted
to determine the effect of perioperative transfusion on 30- and 90-day post-operative mortality with a
retrospective cohort study involving 8787 patients with hip fractures undergoing repair between 1983
and 1993 in 20 different U.S. hospitals.
- This was a large, high-risk, elderly (median age, 80.3 years) population with extensive coexisting
disease and with an overall 30-day mortality rate of 4.6%.
- A total of 3699 patients (42%) received a perioperative transfusion within 7 days of the surgical repair.
- After controlling for trigger hemoglobin concentrations, cardiovascular disease, and other risk factors
for death, the results suggested that patients who had hemoglobin concentrations as low as 80 g/L and
did not receive transfusion were no more likely to die than those with similar hemoglobin concentration
levels who received a transfusion. (With hemoglobin concentrations less than 80 g/L, nearly all patients
received a transfusion, so investigators were unable to draw conclusions about the effect of transfusion
at these lower hemoglobin concentrations levels.)
- More recently, Vincent and coworkers completed a prospective observational cross-sectional study
involving 3534 patients admitted to 146 western European ICUs during a 2-week period in November 1999.
- Thirty-seven percent of these patients received an RBC transfusion during their ICU admission, with
the overall transfusion rate increasing to 41.6% over a 28-day period. For those patients who received a
transfusion, the mean pretransfusion hemoglobin concentration was 84 ±13 g/L.
- In an effort to control for confounding factors created by illness severity and the need for transfusion,
these investigators used a strategy of matching transfused and non transfused patients based on their
propensity to receive a transfusion, thereby defining two well-balanced groups (516 patients in each group)
to determine the influence of RBC transfusions on mortality.
- Using this approach, the associated risk of death was increased instead of decreased by 33% for patients
who received a transfusion as compared with similar patients who did not receive blood.
- A number of studies have attempted to answer the question of the impact of blood
transfusion on outcomes in patients with anemia and acute coronary syndromes (ACS). -
- Rao and colleagues recently addressed this issue by examining the data from three large clinical trials
of anticoagulants (GUSTO) and glycoprotein IIb/IIIa inhibitors (PURSUITand PARAGON) in patients with ACS.
Note that in these trials, blood transfusion was a post-randomization event, and transfusions were given at the
discretion of the treating clinicians. - The combined data included over 24,000 patients with ACS with information
on blood transfusions, anemia and bleeding. Of these patients, 10% were transfused at least 1 unit of whole blood
or packed red blood cells (PRBCs) during their hospitalization.
- The groups were dissimilar, in that the transfused patients were older, more likely to have diabetes mellitus,
hypertension, or hyperlipidemia, to have prior stroke or congestive heart failure, and to be female, than those
who did not receive transfusion. In addition, while the transfusion and no transfusion groups had an equal
percentage of patients with ST-segment elevation at presentation, the transfused group had a higher
percentage of patients with ST-segment depression and were more likely to be Killip class = II.
- These studies when adjusted for baseline differences between groups suggest that blood transfusion in
patients with ACS is associated with worse outcome, especially in those who are not anemic or have mild anemia
(HCT > 25%).
natural
history of
anaemia
General:
- Numerous laboratory experiments indicate that extreme hemodilution is well tolerated
in healthy animals. Animals subjected to acute hemodilution tolerate decreasing
hemoglobin concentrations down to 50 to 30 g/L, with ischemic electrocardiographic
changes and depressed ventricular function, occurring, respectively, at these levels of
hemoglobin concentration.
- acute hemodilution is less well tolerated in experimental animal models of coronary
stenosis, with ischemic electrocardiographic changes and depressed cardiac function
occurring at hemoglobin concentrations between 70 and 100 g/L.
- Human data regarding the limits of anemia tolerance are inadequate and often
conflicting
- From a systematic review completed for the Canadian Guidelines on Red cells, Hébert
and associates identified numerous reports of severe anemia being well tolerated in
surgical patients
Specific high risk conditions:
- A number of risk factors for adverse outcomes associated with anemia have been
identified in clinical practice guidelines and reviews. Anemia is believed to be less
tolerated in:
(i) older patients,
(ii) in the severely ill, and
(iii) in patients with clinical conditions such as coronary, cerebrovascular, or respiratory disease.
- However, the clinical evidence confirming that these factors are independently
associated with an increased risk of adverse outcome is lacking
Coronary artery disease:
- One small case-control study following high-risk vascular surgery suggests an increase
in postoperative cardiac events with increasing severity of anemia.
- In perioperative and critically ill patients, two large cohort studies have documented that
increasing degrees of anemia were associated with a disproportionate increase in
mortality rate in the subgroup of patients with cardiac disease](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-26-320.jpg)


![antibiotic
allergy
[created
by Paul
Young
06/01/08]
general
- Antibiotic hypersensitivity is common, and most frequently involves beta lactams.
- Some instances of ‘pseudo-allergy’ (eg anaphylactoid responses to vancomycin
infusions such as ‘red-man syndrome’) involve direct release of vasoactive mediators
by non-IgE mechanisms. While not truly allergic, these latter responses may be ameliorated
by preventive antihistamines, in combination with slowing of the infusion rate.
- Drug allergy is more commonly seen with certain infections, particularly with HIV and
Epstein-Barr virus infections, and allergic reactions are more likely to be severe in individuals
receiving beta-blocker therapy.
- While many nonspecific reactions are labelled as ‘allergic’, true type I (IgE-mediated)
antibiotic hypersensitivity is strongly suggested by the development of urticaria,
angioedema, bronchospasm, or anaphylaxis (with objectively demonstrated hypotension,
hypoxia or tryptase elevation) within one hour of drug administration.
diagnosis
- Antibiotic hypersensitivity is usually diagnosed on the basis of clinical history,
with oral challenging judiciously employed where skin tests (if performed) are
negative, or in circumstances where alternative drugs are clearly inferior.
- In these cases, the degree of suspicion surrounding possible life-threatening
reactivity will dictate whether a desensitisation protocol is preferable to oral challenge.
- The confirmation of antibiotic hypersensitivity is difficult, as no currently available
skin or blood test offers 100% negative predictive value for drug allergy.
- Due to changing availability of penicillin skin test reagent mixes, skin testing has a
significant false negative rate (3% to 20%) even in the setting of true penicillin allergy.
- In cases of suspected drug allergy, elevation of mast cell tryptase measured on a
serum sample collected between 1 and 6 hours after a clinical reaction is highly
specific for an episode of mast cell degranulation.
penicillin
hypersensitivity
- Between 1% and 10% of beta-lactam courses result in manifestations interpreted
as due to hypersensitivity.
- Most reactions are late, non-IgE mediated and involve skin rash.
- Other later manifestations include fever, haemolysis and serum sickness-like reactions.
- The minority of reactions are immediate hypersensitivity reactions. Anaphylactic
responses to penicillin occur approximately once every 10 000 courses administered,
with 10% of these reactions being fatal, most often associated with parenteral rather
than oral administration.
- Most of these reactions occur in people without a history of prior penicillin allergy.
- Notwithstanding this, a detailed history of penicillin reaction should always be sought
before a course of penicillin is commenced.
- Late manifestations are only a relative contraindication. Rashes, especially with
amoxy/ampicillin, are much less predictive of future reactions and repeat exposure to
beta-lactam drugs is not necessarily contraindicated.
- A history of an immediate hypersensitivity reaction (urticaria, angioedema, bronchospasm,
or anaphylaxis within one hour of drug administration) or other life-threatening reactions
(eg Stevens-Johnson syndrome) contraindicates further exposure to penicillin and other
beta lactams apart from aztreonam.
- Between 3% and 10% of patients hypersensitive to penicillin exhibit cross-reactivity with
cephalosporins and carbapenems.
- A patient with a known beta-lactam hypersensitivity should be encouraged to wear an alert
bracelet or necklace containing this information.
- In the unusual circumstance that it is necessary to use a penicillin, expert advice should be
sought on desensitisation, or a test dose of penicillin should be given under controlled conditions
to reduce the risk in this situation.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-29-320.jpg)


![antiphospholipid
syndrome
[created by
Paul Young
02/10/07]
general
- Antiphospholipid antibodies are a heterogeneous group
of autoantibodies directed against phospholipid binding
proteins.
- Antiphospholipid antibodies can be broadly categorized into:
(i) those antibodies that prolong phospholipid-dependent coagulation
assays, known as lupus anticoagulants (LA), or
(ii) anticardiolipin antibodies (aCL)
- The presence of these antibodies in patients with arterial or
venous thrombosis or pregnancy morbidity comprises the
antiphospholipid antibody syndrome (APS).
- This syndrome is referred to as:
(i) primary APS when it occurs alone and
(ii) secondary APS when it occurs in association with
other conditions, such as systemic lupus erythematosus (SLE).
- Antiphospholipid antibodies are also found in patients with
infections such as human immunodeficiency virus2 and may
develop during therapy with medications such as chlorpromazine.
Their clinical importance in these settings is unknown.
treatment
lupus
anticoagulants
- Lupus anticoagulants are antibodies that block
phospholipid surfaces important for coagulation.
(i) increase APTT
(ii) prolonged APTT does not correct with
a 1:1 mix with normal platelet-free plasma
(iii) correction of the clotting time after addition of
excess phospholipids confirms the presence of LA.
- Consensus guidelines recommend screening for LA with 2 or
more phospholipid-dependent coagulation tests, including the
(i) activated partial thromboplastin time,
(ii) dilute Russell viper venom time,
(iii) kaolin clotting time,
(iv) dilute prothrombin time,
(v) textarin time or
(vi) taipan time
anticardiolipin
antibodies
- Anticardiolipin antibodies share a common in vitro binding
affinity for cardiolipin and can be detected using ELISA.
diagnostic
criteria for
antiphospholipid
syndrome
- According to the Sapporo criteria, APS is present
in patients with 1 clinical and 1 laboratory criterion.
- Clinical criteria include:
(i) objectively confirmed arterial, venous, or small-vessel thrombosis,
(ii) pregnancy morbidity consisting of recurrent fetal loss before the 10th
week of gestation, 1 or more unexplained fetal death at or beyond the 10th
week of gestation, or premature birth due to placental insufficiency, eclampsia,
or preeclampsia.
- Laboratory criteria include:
(i) medium or high titer IgG or IgM aCL or
(ii) the presence of LA on 2 or more occasions at least 6 weeks apart.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-32-320.jpg)
![antivirals
adefovir
- Adefovir is a nucleotide analogue of adenosine with activity against the
hepatitis B virus.
- It is taken orally as a prodrug (adefovir dipivoxil) and is active against wild
type hepatitis B virus and lamivudine-resistant variants.
- The most common adverse effect of adefovir is gastric intolerance.
- It can cause renal impairment.
- Adefovir is eliminated predominantly by renal excretion with a half-life of
about 8 hours in patients with normal kidney function. Reduced dosage
frequency is required in renal impairment.
amantadine
- Amantadine is occasionally used for influenza A prophylaxis or early treatment.
- Amantadine is also used in Parkinson's disease.
- It has antimuscarinic and weak dopamine agonist properties and may also work
as a glutamate antagonist.
- Its elimination depends on renal clearance and the dose should be reduced in
renal impairment.
- Most adverse effects are dose-related and relatively mild in doses of 100 to
200 mg per day. The adverse effect profile closely resembles that of an
anticholinergic drug, namely dry mouth, constipation, blurred vision and urinary
retention.
- Rarely it causes hallucinations and confusion; delirium can develop in elderly
patients with renal impairment. At least 50% of patients develop the peculiar
skin mottling known as livedo reticularis, and 5% to 10% develop ankle oedema
unrelated to congestive heart failure, renal failure or hypoalbuminaemia.
antiretrovirals
- Antiretroviral drugs are used in combination regimens, usually comprising
2 nucleoside/nucleotide reverse transcriptase inhibitors and a protease
inhibitor or non-nucleoside reverse transcriptase inhibitor (highly active
antiretroviral therapy [HAART]).
- These drugs must not be used as single drugs because of the potential for
rapid development of resistance. They decrease viral load and increase CD4
cell counts in patients with HIV infection.
nucleoside / nucleotide reverse transcriptase inhibitors
protease inhibitors
cidofovir
- Cidofovir is used intravenously for cytomegalovirus infection.
- It requires co-administration with probenecid (before and after infusion)
to reduce nephrotoxicity.
- Major contraindications for cidofovir are pregnancy, moderate to severe
renal impairment and co-administration of other nephrotoxic agents (eg foscarnet).
foscarnet
- Foscarnet is given by intravenous infusion for cytomegalovirus infection in
immunocompromised patients.
- Acute renal failure is a common adverse effect.
- Dosage adjustment is required in renal impairment.
- It should not be co-administered with intravenous pentamidine.
guanine
analogues
- Valganciclovir, a prodrug of ganciclovir, is well absorbed when taken orally
and is then hydrolysed to ganciclovir. It is as effective as intravenous
ganciclovir for treatment of CMV retinitis in AIDS patients and is used for CMV
prophylaxis in selected solid organ transplant recipients.
- Aciclovir, famciclovir and valaciclovir are active against herpes simplex
and varicella-zoster virus.
- Aciclovir is absorbed poorly and erratically from the gut, and even less
through the skin. Intravenous doses should be administered slowly.
- Famciclovir is a prodrug of penciclovir and is well absorbed from the gut.
- Famciclovir and valaciclovir require fewer daily doses. They are all
generally well tolerated.
- Valaciclovir, a prodrug of aciclovir, has improved bioavailability compared
with aciclovir.
- Ganciclovir is used intravenously for the treatment of serious CMV
infection in immunocompromised patients. It has dose-dependent bone
marrow suppressive effects.
- Intraocular implants or injections can be used in the management of CMV
retinitis.
interferons
- Interferons are naturally occurring proteins that belong to the family of cytokines
and are released in vivo in response to viral infections. Three major classes have
been identified: alfa, beta and gamma.
- After binding to specific cell receptors, interferons lead to increased synthesis of
a range of proteins that enhance the cell's immune response to a virus.
- Five interferons have been synthesised and are available for therapeutic use for
conditions such as multiple sclerosis, hairy-cell leukaemia, multiple myeloma and
chronic granulomatous disease.
- Interferon alfa-2a and interferon alfa-2b are used in the treatment of chronic
hepatitis B and C.
- Some patients develop antibodies to interferon after prolonged use and this may
reduce its efficacy.
- Influenza-like symptoms can usually be managed with paracetamol.
- Neuropsychiatric effects such as depression, anxiety, emotional lability, somnolence
and forgetfulness are frequent. Interferons can precipitate psychiatric disorders,
especially depression and anxiety, and should be used with caution in patients with
a history of these disorders.
- Interferons can cause serious thyroid dysfunction and therefore thyroid function
tests should be performed before, and every 3 months during, therapy.
- Transient bone marrow suppression (neutropenia and thrombocytopenia) can
require dose reduction. Blood counts should be checked at least monthly.
- Common adverse effects are influenza-like symptoms, anorexia and weight loss.
- Interferons can exacerbate hepatitis in patients with cirrhosis and cause hepatic
decompensation. Therapy should be ceased if alanine aminotransferase (ALT)
increases despite dose reduction, or is accompanied by increased bilirubin or
evidence of hepatic decompensation.
Lamivudine
- a nucleoside reverse transcriptase inhibitor developed for treating HIV.
- It is also used in the treatment of chronic hepatitis B in those with evidence
of hepatitis B virus replication.
- It is given orally and adverse effects are uncommon.
- When used as monotherapy for hepatitis B, the major limitation of lamivudine
is the development of viral resistance (69% after 4 years).
neuraminidase
inhibitors
- Oseltamivir (oral) and zanamivir (inhaled) are both inhibitors of influenza
virus A and B neuraminidase, which is essential for replication of the virus.
- If started within 48 hours after symptom onset, they may shorten symptom
duration (by approximately one day). The drugs may be used as prophylaxis
in institutions (eg nursing homes), to minimise the spread of infection.
- Zanamivir should be used with caution in people with asthma or chronic
obstructive pulmonary disease because bronchospasm may be exacerbated.
ribavirin
- Ribavirin has a broad antiviral spectrum, inhibiting the replication of a wide range
of RNA and DNA viruses.
- It is a nucleoside analogue used in the treatment of chronic hepatitis C in combination
with peginterferon alfa or interferon alfa.
- It has also been used to treat certain haemorrhagic fevers and severe measles
infection in immunocompromised patients, and serious lower respiratory tract infection
with respiratory syncytial virus (RSV) in hospitalised children.
- Haemolytic anaemia is a common adverse effect.
- Frequent monitoring and dose reduction may be required (particularly in the first 6 weeks).
- It is contraindicated in patients with haemoglobinopathies or those requiring dialysis.
- Caution is required in patients with, or suspected of having, ischaemic heart disease.
- Blood counts must be monitored on a regular basis along with serum electrolytes and
creatinine.
- Skin rashes are occasionally seen early in treatment (10% to 15% of cases), but are
usually mild and may not require cessation of therapy.
- Ribavirin is embryotoxic or teratogenic, or both, at doses well below the recommended
human dose in all animal species studied.
- It is also genotoxic (mutagenic) and reversibly impairs spermatogenesis. It accumulates
intracellularly and its half-life in humans is approximately 12 days. Therefore Ribavirin is
contraindicated in women who are pregnant or who may become pregnant during exposure.
- It is contraindicated in men whose partner is fertile unless both are using effective
contraception.
- Pregnancy should be avoided until 6 months after completion of therapy.
- A man whose partner is already pregnant should use condoms, as it is not known if the
concentration in sperm may affect the fetus.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-33-320.jpg)
![aortic
dissection
[created by
Paul Young
02/10/07]
defn
the most common catastrophe of the aorta
symptoms
signs
1. chest pain is the most frequent presenting complaint:
- may be ripping or tearing in nature
- pain may migrate
- chest pain is of sudden onset (a key feature in distinguishing it from ischaemic pain)
- maximal at onset
- location of pain may indicate where the dissection arises (anterior chest pain is
associated with anterior dissection & may result in part from coronary occlusion;
jaw or neck pain occurs with extension into the great vessels; interscapular pain
occurs with dissection of the descending aorta)
1. Blood pressure:
- may increase or decrease
- hypotension is an ominous sign and may result from excessive vagal
tone, cardiac tamponade or hypovolaemia from rupture of dissection
- 20mmHg differential in an independent predictor of aortic dissection
2. Neurological deficits:
- peripheral nerve ischaemia can cause numbness & tingling in the extremities
- hoarseness from recurrent laryngeal nerve compression has been described
- Horners syndrome
3. SVC syndrome
- may occur from compression of SVC by aorta
4. cardiac tamponade
5. new diastolic murmur
6. assymetrical pulses (carotid, brachial and femoral)
7. findings of haemothorax if ruptures
investigation
1. bloods:
- leukocytosis may be present
- Cr is elevated if dissection involves the renal arteries
- Trop is elevated if dissection has caused myocardial ischaemia
- decreased Hb suggests leak or rupture
- a -ve D-dimer makes diagnosis very unlikely
- X-match
treatment
1. Oxygen & large bore iv access
2. Pain relief
3. Initiate aggressive management of heart rate
& blood pressure (HR<60-80 & BP <100-120 systolic)
4. urgent surgical intervention is indicated for type A dissection
5. type B dissection may be managed surgically, radiologically or medically
disposition
- untreated 33% die in 24hrs, 50% within 48hrs & mortality approaches
75% in patients with undiagnosed ascending aortic dissection
2-3Xs more common than rupture of the abdominal aorta
aetiology
Classification:
(i) Stanford classification:
- type A involves the ascending aorta
- type B does not involve the ascending aorta
(ii) DeBakey classification
- type I involves ascending aorta, arch & descending aorta
- type II is confined to the arch
- type III is confined to the descending aorta distal to the left subclavian artery
Pathophysiology:
- breakdown of collagen, elastin and smooth muscle (cystic medial necrosis) occurs
with aging, occlusive atherosclerosis of the vasavasorum & Marfan syndrome
Risk factors:
(i) CT disorders (Marfans, Ehlers-Danlos, adult polycystic kidney disease)
(ii) vascular disease risk factors (smoking, hypertension, dylipidaemia)
(iii) structural anomalies (bicuspid aortic valve, coarctation)
(iv) pregnancy increases risk
(v) syphillus
(vi) recent cardiac catherisation increases risk of iatrogenic dissection
2. other presenting symptoms include:
- neurological symptoms
- syncope
- altered mental status
- limb paraesthesias, pain or weakness
- dyspnoea (from tracheobronchial compression)
- dysphagia (from oesophageal compression)
- orthopnoea
- flank pain if the renal artery is involved
- dyspnoea and haemoptusis if the dissection ruptures into the pleura
2. imaging:
(i) plain radiography
- mediastinal widening of greater than 8cm on AP chest radiograph
- blunted aortic knuckle
- ring sign (displacement of aorta >5mm past calcified intima is specific)
- left apical cap
- tracheal deviation
- deviation of the left mainstem bronchus
- oesophageal deviation
- loss of paratracheal stripe
(ii) CT aortogram
- advantages are that it details the anatomy and helps surgical planning
- disadvantages are transport of unstable patient out of ED, need for
contrast often with impaired renal function
(iii) echocardiography
- TTE is good for evaluating AR and tamponade; it is less senstive than CT
- TOE is advantageous because patient does not need to be transported
& because it detects involvement of the coronaries, AR & tamponade; it
can give false positives and false negatives due to fact upper ascending
aorta and arch may not be well visualised
(iv) MRI and angiography
3. ECG:
- ST elevation occurs with coronary involvement
- right coronary dissects most commonly
- mortality is 1-2% per hour for the first 24-48 hours
initial consultation with cardiology & later with cardiothoracic surgeon](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-34-320.jpg)
![approach
to ABG
analysis
[created
by Paul
Young
14/12/07]
1 pH:
- Check
arterial
pH
Principle:
- The net deviation in pH will indicate whether an acidosis or an alkalosis is present
Guidelines:
- IF an acidaemia is present THEN an acidosis must be present
- IF an alkalaemia is present THEN an alkalosis must be present
- IF pH is normal pH THEN Either (no acid-base disorder is present) or (Compensating
disorders are present ie a mixed disorder with an acidosis and an alkalosis)
2. assess
the
pattern
Principle:
- Each of the simple disorders produces predictable changes in [HCO3] & pCO2.
Guidelines:
- IF Both [HCO3] & pCO2 are low THEN Suggests presence of either a Metabolic
Acidosis or a Respiratory Alkalosis (but a mixed disorder cannot be excluded)
- IF Both [HCO3] & pCO2 are high THEN Suggests presence of either a Metabolic
Alkalosis or a Respiratory Acidosis (but a mixed disorder cannot be excluded)
- IF [HCO3] & pCO2 move in opposite directions THEN a mixed disorder MUST be present
3. look
for
associated
clues
Principle:
- Certain disorders are associated with predictable changes in other biochemistry results
Guidelines:
(i) High anion gap
- Always strongly suggests a metabolic acidosis.
(ii) Hyperglycaemia
- If ketones also present in urine -> diabetic ketoacidosis
(iii) Hypokalaemia and/or hypochloraemia
- Suggests metabolic alkalosis
(iv) Hyperchloraemia
- Common with normal anion gap acidosis
(v) Elevated creatinine and urea
- Suggests uraemic acidosis or hypovolaemia (prerenal renal failure)
- With an elevated creatinine consider ketoacidosis: ketones interfere in the
laboratory method (Jaffe reaction) used for creatinine measurement & give a
falsely elevated result; typically urea will be normal.
(vi) Elevated glucose
- Consider ketoacidosis or hyperosmolar non-ketotic syndrome
(vii) Urine dipstick tests for glucose and ketones
- Glucose detected if hyperglycaemia; ketones detected if ketoacidosis
4. assess
the
compensatory
response
Rule 1 : The 1 for 10 Rule for Acute Respiratory Acidosis
- The [HCO3] will increase by 1 mmol/l for every 10 mmHg elevation in pCO2 above 40 mmHg.
Expected [HCO3] = 24 + { (Actual pCO2 - 40) / 10 }
- The increase in CO2 shifts the equilibrium between CO2 and HCO3 to result in an acute
increase in HCO3. This is a simple physicochemical event and occurs almost immediately.
Rule 2 : The 4 for 10 Rule for Chronic Respiratory Acidosis
- The [HCO3] will increase by 4 mmol/l for every 10 mmHg elevation in pCO2 above 40mmHg.
Expected [HCO3] = 24 + 4 { (Actual pCO2 - 40) / 10}
- With chronic acidosis, the kidneys respond by retaining HCO3, that is, renal
compensation occurs. This takes a few days to reach its maximal value.
Rule 3 : The 2 for 10 Rule for Acute Respiratory Alkalosis
- The [HCO3] will decrease by 2 mmol/l for every 10 mmHg decrease in pCO2 below 40 mmHg.
Expected [HCO3] = 24 - 2 { ( 40 - Actual pCO2) / 10 }
- In practice, this acute physicochemical change rarely results in a [HCO3] of less than about
18 mmol/s. (After all there is a limit to how low pCO2 can fall as negative values are not possible!)
So a [HCO3] of less than 18 mmol/l indicates a coexisting metabolic acidosis.
Rule 4 : The 5 for 10 Rule for a Chronic Respiratory Alkalosis
- The [HCO3] will decrease by 5 mmol/l for every 10 mmHg decrease in pCO2 below 40 mmHg.
Expected [HCO3] = 24 - 5 { ( 40 - Actual pCO2 ) / 10 } ( range: +/- 2)
- It takes 2 to 3 days to reach maximal renal compensation
- The limit of compensation is a [HCO3] of about 12 to 15 mmol/l
Rule 5 : The One & a Half plus 8 Rule - for a Metabolic Acidosis
- The expected pCO2 (in mmHg) is calculated from the following formula:
Expected pCO2 = 1.5 x [HCO3] + 8 (range: +/- 2)
- Maximal compensation may take 12-24 hours to reach
- The limit of compensation is a pCO2 of about 10 mmHg
- Hypoxia can increase the amount of peripheral chemoreceptor stimulation
Rule 6 : The Point Seven plus Twenty Rule - for a Metabolic Alkalosis
- The expected pCO2(in mmHg) is calculated from the following formula:
Expected pCO2 = 0.7 [HCO3] + 20 (range: +/- 5)
- The variation in pCO2 predicted by this equation is relatively large.
5. check
additional
indices
for metabolic
acidoses
anion gap
- An elevated Anion Gap always strongly suggests a Metabolic Acidosis.
- the 'normal anion gap depends on the serum phosphate and the serum albumin.
anion gap = 0.2 x [albumin] (g/L) + 1.5 x [phosphate] (mmol/L)
- If AG is 20-30 then high chance (67%) of metabolic acidosis
- If AG is > 30 then a metabolic acidosis is definitely present
causes of raised anion gap are MUDPILES
causes of a normal anion gap are USED CRAP
causes of a low anion gap are:
(i) decreased unmeasured anions (albumin, dilution)
(ii) increased unmeasured cation (multiple myeloma, hypercalcaemia,
hypermagnesaemia, acute lithium overdose, polymixin B)
(iii) non random analytical errors (increased sodium, increased
viscosity, iodide ingestion, increased lipids)
Delta Ratio
< 0.4 - Hyperchloraemic normal anion gap acidosis
0.4 to 0.8 - Combined high AG and normal AG acidosis
1 - Common in DKA due to urinary ketone loss
1 to 2 - Typical pattern in high anion gap metabolic acidosis
> 2 Check for either a co-existing Metabolic Alkalosis (which would elevate [HCO3]) or a
co-existing Chronic Respiratory Acidosis (which results in compensatory elevation of [HCO3])](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-35-320.jpg)





![aspiration
syndromes
aspiration
pneumonia
General
- Aspiration pneumonia develops after the aspiration of colonized oropharyngeal
contents. Aspiration of pathogens from a previously colonized oropharynx is the primary
pathway by which bacteria gain entrance to the lungs.
- For initial treatment of aspiration pneumonia, use:
benzylpenicillin 1.2 g (child: 30 mg/kg up to 1.2 g) IV, 6-hourly
PLUS
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 12-hourly
or metronidazole 400 mg (child: 10 mg/kg up to 400 mg) orally, 12-hourly.
- Alternatively, or in patients with immediate penicillin hypersensitivity, as a
single drug use:
clindamycin 450 mg (child: 10 mg/kg up to 450 mg) IV or orally, 8-hourly
OR
lincomycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly.
- Aerobic Gram-negative bacilli are uncommon causes of aspiration pneumonia,
despite frequent appearance on Gram stains of sputum. If Gram-negative pneumonia
is suspected (eg in alcoholic patients), use:
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 12-hourly
or metronidazole 400 mg (child: 10 mg/kg up to 400 mg) orally, 12-hourly
PLUS EITHER
ceftriaxone 1 g (child: 25 mg/kg up to 1 g) IV, daily
OR
cefotaxime 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly
OR (as a single preparation)
piperacillin+tazobactam 4+0.5 g (child: 100+12.5 mg/kg up to 4+0.5 g) IV, 8-hourly
OR
ticarcillin+clavulanate 3+0.1 g (child: 50+1.7 mg/kg up to 3+0.1 g) IV, 6-hourly.
- If infection with Staphylococcus aureus is suspected or proven, see Staphylococcal
pneumonia.
- Switch to oral therapy after there has been significant improvement (eg when fever
and/or other objective signs are resolving), and the patient is able to tolerate oral medication.
Use:
amoxycillin+clavulanate 875+125 mg (child: 22.5+3.2 mg/kg up to 875+125 mg) orally, 12-hourly.
- In patients with penicillin hypersensitivity, use:
clindamycin 450 mg (child: 10 mg/kg up to 450 mg) orally, 8-hourly.
- For uncomplicated aspiration pneumonia, 7 days of therapy is usually adequate, but
extensive disease or abscess formation may require more prolonged high-dose therapy
and/or surgery
aspiration
pneumonitis
risk factors
for aspiration
during
endotracheal
intubation:
Definition:
- Aspiration pneumonitis is best defined as acute lung injury after the aspiration
of regurgitated gastric contents.
pathogenesis:
- aspiration of gastric contents results in a chemical burn of the tracheobronchial tree
and pulmonary parenchyma with an intense parenchymal inflammatory reaction.
the role of bacteria:
- Gastric acid prevents the growth of bacteria, and thus the contents of the stomach are
normally sterile. Bacterial infection, therefore, does not play a significant role in the early
stages of acute lung injury after aspiration of gastric contents.
- Bacterial superinfection may occur at a later stage; however, the incidence of this
complication has not been studied.
- Colonization of the gastric contents by potentially pathogenic organisms may occur
when the gastric pH is increased by the use of antacids, H2 blockers, or proton pump
inhibitors. In addition, gastric colonization by gram-negative bacteria occurs in patients
receiving gastric enteral feedings, as well as in patients with gastroparesis and small
bowel obstruction. In these circumstances the pulmonary inflammatory response is likely
to result from both bacterial infection and the inflammatory response of the gastric
particulate matter.
clinical manifestations:
- Aspiration of gastric contents can present dramatically with a full-blown picture that
includes gastric contents in the oropharynx, wheezing, coughing, shortness of breath,
cyanosis, pulmonary edema, hypotension, and hypoxemia, which may progress rapidly to
severe acute respiratory distress syndrome (ARDS) and death.
- Many patients may not develop signs or symptoms associated with aspiration, whereas
others may develop a cough or wheeze.
- In some patients aspiration may be clinically silent, manifesting only as arterial desaturation
with radiologic evidence of aspiration.
use of antimicrobials
- While common practice, the prophylactic use of antibiotics in patients with suspected or
witnessed aspiration is not recommended. Similarly, the use of antibiotics shortly after an
aspiration episode in a patient who develops a fever, leukocytosis, and a pulmonary
infiltrate is discouraged because it may select for more resistant organisms in a patient
with an uncomplicated chemical pneumonitis.
- empirical antimicrobial therapy is appropriate in patients who aspirate gastric contents
in the setting of small bowel obstruction or in other circumstances associated with
colonization of gastric contents.
- Antimicrobial therapy should be considered in patients with an aspiration pneumonitis
that fails to resolve within 48 hours. Empirical therapy with broad-spectrum agents is
recommended.
- Lower respiratory tract sampling in intubated patients may allow targeted antimicrobial
therapy and the discontinuation of antibiotics in culture-negative patients.
Pathogenesis:
- Any condition that increases the volume and/or bacterial burden of oropharyngeal secretion
in the setting of impaired host defense mechanism may lead to aspiration pneumonia.
- Colonization of the oropharynx is another important step in the pathogenesis of
aspiration pneumonia. The elderly have increased oropharyngeal colonization with
pathogens such as Staphylococcus aureus and aerobic gram-negative bacilli (e.g.,
Klebsiella pneumoniae and Escherichia coli).
- Dysphagia is a key risk factor & commonly develops in the setting of stroke or
neurodegenerative disease
lung
abscess
- Lung abscesses usually develop either as a result of aspiration of organisms
in patients with dental caries, aspiration of foreign bodies (eg a tooth, a peanut),
or as a consequence of severe necrotising pneumonia.
- Patients with altered conscious states (eg from anaesthesia, or alcohol intoxication,
or postictal) and/or with swallowing difficulties are at particular risk. Septic emboli
are occasionally a cause in intravenous drug users, often with right-sided endocarditis.
- Lung abscesses can also be a consequence of septic thrombophlebitis of pelvic or
internal jugular veins (Lemierre syndrome).
- If the cause is necrotising pneumonia, pathogens such as Staphylococcus aureus
(eg post-influenza) and Klebsiella pneumoniae should be considered.
- Infection of pre-existing bullae in a patient with emphysema can masquerade as a
primary lung abscess.
- Tumours, vasculitis and tuberculosis can also present as solitary cavitating pulmonary lesions.
- Where possible, attempts should be made to identify the causal organism.
- Bronchoscopy or fine needle aspiration may be needed to obtain diagnostic specimens or
remove a foreign body.
- If the abscess has clearly cavitated and the patient has a productive cough, the
abscess is probably draining into the airways, and antibiotics and physiotherapy should
be sufficient. If that is not the case, drainage of the abscess via a percutaneous
catheter (eg inserted under ultrasound or computerised tomography [CT] guidance) is
recommended.
- For empirical antibiotic therapy (after obtaining appropriate cultures), see recommendations
for aspiration pneumonia.
- Antibiotic therapy is generally required for at least 10 to 14 days, but should be continued until
the patient’s sputum is no longer purulent and the abscess cavity is free of fluid (in some cases
this may require up to 4 weeks of treatment).
Clinical features:
- In patients with aspiration pneumonia, unlike the case of aspiration pneumonitis, the
episode of aspiration is generally not witnessed. The diagnosis is therefore inferred when
a patient with known risk factors for aspiration has an infiltrate in a characteristic
bronchopulmonary segment.
- In patients who aspirate in the recumbent position the most common sites of
involvement are the posterior segments of the upper lobes and the apical segments of the
lower lobes. In patients who aspirate in the upright or semi-recumbent position the basal
segments of the lower lobes are favored.
- The usual picture is that of an acute pneumonic process, which runs a course similar to
that of a typical CAP. If untreated, however, these patients appear to have a higher
incidence of cavitation and lung abscess formation.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-41-320.jpg)



![bacterial
meningitis
- directed
therapy
[created
by Paul
Young
27/11/07]
Meningococcal meningitis:
- for Neisseria meningitidis (meningococcal meningitis), use:
(i) benzylpenicillin 1.8 g (child: 45 mg/kg up to 1.8 g) IV, 4-hourly for 3 to 5 days.
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity), use:
(i) ceftriaxone 4 g (child: 100 mg/kg up to 4 g) IV, daily for 3 to 5 days
or ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV, 12-hourly for 3 to 5 days
OR
(ii) cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly for 3 to 5 days.
- For patients with immediate penicillin or cephalosporin hypersensitivity, use:
(i) ciprofloxacin 400 mg (child: 10 mg/kg up to 400 mg) IV, 12 hourly for 3 to 5 days.
- Prophylaxis and/or immunisation is essential for close contacts (see chemoprophylaxis
for meningitis). Prophylaxis is also necessary for patients who have received only
benzylpenicillin, since this does not reliably clear nasal carriage.
Streptococcus pneumonia meningitis:
- MICs to penicillin and ceftriaxone/cefotaxime should be determined for all Streptococcus
pneumoniae isolates. For strains with a penicillin MIC =0.125 mg/L, use vancomycin plus either
ceftriaxone or cefotaxime (see Empirical therapy for doses).
- Specialist advice must be sought particularly if the MIC of these cephalosporins is elevated. Rifampicin
or moxifloxacin are possible alternatives to vancomycin.
- For penicillin-susceptible strains (MIC <0.125 mg/L), use:
(i) benzylpenicillin 1.8 g (child: 45 mg/kg up to 1.8 g) IV, 4-hourly for 10 to 14 days.
[Very ill patients may require treatment for up to 3 weeks.]
H. influenzae meningitis:
- For meningitis due to Haemophilus influenzae type b, use:
(i) ceftriaxone 4 g (child: 100 mg/kg up to 4 g) IV, daily for 7 days
or ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV, 12-hourly for 7 days
OR
(ii) cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly for 7 days.
- If the organism is proven to be susceptible, use:
(i) benzylpenicillin 2.4 g (child: 60 mg/kg up to 2.4 g) IV, 4-hourly for 7 days
OR
(ii) amoxy/ampicillin 2 g (child: 50 mg/kg up to 2 g) IV, 4-hourly for 7 days.
- For patients with immediate penicillin or cephalosporin hypersensitivity, use:
(i) chloramphenicol 1 g (child: 20 to 25 mg/kg up to 1g) IV, 6-hourly for 7 days
OR
(ii) ciprofloxacin 400 mg (child: 10 mg/kg up to 400 mg) IV, 12-hourly for 7 days
Listeria meningitis:
- For meningitis due to Listeria monocytogenes, penicillin and amoxy/ampicillin appear
equally efficacious. Use:
(i) benzylpenicillin 2.4 g (child: 60 mg/kg up to 2.4 g) IV, 4-hourly
OR
(ii) amoxy/ampicillin 2 g (child: 50 mg/kg up to 2 g) IV, 4-hourly.
- In patients hypersensitive to penicillin, trimethoprim+sulfamethoxazole may be used alone:
(i) trimethoprim+sulfamethoxazole 160+800 mg (child: 4+20 mg/kg up to 160+800 mg) IV, 6-hourly.
- There is limited evidence that combination therapy with beta lactam plus
trimethoprim+sulfamethoxazole improves outcomes. The value of adding an
aminoglycoside is not clear.
- The usual duration of therapy is 3 weeks, with extension to 6 weeks in immunocompromised patients.
Oral therapy with trimethoprim+sulfamethoxazole may be used to complete the course after initial 3
weeks if there has been a good response to IV therapy.
Group B strep meningitis
- Streptococcus agalactiae is the commonest cause of meningitis in the newborn. Use:
(i) benzylpenicillin 60 mg/kg up to 2.4 g IV, 4-hourly for 14 to 21 days.
Cryptococcal meningitis:
- Cryptococcal meningitis is caused either by Cryptococcus neoformans (particularly in
immunocompromised patients) or Cryptococcus gattii (previously known as C.
neoformans var. gattii).
- Monitoring of CSF pressure is a critical part of management to ensure that
communicating hydrocephalus does not develop and cause permanent neurological
sequelae. Consultation with those experienced in the management of this condition is
strongly recommended.
- The standard treatment for cryptococcal meningitis is:
(i) amphotericin B desoxycholate 0.7 mg/kg IV, daily (dosage to be adjusted according to
tolerance) for 6 to 10 weeks
PLUS
(ii) flucytosine 25 mg/kg IV or orally, 6-hourly for 6 to 10 weeks (monitor plasma levels)
- Patients infected with Cryptococcus gattii may be slower to respond and require a
longer treatment course. Alternatively, if the CSF is culture negative after 2 weeks of
therapy, cease the amphotericin B desoxycholate and flucytosine and commence:
(i) fluconazole 800 mg (child: 20 mg/kg up to 800 mg) orally or IV for the first dose, then
400 mg (child: 10 mg/kg up to 400 mg) orally, daily for at least 10 weeks of therapy.
- Itraconazole has been successfully used when fluconazole cannot be used.
- In the immunocompromised, long-term suppressive therapy may be required. If there
has been a successful response after 10 weeks of fluconazole at the above dose, reduce
the dose to:
(i) fluconazole 200 mg (child: 5 mg/kg up to 200 mg) orally, daily indefinitely as secondary prophylaxis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-45-320.jpg)
![bacterial
meningitis
[created
by Paul
Young
27/11/07]
general
clinical
course
investigation
- bacterial meningitis is a pyogenic infection of the cerebral ventricles and the subarachnoid space with bacteria usually confined to the nutrient rich cerebrospinal fluid
- most patients with bacterial meningitis exhibit only modest impairment of cognition on presentation. Several days
of malaise, fever & headache are typical and meningismus is usually present
- the CSF indices are almost always abnormal and gram stain or culture usually reveals the infecting pathogen unless
antibiotics were administered beforehand
routes
of infection
- infectious agents can invade the cerebrospinal fluid via three routes:
(i) vascular (via the blood brain barrier)
- most likely pathogens are pneumococci, meningococci, Listeria, E. coli (neonates), group B strep (neonates) & H. influenzae
(ii) transdural
- most likley pathogens are pneumococci, gram negative enteric bacilli, staphlococci (including coagulase negative staph), & H. influenzae
- surgery including VP shunt, trauma especially with cribriform plate fracture & parameningeal infective focus such as sinusitis, mastoiditis,
otitis or osteomyelitis may all predispose to infection by this route; congenital defects such as meningocele may also predispose
(iii) transparenchymal
- most likely pathogens are anaerobic bacilli, enteric gram negative bacilli
- occurs when brain abscess ruptures directly into the ventricles or subarachnoid space
(ii) lumbar puncture: need to exclude coagulopathy
A. opening pressure:
- 40% of patients have an opening pressure of greater than 40cmH20
B. CSF findings:
- WCC of 100-1000, elevated protein & decreased glucose are usually present; normal
or marginally elevated WCC is seen in 5-10% an is associated with poor outcome
- there is usually a predominance of neutrophils (80-85%) but a predominance of lymphocyte
C. Gram stain:
- sensitivity is 60-90% and specificity is at least 97%
D. culture:
- allows further refinement of therapy
(iii) bloods
- FBE, urea, Cr, electrolytes, LFTs, lactate
- blood cultures
- coags
- for unclear reasons, pyogenic meningitis follows a more fulminant course in some patients. These patients experience rapid
deterioration in signs and symptoms within 48 hours. In addition to having fever, headache and meningismus they exhibit early
impariemnt of sensorium ranging from lethargy to coma
- brain parenchyma is usually not affected in uncomplicated bacterial meningitis (even when the illness follows a fulminant course)
- exceptions occur in neonates, in whom Citrobacter freundii & H. influenzae may cause focal areas
of cerebritis & in adults in whom Listeria monocytogenes may cause encephalitis or brain abscess
pathphysiology
- the anatomy & composition of the CSF combined with the paucity of host immunologic defenses
creates a microenvironment that allows persistence and proliferation of microorganisms; once the
CSF is innoculated with pathogens the resolution of infection without antibiotics is virtually impossible
- limited local defense mechanisms may explain the importance of using bacteriocidal rather than
bacteriostatic antibiotics in bacterial meningitis
Acute meningitis syndrome:
- initial manifestations of the illness may be subtle with low grade fever or headache; however, once meningeal symptoms
(vomiting, severe headache and stiff neck) develop, the clinical course is dramatic with patients appearing toxic and higher
integrative functions often deteriorating rapidly
- acute meningitis is an infectious disease emergency with a delay in antibiotic therapy being associated with and adverse outcomes
- if a significant dealy in obtaining CSF specimens is anticipated, antibiotics should be given immediately after peripheral blood
cultures are obstained. Depending on the pathogen, the yield of CSF fluid declines markedly 15 minutes to 4 hours after antibiotics.
nevertheless, the risk of delaying treatment supercedes the need to make a microbiological diagnosis
- common cuases of this syndrome are pyogenic meningitis (pneumococcal, meningococcal, Listeria & others)
- uncommon causes are viral encephalitis (especially herpes simplex), subarachnoid haemorrhage & brain abscess with rupture
- rare causes are viral meningitis, granulomatous meningitis (cryptococcal, mycobacterial), carcinomatous meningitis & brain tumour
Subacute meningitis syndrome:
- febrile illness with a somewhat more gradual progression of signs and symptoms of CNS involvement represents the subacute CNS
infection symfrome. Headache can be mild to severe, neck stiffness can be minimum or marked. Patients with this syndrome are
typically oriented and clinically stable at the onset of illness with a gradual progression of symptoms over >24-48 hours
- although bacteria can cause this syndrome it is more often caused by other pathogens or non-infectious processes
- common causes are viral meningitis, viral encephalitis, rickettsial infection
- uncommon causes are brain abscess, neurosyphillus, brain tumour, granulomatous meningitis
- rare causes are cerebrovascular accident and carcinomatous meningitis
- the first priority when managing subacute CNS syndrome is rapid diagnosis rather than the rapid therapy approach required for
acute meningitis.
- additional diagnostic studies may be indicated for subacute infections. Serological testing for HIV should be performed because the spectrum
of infectious agents is musch broafder among HIV infected individuals. Testing for enteroviruses (PCR), crytococcal antigen, neurosyphilis,
mycobacterial infection (culture or PCR), tick borne infections (Ehrlichia, Rickettsia, Lyme disease) and arboviral encephalitides should be
individualised based on the patient characteristics, severity of illness and knowledge of local pathogens
corticosteroids
general
- much of the morbidity of bacterial meningitis is caused by the vigorous host inflammatory response which may be blocked by corticosteroids
- animal studies have shown improvement in outcome when corticosteroids are given as adjuvant therapy with antibiotics
paediatrics:
- children receiving concomitant dexamethasone and antibiotics have decreased morbidity particularly hearing loss;
however, in these studies the majority of cases were due to H. influenzae which is a rare cause of meningitis in
developed countriessince the introduction of vaccination and questions remain regarding the utility of steroids for other pathogens
adults:
- a randomised controlled trial found a significant reduction in both morbidity and mortality among adults receiving combination
therapy with antibiotics and dexamethasoneparticularly among the subgroup with pneumococcal meningitis (in this study most
infections were due to penicillin sensitive pneumococci and patients were treated with aminopenicillins)
- evaluation of steroid use for resistant pneumococci has not been performed; however, data that demonstrate reduced vancomycin
levels in the CSF when this antibiotic is administered with steroids have raised concern about adjuvant therapy when cephalosporin
resistant pneumococci are prevalent
- the dose of dexamethasone is 10mg iv Q6hrly for 4 days in adults
- in the studies in both children and adults, both steroids and antibiotics were given simultaneously
and it is unknown whether beneficial effects remain when steroids are delayed
complications
- systemic complications may dominate the clinical course of acute bacterial meningitis; 40% of patients
with pneumococcal meningitis have concomitant sepsis which is usually from an extra-CNS site such
as pneumonia. Sepsis may also represent seeding of the blood stream by infected meninges
- many patients with septicaemia in the context of acute bacterial meningitis will meet criteria for activated protein C;
however, it is importatnt to realise that limited data on the safety and efficacy of APC in patients with acute meningitis
exists and there may be and increased risk of intracranial haemmorrhage in these patients
- general complications include adrenal insufficiency due to infarction (Waterhouse
Friderichsen syndrome) and renal failure due to ATN in the setting of hypotension
- neurological complications include deafness, hydrocephalus and cognitive impairment
- complications specific to meningococcal meningitis include purpura fulminans
and necrotising vasculitis leading to skin necrosis and digital gangrene
treatment
empirical
therapy
(i) imaging (NEJM (2005) 354:44-53 recommendations):
cranial imaging should precede lumbar puncture in patients who have:
- new onset seizures
- immunocompromise
- moderate to severe impairment of conscious state (GCS<10) if imaging is not readily available, LP should be
given preference to neuroimaging in all patients except those warning signs of a space occupying lesion
(eg new seizure, papilloedema, focal neurology)
1. If the organism or susceptibility is not known, empirical therapy should cover the most common pathogens.
In patients over 3 months of age, use:
(i) ceftriaxone 4 g (child: 100 mg/kg up to 4 g) IV, daily
or ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV, 12-hourly
OR
(ii) cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly.
2. Listeria monocytogenes is resistant to cephalosporins. If the patient is immunosuppressed or Listeria infection
is suspected, add to the above regimen either:
(i) benzylpenicillin 2.4 g (child: 60 mg/kg up to 2.4 g) IV, 4-hourly
OR
(ii) amoxy/ampicillin 2 g (child: 50 mg/kg up to 2 g) IV, 4-hourly.
3. Add vancomycin if Gram-positive diplococci are seen or a pneumococcal antigen assay in CSF is positive, or if the patient has been
heavily pretreated with a beta lactam (eg for recurrent ear infections). This is to ensure that Streptococcus pneumoniae isolates that
display intermediate or higher resistance to penicillin and/or cephalosporins are adequately covered prior to the availability of culture and
susceptibility results. Consider vancomycin also if Gram-positive cocci resembling staphylococci are seen, or if neutrophils are present but
organisms are not seen, and if viral meningitis or meningococcal disease are unlikely. Use:
(i) vancomycin 12.5 mg/kg up to 500 mg (child <12 years: 15 mg/kg up to 500 mg) IV,
6-hourly (monitor blood levels and adjust dose accordingly; slow infusion required).
- Cease vancomycin if an organism likely to be susceptible to ceftriaxone/cefotaxime is
isolated or if a penicillin-susceptible pneumococcus (MIC <0.125 mg/L) is isolated.
- For neonates and infants under 3 months, the likely organisms are Streptococcus agalactiae, enteric Gram-negative
rods or, rarely, Listeria monocytogenes. Treat as for severe sepsis in children under 6 months of age in whom meningitis
has not been excluded. Intravenous treatment should continue for a minimum of 2 weeks. Repeat lumbar puncture(s) are
usually done to directly assess bacteriological response.
For patients with immediate penicillin or cephalosporin hypersensitivity, use:
(i) vancomycin 12.5 mg/kg up to 500 mg (child <12 years: 15 mg/kg up to 500 mg) IV, 6-hourly
PLUS
(ii) ciprofloxacin 400 mg (child: 10 mg/kg up to 400 mg) IV, 12-hourly
OR
(iii) moxifloxacin 400 mg (child: 10 mg/kg up to 400 mg) IV, daily.
public
health
considerations
- respiratory isolation is required for 24 hours for patients with known or suspected N. meningitis meningitis;
prophylaxis is indicated for close contacts which is defined as those living in the same dwelling or having
close social contact or health care workers who perform intubation or ET tube management](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-46-320.jpg)
![bacterial
meningitis
[created by
Paul Young
02/10/07]
criteria for CT
prior to lumbar
puncture
therapy based
on presumptive
gram stain
identification
empirical
therapy
specific
antimicrobial
therapy
duration
of therapy
the role of
dexamethasone
neonates:
- there are insufficient data to make a recommendation on the use of
adjunctive dexamethasone in neonates with bacterial meningitis
children:
- adjunctive dexamethasone (0.15 mg/kg every 6 h for 2–4 days)
has confirmed benefit for H. influenzae type b meningitis and, if
commenced with or before antimicrobial therapy, suggested benefit
for pneumococcal meningitis in children. Evidence of clinical benefit
was greatest for hearing outcomes.
adults:
- level one evidence supports the use of dexamethasone
(0.15 mg/kg q6h for 2–4 days with the first dose administered
10–20 min before, or at least concomitant with, the first dose
of antimicrobial therapy) in adults with suspected or proven
pneumococcal meningitis
- Dexamethasone should only be continued if the CSF Gram
stain reveals gram-positive diplococci, or if blood or CSF cultures
are positive for S. pneumoniae.
- Adjunctive dexamethasone should not be given to adult patients
who have already received antimicrobial therapy, because administration
of dexamethasone in this circumstance is unlikely to improve patient
outcome
- The data are inadequate to recommend adjunctive dexamethasone to
adults with meningitis caused by other bacterial pathogens
- Concerns have been raised about whether use of adjunctive dexamethasone
may be harmful in patients with pneumococcal meningitis caused by highly
penicillin- or cephalosporin-resistant strains; these patients may require
antimicrobial therapy with vancomycin, and the diminished inflammatory
response induced by dexamethasone might reduce CSF vancomycin penetration
and delay CSF sterilization. This finding has been observed in experimental animal
models of resistant pneumococcal meningitis](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-47-320.jpg)






![bone
& joint
infections
osteomyelitis
empirical
therapy
- For empirical therapy of osteomyelitis, use:
flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly.
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity), use:
cephalothin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
OR cephazolin 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly.
- If Gram-negative infection is suspected, or for children under 5 years not immunised
against Haemophilus influenzae type b (Hib), use:
cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly
OR the combination of
ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV, daily
PLUS flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly.
- For patients with immediate penicillin hypersensitivity, use initially:
vancomycin 25 mg/kg up to 1 g (child <12 years: 30 mg/kg up to 1 g) IV, 12-hourly
- Adjust therapy according to culture and susceptibility results.
general
points
about
osteomyelitis
General:
- Infection in bone may arise from haematogenous spread, direct inoculation following
trauma or surgery, or spread from a contiguous structure such as a joint.
- In children and young adults, haematogenous osteomyelitis usually affects
the long bones; in adults it is more likely to involve the axial skeleton.
- Staphylococcus aureus accounts for more than 80% of disease, although enteric
Gram-negative organisms are an important cause of vertebral osteomyelitis in adults.
- Chronic infections are more difficult to treat and often require prolonged therapy.
- Sequestra, dead bone or foreign material require surgical removal in chronic
infection, or in acute infection which fails to resolve.
Investigation:
- It is important to obtain suitable specimens for culture.
- In chronic infections, sinus cultures may be misleading.
- If cultures are negative and alternative pathology such as malignancy and
tuberculosis are ruled out, treat as S. aureus infection.
osteomyelitis
directed
therapy
Methicillin-susceptible Staphylococcus aureus (MSSA)
- To treat osteomyelitis due to MSSA, use:
flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
then flucloxacillin 1 g (child: 25 mg/kg up to 1 g) orally, 6-hourly
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity), use:
cephalothin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
then cephalexin 1 g (child: 25 mg/kg up to 1 g) orally, 6-hourly
OR
cephazolin 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly
then cephalexin 1 g (child: 25 mg/kg up to 1 g) orally, 6-hourly
- For patients with immediate penicillin hypersensitivity and MSSA with proven
macrolide (and hence lincosamide) susceptibility, use:
clindamycin 450 mg (child: 10 mg/kg up to 450 mg) IV, 8-hourly
then clindamycin 450 mg (child: 10 mg/kg up to 450 mg) orally, 8-hourly
OR
lincomycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly
then clindamycin 450 mg (child: 10 mg/kg up to 450 mg) orally, 8-hourly
- For patients with immediate penicillin hypersensitivity and MSSA which
is not susceptible to macrolides (and hence lincosamides), use initially:
vancomycin 25 mg/kg up to 1 g (child <12 years: 30 mg/kg up to 1 g) IV, 12-hourly
- Base oral therapy following vancomycin on proven susceptibility; suitable
oral options may be trimethoprim+sulfamethoxazole (dose as for MRSA) or
doxycycline 100 mg (child >8 years: 2.5 mg/kg up to 100 mg) orally, 12-hourly.
Methicillin-resistant Staphylococcus aureus (MRSA)
- To treat osteomyelitis due to MRSA, use initially:
vancomycin 25 mg/kg up to 1 g (child <12 years: 30 mg/kg up to 1 g) IV,
FOLLOWED BY (if the organism is proven susceptible)
rifampicin 300 mg (child: 7.5 mg/kg up to 300 mg) orally, 12-hourly
PLUS
fusidate sodium tablets 500 mg (child: 12 mg/kg up to 500 mg) orally, 12-hourly
- If the MRSA is non-multiresistant, for alternative oral continuation therapy,
according to susceptibilities, use:
clindamycin 450 mg (child: 10 mg/kg up to 450 mg) orally, 8-hourly
OR trimethoprim+sulfamethoxazole 320+1600 mg (child: 8+40 mg/kg up to 320+1600 mg) orally, 12-hourly.
- For multiresistant MRSA, alternative oral therapies include linezolid and pristinamycin
management
of infected
prostheses
- Infections involving orthopaedic and prosthetic material are most frequently due
to staphylococci [coagulase-negative staphylococci (eg Staphylococcus epidermidis)
and Staphylococcus aureus.]
- These infections are difficult to cure with antibiotics alone and may require extensive
debridement and/or removal of the infected prosthesis.
- Note that negative bacterial cultures of joint aspirates or intraoperative joint swabs
will not exclude the presence of infection, particularly if the patient is on antibiotics.
- Examination of multiple (at least 5) intraoperative joint tissue biopsies in the absence
of antibiotic treatment is recommended when detection of infection with optimal
sensitivity is required.
- Early infection (presenting within 4 weeks after surgery) is usually due to S. aureus
and can often be successfully treated with extensive debridement, prosthesis retention
and 4 to 6 weeks of appropriate intravenous antibiotics. Cure rates of 60% to 80% have
been reported in this group when the organism isolated is fully susceptible to the
antibiotics used.
- Prosthetic joint infection due to genuine new acute haematogenous seeding can also
be treated this way provided surgery is performed within 72 hours of symptom onset
- For chronic infections, cure is rare if the prosthetic material is not removed. In these
patients, removal of the prosthesis with a 2-stage joint replacement (delayed-exchange
arthroplasty) and 6 weeks of intravenous antibiotics has the best reported success rates
(80% to 90%). One-stage replacement (direct-exchange arthroplasty) may be preferred in
some frail patients, but the success rate is lower (70% to 80%).
general
points
about
septic
arthritis
- Septic arthritis generally presents either spontaneously or following penetrating
trauma as a monoarticular arthritis.
- The pathogens involved are generally similar to those that cause acute osteomyelitis.
- Diagnostic specimens including a joint aspirate and blood cultures should be taken
prior to the commencement of therapy whenever possible. This allows alternative
diagnoses such as acute crystal arthropathies to be firmly ruled in or out.
- It is urgent to drain pus from the infected joint to avoid permanent joint damage and
to allow antibiotics to work effectively. The standard method of drainage is arthroscopic
washout, or arthrotomy for deeper joints. Repeated simple needle aspiration has been
suggested as a less invasive alternative; however, there is insufficient evidence to
recommend this.
empirical
treatment
of septic
arthritis
- Empirical therapy is similar to that of osteomyelitis but should be directed
wherever possible by the result of Gram stain of a joint aspirate.
- Adjust therapy according to the culture and susceptibility results.
- For directed therapy of septic arthritis due to organisms other than
Staphylococcus aureus, seek advice from an infectious diseases physician or
clinical microbiologist.
- Gonococcal arthritis should be treated with cefotaxime or ceftriaxone (as for
disseminated gonococcal sepsis) until susceptibility tests are known. Treatment
should continue for a total of 7 days. Joint washouts are usually unnecessary.
duration
of therapy
for septic
arthritis
septic
bursitis
- Septic bursitis is usually caused by Staphylococcus aureus and often follows
local trauma. The usual sites are the prepatellar and olecranon bursae.
- Confirm with aspiration and culture.
- Sometimes the underlying joint is also involved.
- Treat with an antistaphylococcal antibiotic for 2 to 3 weeks, as for treatment
of Septic arthritis due to S. aureus.
- The infected bursa should be aspirated repeatedly if clinically indicated and
may need formal drainage.
viral
arthritis
- A number of viruses can cause joint inflammation.
- Oligoarthritis or polyarticular disease is more common than monoarticular arthritis.
- Acute rheumatic fever must be excluded.
- Viruses implicated include hepatitis B and C, rubella (and its vaccine), parvovirus
B19 and a number of alphaviruses.
- In Australia, Ross River virus and Barmah Forest virus are the most common.
Although asymptomatic infection and seroconversion with these viruses is common,
acute polyarticular synovitis is not infrequent and may cause severe pain and disability.
- Almost all infections are self-limiting, with joint pain usually resolving within 3 to 6 months.
As there are no effective antiviral drugs, symptomatic treatment with anti-inflammatory
drugs and analgesics is the mainstay of therapy.
duration
of therapy for
osteomyelitis](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-54-320.jpg)
![bone marrow
transplant:
cardiac
complications
[created by
Paul Young
02/10/07]
pulmonary
oedema
General
- commonest cardiac complication requiring ICU admission is pulmonary oedema
Risk Factors
- risk factors are:
(i) pre-existing cardiac disease (even subclinical); EF <50%
(ii) fluid overload associated with the infusion of chemotherapy,
(iii)acute renal failure,
(iv) venoocclusive disease,
(v) severe sepsis
(vi) anemia.
(vii) High-dose chemotherapy used in the preparation for HSCT, such as cyclophosphamide,
cytosine arabinoside, paclitaxel, etoposide, and cisplatin, may be associated with significant
cardiac toxicity and congestive heart failure
pericardial
tamponade
- pericardial effusion following HSCT is rare and is usually related to
(i) cyclophosphamide toxicity,
(ii) viral syndrome,
(iii) chronic GVHD, or
(iv) renal failure
(v) rarely may it be due to bacterial infection (mainly S. aureus) or aspergillosis
endocarditis
Organisms
- The usual organisms isolated are Gram-positive bacteria including
S. aureus and S. viridans; however,there is a high prevalence of
fungal endocarditis, including Aspergillus and Candida species
- In one third of patients, no organisms are isolated, consistent with
the diagnosis of nonbacterial thrombotic endocarditis
Epidemiology:
- Endocarditis is infrequently reported following HSCT (prevalence is approximately 1.3%)
Clinical features:
- The clinical presentation of endocarditis following HSCT can be subtle
(75% of cases are diagnosed at autopsy)
- Left-sided cardiac valves, especially mitral valve, are most commonly involved
Risk factors
- The main risk factors are:
(i) indwelling central venous catheters,
(ii) disruption of skin and mucosal barriers by high-dose chemotherapy and GVHD, and
(iii) the administration of immunosuppressive therapy
arrhythmias
- most commonly associated with electrolyte abnormalities,
hypoxemia, sepsis, MOSF, and use of vasopressor agents](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-55-320.jpg)
![bone marrow
transplant:
gastrointestinal
complications
[created by
Paul Young
02/10/07]
general
- In addition to the common causes of acute abdominal pain in critically ill patients
such as peptic ulcer disease, pancreatitis, and acute cholecystitis, other conditions
that are unique to HSCT recipients should be considered, including:
(i) chemotherapy related abdominal pain,
(ii) GVHD of the intestines,
(iii) intestinal pseudoobstruction,
(iii) intestinal perforation,
(iv) intestinal infections,
(v) hemorrhagic enteritis.
GVHD
of the
intestine
Clinical features:
- GHVD of the intestine is associated with abdominal
pain, nausea, vomiting, diarrhea, and bleeding.
- The abdominal pain may be associated with peritoneal signs
- Commonly, there are other manifestations of
acute GVHD such as hepatitis and skin rash.
Investigations:
- A computerized tomographic scan of the
abdomen will show bowel wall edema.
- Endoscopic biopsy is diagnostic; however, it is rarely
necessary unless there are no other features of the disease.
Treatment:
- GVHD of the intestine usually responds well
to intensification of the immunosuppressive therapy
Intestinal
pseudo-
obstruction
General:
- Intestinal pseudoobstruction is a common cause
of abdominal pain following HSCT and is frequently
seen during the course of these patients in the ICU.
Causes:
(i) GVHD,
(ii) sepsis,
(iii) narcotics,
(iv) electrolyte disturbances, and
(v) chemotherapeutic agents.
Treatment:
- Treatment is supportive and is directed
toward treating the underlying cause.
enteritis
Epidemiology:
- Enteritis is another significant GI problem following HSCT, with
reported prevalence of 43% after allogeneic HSCT
Clinical Manifestations:
- It is usually mild and self-limiting; however, in a small percentage
of patients, it may be severe, leading to dehydration, with hypotension
and acute renal failure.
Causes:
- The main causes of enteritis following HSCT are GVHD,
bacterial infection, the most common of which is Clostridia
difficile enteritis, and viral infections such as rotavirus, adenovirus,
CMV, herpes simplex virus, and herpes zoster virus.
Treatment:
- The management of severe enteritis following HSCT includes
supportive measures and treatment of the underlying pathogenesis.
In the case of severe diarrhea,patients may respond to octreotide,
a somatostatin analog, which inhibits the secretory hormones.
- Anti-diarrhea agents should be avoided because
they may precipitate pseudoobstruction.
- Enteritis due to rotavirus responds to oral immunoglobulins.
Prognosis:
- Prognosis of enteritis following HSCT is generally favorable
GI bleeding
Treatment:
- Management of severe GI bleeding following HSCT is similar to that in other
patient populations. However, endoscopic procedures are of limited value in cases of
diffuse mucosal bleeding.
- Surgery should be restricted to those with focal bleeding sites that do not respond to
transfusion of blood products and endoscopic procedures.
- The outcome of patients who undergo surgical intervention for GI bleeding is poor.
Epidemiology:
- GI bleeding following HSCT has been reported in 7-18% of those patients.
Causes:
- GI bleeding in this patient population is that it tends to be
diffuse mucosal bleeding that may involve the small intestine.
- The most common cause of GI bleeding in allogeneic
HSCT recipients is GVHD (up to 60%)
- Other common causes of severe GI bleeding include mucosal injury
due to chemoradiotherapy, viral infections such as adenovirus, and CMV
that lead to deep mucosal ulcers and necrosis, which may be associated
with severe bleeding.
- Peptic ulcer disease is a rare cause of upper GI bleeding early post
HSCT (6-10% of all cases).
Prognosis:
- GI bleeding is an indicator of poor outcome in critically ill
HSCT recipients, although it is rarely the cause of death.
other
liver
disease
Viral hepatitis:
- that due to adenovirus, herpes simplex virus, and herpes zoster virus
may lead to severe hepatitis with a rapid increase in liver enzymes.
- CMV infection commonly leads to hepatitis, although rarely severe.
- Hepatitis B and C may progress, leading to liver failure when
immunosuppressive therapy for GVHD is tapered.
acute GVHD:
- rarely a cause of fulminant liver failure.
Fungal infection:
fungal infection involving the liver is rare and is usually part
of a multiple system infection. The most common fungal species
that involve the liver are Candida and Aspergillus
veno-occlusive
liver disease
Epidemiology:
- Veno-occlusive disease (VOD) is reported in 20-50% of patients following HSCT.
Pathogenesis:
- VOD arises from thrombosis of small central hepatic venules
due to endothelial cell damage by high-dose chemotherapy.
Clinical manifestations:
- VOD usually develops in the first 21 days following HSCT, and the earliest signs
of the syndrome are weight gain and tender hepatomegaly, followed by jaundice. A
decrease in bilirubin level is an early indicator of recovery.
- The clinical course of VOD varies from mild, self-limiting liver dysfunction
to a rapidly fatal disease associated with MOSF, including acute renal
failure and acute respiratory failure requiring mechanical ventilation.
Risk factors:
- The main risk factors for VOD are:
(i) patient age,
(ii) elevation of transaminases before HSCT,
(iii) the intensity of conditioning regimen, and
(iv) prolonged fever.
Investigations:
- The diagnosis of VOD is based on the clinical picture (the onset of hyperbilirubinemia,
hepatomegaly, and weight gain or ascites in the first 30 days following HSCT).
- Doppler ultrasound of the hepatic blood vessels shows reversal or diminished
portal blood flow.
- Percutaneous liver biopsy carries a high risk of bleeding. Hepatic vein catheterization
with measurement of the hepatic venous pressure gradient (10 mm Hg) and transvenous
liver biopsy confirms the diagnosis of VOD but is rarely performed in clinical practice.
Treatment:
- The management of VOD is supportive and is directed toward sodium and fluid
restriction, diuresis, paracentesis in cases of tense ascites, and avoiding infection
and hepatotoxic medications.
- Thrombolytic treatment is associated with a 30%
response rate, but case fatality approaches 10%.
- Heparin and antithrombin III have been used with variable results.
- Oral ursodeoxycholic acid (ursodiol) is useful in lowering
bilirubin levels and may prevent further hepatic injury caused
by free radicals generated by bile acids.
Prognosis:
- VOD is fatal in 25-50% of patients.
pancreatitis
Epidemiology:
- Acute pancreatitis is reported to occur in 20% of HSCT
recipients at autopsy; however, clinically significant disease
is rare, and the prevalence is 3.5%.
Causes:
The main causes of acute pancreatitis following HSCT are:
(i) medication use (cotrimoxazole, corticosteroids, cyclosporine A),
(ii) infections (CMV and adenovirus),
(iii) GVHD, and
(iv) biliary sludge
Treatment:
The management of severe pancreatitis is
supportive and treating the underlying problem.
Intestinal
perforation
The main causes of intestinal perforation following HSCT are:
(i) CMV ulcers,
(ii) corticosteroids therapy, and
(iii) GVHD
- The management of this condition is similar
to that of nontransplant patients.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-56-320.jpg)
![bone marrow
transplant:
infectious
complications
[created by
Paul Young
02/10/07]
general
- estimated to be the reason for ICU admission in approximately 25%
- susceptible to a wide range of infections including opportunistic infections
such as invasive pulmonary aspergillosis (IPA), CMV, and PCP
viral
CMV:
- The most serious complication of these viral infections is pneumonitis with acute
respiratory failure; however, they may lead to other organ dysfunctions such as
hepatitis, encephalitis, and bone marrow suppression.
fungal
General
- Fungal infections are increasingly identified in critically ill HSCT recipients.
Candida species is the most commonly isolated fungal infection in this patient population.
Invasive
pulmonary
aspergillus
Epidemiology:
- Aspergillus is a leading cause of severe fungal infection following HSCT. The
prevalence of IPA has been rising and currently ranges between 2% and 26%.
Candida
Risk factors:
- The main risk factors for serious candidal infections in HSCT recipients are :
(i) advanced age,
(ii) unmatched donor,
(iii) neutropenia,
(iv) acute GVHD,
(v) underlying disease,
(vi) corticosteroid therapy,
(vii) duration of candidemia
Treatment
- The treatment of candidemia and deep infection is primarily fluconazole; however, if there is
evidence of endophthalmitis or resistant organisms, then caspofungin is the treatment of choice
PCP
Epidemiology:
- P. carinii Pneumonia. P. carinii pneumonia (PCP) is rarely seen following
HSCT due to the effective prophylaxis using trimethoprim-sulfamethoxazole
Clinical Features:
- The clinical presentation of PCP in HSCT recipients is more severe and fulminant
than in HIV patients; however, response to therapy is good if instituted early.
Investigations:
- BAL is the procedure of choice for the diagnosis of PCP, with positive yield in 90% of cases
Time Course
- The onset of IPA has a bimodal distribution, with an early peak during the neutropenic
phase and a late phase during the treatment of chronic GVHD
Investigation:
- Two radiologic signs that are highly suggestive, but not pathognomonic, of IPA on HRCT of
the chest are the Halo sign and aircrescent sign. These signs are demonstrated in 33–60% of
patients with proven IPA
- Sputum cultures and BAL are positive in 45–62% of patients with IPA. Isolation of Aspergillus
species from sputum or BAL fluid has a high predictive value of 82% for IPA in this patient
population, although these tests are negative in 70% of patients with proven IPA
Treatment:
- the treatment of choice for patients with IPA is voriconazole, and in the case of breakthrough
therapy, caspofungin is an alternative
Prognosis:
- The mortality rate of IPA is very high (74–92%)
Clinical features
- The lung is the primary site of Aspergillus infection, leading to severe
pneumonia with vascular invasion, necrosis, and hemorrhage. IPA disseminates
to other organs, especially the brain, kidney, liver, and skin. In the lungs, the
presentation is nonspecific, and fever may be absent. Pleuritic chest pain and
hemoptysis, though nonspecific, should alert to the possibility of IPA
Epidemiology
The prevalence of invasive candidal infection is estimated to be 1.3–10%, with mortality reaching 50%
Clinical features
- Candidemia is the most common serious manifestation of this infection; however, other internal organs
may be affected, including hepatic and splenic infections. Primary candidal pneumonia is extremely rare.
- Viral infections are common following HSCT and may occasionally
result in critical illness. These viruses include CMV, herpes zoster virus,
respiratory syncytial virus, human herpes simplex virus 6, and adenovirus.
Treatment:
- Treatment of CMV pneumonia using ganciclovir and immunoglobulins,
especially when started early in the course of the illness, results in
significant improvement in survival. However, it is important
to note that ganciclovir treatment is associated with significant side
effects, including neutropenia, nephrotoxicity, seizures, and retinal detachment.
Foscarnet is an alternative that may also lead to acute renal failure.
Clinical features:
- CMV pneumonia usually presents a median of 7 wks after transplantation, with
nonproductive cough, dyspnea, fever, and hypoxemia that quickly progresses to
acute respiratory failure
Epidemiology:
- Recently prevalence of CMV has decreased due to:
(i) routine prophylaxis against CMV using ganciclovir
in high-risk patients in the first 100 days following HSCT.
(ii) preemptive treatment of patients with subclinical viremia detected by
surveillance pp65 antigenemia or polymerase chain reaction assay
Risk Factors:
(i) transplant from a seropositive donor to a seronegative recipient
(ii)older age,
(iii) transplantation for hematologic malignancy,
(iv) total body irradiation,
(v) antithymocyte globulins,
(vi) neutropenia,
(vii) GVHD
(viii) CMV seroconversion
General:
- CMV is the most important viral infection following HSCT, and pneumonitis is the
most severe manifestation of this infection.
RSV
Treatment:
- Uncontrolled trials suggest that the combination of aerosolized ribavirin and intravenous immunoglobulins
decrease mortality, especially if started before the onset of acute respiratory failure
Prognosis:
- Once pneumonia develops, mortality is very high and approaches 80%.
Clinical features
- begins with URTI symptoms that progress to lower respiratory symptoms.
Investigation:
- The diagnosis is made by detecting the virus by nasal wash or BAL fluid culture.
HSV-6
General:
- Human herpes simplex virus 6 is another severe viral infection following HSCT and may
cause pneumonitis, marrow suppression,and encephalitis.
Treatment:
- Treatment is by ganciclovir or foscarnet
Herpes Zoster
General:
- Herpes zoster virus infection following HSCT is rare but may lead to a disseminated disease with
pneumonia, hepatitis, skin rash, encephalitis, and disseminated intravascular coagulation.
Treatment:
High-dose acyclovir is the treatment of choice.
bacterial
Risk factors:
- The main risk factors for bacterial infections following HSCT are:
(i) neutropenia,
(ii) mucositis or skin breakdown,
(iii) gastrointestinal problems associated with acute GVHD,
(iv)intravenous catheters
Clinical features:
- Severe bacterial infections in the ICU usually present as pneumonia,
bacteremia, or septic shock.
- Surveillance blood cultures may be necessary to detect occult blood
stream bacterial infections in HSCT recipients, especially those who
are receiving systemic corticosteroids
Organisms:
- Gram-negative pathogens such as Pseudomonas and Klebsiella should be
given important consideration during the neutropenic phase.
- Gram positive organisms such as MRSA, Streptococcus viridans, and enterococci are
being increasingly identified as the main cause of severe bacterial infections following
HSCT](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-57-320.jpg)
![bone marrow
transplant:
neurological
complications
[created by
Paul Young
02/10/07]
epidemiology
The prevalence of clinically significant neurologic problems following
HSCT is estimated to range between 11% and 18%, and these are
generally more common following allogeneic transplantation
Based on an autopsy study, neurologic complications were the cause
of death in 17% of HSCT recipients
risk
factors
(i) high-dose chemotherapy,
(ii) immunosuppressive therapy,
(iii) GVHD, and
(iv) thrombocytopenia
account for 6% of all admissions or transfers to the ICU in this population
Cerebrovascular
accident (CVA)
Epidemiology:
- develops in approximately 3% of HSCT recipients and
is slightly more common following allogeneic HSCT
- CVA develops a median of 28 days following HSCT
Causes:
- The main causes of CVA are, in order:
(i) intracranial bleeding (predominately intracerebral and
subarachnoid hemorrhage secondary to thrombocytopenia),
(ii) cerebral infarction related to infection (predominantly due
to aspergillosis), and
(iii) noninfectious infarction due to thrombosis
(iv) Nonbacterial thrombotic endocarditis is a rare cause of
cerebral infarction seen in HSCT that is related to DIC.
Prognosis:
- The development of CVA is associated with poor outcome, and
in a large study of CVA after HSCT the hospital mortality was 69.4%.
- Age, oncologic diagnosis, type of HSCT, and time of
CVA did not predict poor outcome.
Treatment:
- The management of CVA following HSCT is similar to that
of nontransplantation patients.
- Special considerations in this population are:
(i) correction of thrombocytopenia and coagulopathy,
(ii) careful evaluation for an infectious pathogenesis.
CNS
infections
Epidemiology
- Central nervous system infections account for 10% of neurologic
complications following HSCT. The causes and time patterns of these
infections are similar to that of other organs
Causes:
- The main causes of central nervous system infections
are aspergillosis, which was found in 4.4% HSCT recipients
who underwent post mortem examination
- Central nervous system involvement by aspergillosis is usually
part of disseminated disease, with other evidence of the infection.
- Other causes of central nervous system infection in this
patient population are CMV, herpes zoster virus, toxoplasma,
Candida, Cryptococcus, and bacterial meningitis
Prognosis:
Prognosis of patients with central nervous system involvement
is extremely poor.
metabolic
encephalopathy
Epidemiology
- The prevalence of metabolic encephalopathy in HSCT recipients
ranges between 3% and 13% and is more common following allogeneic
transplantation.
- The condition usually develops in the first 2 months following
transplantation.
Clinical manifestations:
- usually presents with change in mental status or seizures.
- Other patients may present with classic Wernicke encephalopathy,
with altered mental status, ataxia, and ophthalmoplegia.
Causes:
The main causes of metabolic encephalopathy following HSCT are:
(i) hypoxemia,
(ii) electrolyte abnormalities,
(iii) metabolic acidosis,
(iv) sepsis,
(v) hepatic failure, and
(vi) medications including sedatives and analgesics.
(vii) Thiamine deficiency, secondary to malabsorption associated with
acute GVHD, has been suggested as the cause of Wernicke encephalopathy.
Treatment:
- Treatment of metabolic encephalopathy is supportive, including correction
of electrolyte abnormalities and hypoxemia, withholding offending medications,
and treatment of the underlying problems.
treatment-
related
neurological
complications
Risk factors:
- The risk of neurologic complications increases with:
(i) history of cranial radiation,
(ii) hypertension,
(iii) uremia,
(iv) hypomagnesemia,
(v) lactam antibiotics,
(vi) high-dose corticosteroids
Specific causes:
- OKT3 treatment has been associated with aseptic meningitis
that may develop 24-72 hrs after injection. [Pretreatment with
corticosteroids may reduce or prevent this syndrome].
- Antibiotics such as imipenem may be the cause of
seizure activity.
- Corticosteroids are associated with myopathy, psychosis, and
other problems resulting from withdrawal of this medication.
- the treatment of HSCT recipients in the ICU may lead to further
neurologic complications, including critical care polyneuropathy
and myopathy and prolonged effects of neuromuscular blocking
agents and sedatives.
- Cyclosporine A may lead to encephalopathy, leukoencephalopathy,
generalised cerebellar dysfunction, hemiparesis, quadriplegia, and seizures
GVHD
- Acute GVHD is not specifically associated with neurologic complications,
except for encephalopathy associated with other organ dysfunction.
- Chronic GVHD may be associated with polyneuropathy, polymyositis, and myasthenia gravis.
Treatment:
- Most of these syndromes respond to intensifying immunosuppressive therapy](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-58-320.jpg)
![bone marrow
transplant:
pulmonary
complications
[created by
Paul Young
02/10/07]
engraftment
syndrome:
Time Course
- Engraftment syndrome develops within 96 hrs of engraftment
Epidemiology
- The syndrome is reported in 7–35% of HSCT recipients
- Engraftment syndrome is described following autologous
HSCT; however, it is also seen in patients following allogeneic
transplantation (it coincides with neutrophil recovery and may
be due to the release of cytokines by these neutrophils
Clinical features
- characterized by fever, erythematous rash, diarrhea, renal
impairment, and diffuse pulmonary infiltrates (noncardiogenic
pulmonary edema due to capillary leak)
Treatment:
- cease GCSF; steroids decrease duration of syndromes
Prognosis:
- Mortality secondary to engraftment syndrome is around 25%:
Diffuse
alveolar
haemmorrhage
Prognosis:
- mortality is greater than 70%; usually from multiorgan failure
General:
The following criteria are suggested to define this syndrome:
(i) evidence of widespread alveolar injury manifested by multilobar pulmonary infiltrate,
(ii) symptoms and signs of pneumonia, and abnormal pulmonary physiology with
increased alveolar to arterial oxygen gradient and restrictive ventilatory defect
(iii) absence of infection that may be associated with similar presentation
(iv) BAL showing progressively bloodier return from three separate subsegmental
bronchi or the presence of at least 20% hemosiderin-laden macrophages or the
presence of blood in at least 30% of the alveolar surfaces of lung tissue
Pathogenesis:
- pathogenesis involves:
(i) damage to endothelium by chemotherapy
(ii) +/- alveolitis secondary to acute graft versus host disease
Risk factors:
(i) intensive chemotherapy before HSCT,
(ii) total body irradiation,
(iii) older age,
(iv) white blood cell count recovery,
(v) renal insufficiency
NB: coagulopathy is not a recognised feature
Treatment:
- treatment is largely supportive; steroids are commonly used.
- In retrospective studies, high-dose methylprednisolone(125–250 mg
every 6 hrs for 4–5 days and then tapered over 2–4 wks) was associated
with a better outcome compared with low-dose or no corticosteroids groups.
Clinical features:
- The syndrome is characterised by progressive dyspnea, cough,
fever, and hypoxemia. Hemoptysis is rare.
- The chest radiograph shows bilateral interstitial and alveolar infiltrates that tend
to be perihilar and in lower lobes. These radiologic findings may precede by
an average of 3 days the clinical presentation.
- HRCT of the chest shows bilateral ground glass infiltrates
Epidemiology
- occurs in 5% and accounts for 40% of cases of respiratory failure requiring ICU
admission after HSCT (slightly more common after autologous rather than allogeneic)
idiopathic
pneumonia
syndrome:
General:
- diffuse pneumonia syndrome that develops
without identification of an infectious aetiology
Epidemiology:
- occurs in 10% (slightly more common
in allogeneic than autologous transplant)
Risk factors:
- The main risk factors for IPS are:
(i) older age,
(ii) malignancy other than leukemia,
(iii) lower performance status before transplantation,
(iv) positive donor cytomegalovirus serology,
(v) high-dose chemotherapy,
(vi) total body irradiation,
(vi) high-grade acute GVHD,
(vii) multiorgan failure
Prognosis:
- mortality is greater than 70%
Treatment:
- treatment is supportive; corticosteroids are
commonly used although evidence is lacking
BO
Prognosis:
- gradually worsens over months to years and patients eventually die of respiratory failure.
General:
- Bronchiolitis obliterans is an inflammatory disease of the small airways that develops
later in the course of allogeneic HSCT. It leads to progressive obstructive airway disease
with no parenchymal involvement
Treatment:
- The treatment of bronchiolitis obliterans is difficult, and these
patients do not respond well to systemic corticosteroids.
Chronic therapy with macrolides may slow the progression of this disease
BOOP:
Epidemiology:
- seen in 1.4% (primarily in allogeneic recipients)
Clinical features:
- Patients usually present with dyspnea, dry cough, and fever. They are commonly hypoxemic
and may develop acute respiratory failure requiring mechanical ventilation. The condition is
usually misdiagnosed as pneumonia; however, cultures are negative.
- HRCT of the chest shows patchy consolidation with ground glass attenuation
- The diagnosis is confirmed by surgical lung biopsy. Transbronchial biopsy may
provide the diagnosis in a small number of patients.
Treatment:
- Establishing the diagnosis is essential because these patients
have a good response to long-term systemic corticosteroid therapy.
Prognosis:
- The overall case fatality in patients with BOOP following HSCT is 21%](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-59-320.jpg)
![bone marrow
transplant: renal
complications
[created by
Paul Young
02/10/07]
general
-Prevalence of acute renal failure following HSCT varies between 9% and 53%.
- The presence of acute renal failure significantly affects the mortality
of HSCT recipients. Between 5% and 33% of these patients require
renal replacement therapy. Mortality in those requiring hemodialysis is
high, with ranges between 84% and 100%.
tumour
lysis
syndrome
General:
- Tumor lysis syndrome is due to the breakdown of tumor cells following radiochemotherapy.
- The syndrome is rarely seen following HSCT because the underlying malignancy
is usually in remission or partial relapse at the time of transplantation, so the burden
of tumor cells is rarely high.
Clinical features:
- When tumor lysis syndrome develops, it usually occurs in the first few days following
chemotherapy and is characterized by hyperuricemia, hyperkalemia, hyperphosphatemia,
hypocalcemia, and oliguric renal failure.
Treatment:
- This syndrome is usually reversible by adequate intravenous hydration and alkalinization of
the urine.
- Allopurinol, hydration, alkalinization of urine, and oral phosphate binding antacids 1-2 days
before chemotherapy are effective in preventing this syndrome.
Infusion
of stem
cells
- Infusion of stem cells may result in acute renal failure due to hemolysis,
which leads to hemoglobinuria and proximal acute tubular necrosis.
- The infusion of hematopoietic stem cells cryopreserved with dimethyl
sulfoxide probably contributes to intravascular hemolysis.
- Factors that increase the risk of acute renal failure in this situation
are hypovolemia and acidosis.
- Adequate hydration and alkalinization
of the urine with adequate urine output protects against this complication.
haemorrhagic
cystitis
Epidemiology
- Hemorrhagic cystitis develops in 25% of allogeneic HSCT recipients.
Causes:
- The condition is precipitated by cyclophosphamide metabolites,
busulfan, or irradiation.
- Hemorrhagic cystitis may also develop later (median, 40-80 days)
following HSCT secondary to BK virus, adenovirus, or CMV infections.
Prevention:
- Hemorrhagic cystitis is prevented by intravenous hydration,
diuresis, irrigation of the urinary bladder, and the use of mesna.
venoocclusive
renal disease
Epidemiology
- VOD is the most common cause of acute renal
failure in the first 10-21 days following HSCT
Clinical features:
- VOD is associated with a hepatorenal syndrome characterized by
sodium retention, weight gain, and edema and ascites.
- This is followed by azotemia.
Risk factors:
- The main risk factors for acute renal failure in patients with VOD are:
(i) mismatched graft,
(ii) age of > 25 yrs,
(iii) high baseline creatinine,
(iv) sepsis, and
(v) the use of amphotericin B
Drug
nephrotoxicity
General:
- is an important cause of acute renal failure and
should be considered anytime following HSCT.
Causes:
- Cyclosporine A causes intense afferent arteriolar vasoconstriction
and nephrotoxicity, which is associated with hyperkalemia, metabolic
acidosis, hyperuricemia, and hypomagnesemia
- Other drugs that lead to acute renal failure following HSCT include
cytotoxic agents such as nitrosurea, methotrexate, and cyclophosphamide;
antibiotics such as amphotericin B, acyclovir, foscarnet, and aminoglycosides;
and immunosuppressive agents such as tacrolimus.
electrolyte
disturbances
- Electrolytes abnormalities are common following HSCT.
- These include hyponatremia, hypokalemia, and hypomagnesemia, and
are related to intravenous fluids, diarrhea, total parenteral nutrition, renal insufficiency,
and drugs such as diuretics, cyclophosphamide, amphotericin B, and
cyclosporine A.
- Severe hyponatremia (serum Na <125mEq/L) is reported in 19%
of HSCT recipients a median of 19 days following transplantation.
- The most common causes of severe hyponatremia are SIADH, infections,
diarrhea, GVHD, VOD, acute renal failure, and the effect of medications
and intravenous fluids](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-60-320.jpg)
![Bone marrow
transplant
related TTP
[created by
Paul Young
02/10/07]
Epidemiology:
- It is more commonly identified in allogeneic HSCT recipients
(prevalence, 5-15%); however, TTP is also seen after autologous
HSCT.
time
course
- The median time of onset of TTP is 44 days following HSCT.
clinical
features
- Classic pentad of TTP:
Fevers
Anaemia (microangiopathic haemolytic)
Thrombocytopenia
Renal Impairment
Neurological symptoms
- Hemolytic uremic syndrome, which has also been described
following HSCT, is similar to TTP but differs in the severity
of renal impairment.
risk
factors
- The main risk factors for TTP following HSCT are:
(i) older age,
(ii) female sex,
(iii) human leukocyte antigen mismatching,
(iv) high-grade acute GVHD,
(v) cyclosporine treatment, and
(vi) history of severe infection
pathogenesis
- The proposed mechanisms of TTP following HSCT include endothelial
damage due to chemotherapy or cyclosporine that led to release of cytokines,
such as tumor necrosis factor that precipitate a prothrombotic state
- It is important to note that deficiency of von Willebrand factor- cleaving
protein, which is implicated in the pathogenesis of classic TTP, does not play a
role in TTP following HSCT.
differential
diagnosis
- The most important differential diagnosis of TTP following
HSCT is cyclosporine toxicity, which may lead to microangiopathic
hemolytic anemia, renal impairment, and neurologic complications.
treatment
- The management of TTP following HSCT includes discontinuing cyclosporine or
tacrolimus and avoiding platelet transfusion.
- The role of plasma exchange, which is the mainstay of treatment in idiopathic
TTP, is not clear. Furthermore, the response to plasma exchange in cases of TTP
following HSCT is not as good as that with idiopathic TTP (25% vs 90%, respectively.)
prognosis
- The prognosis of TTP following HSCT is generally poor,
and the mortality rate is around 70%
- Mortality is higher if the syndrome develops in the first 120
days following HSCT, after treatment with cyclosporine or tacrolimus, or if
there is neurologic deficit. The only predictor of resolution of TTP is the absence
of renal impairment.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-61-320.jpg)
![Botulism
[created
by Paul
Young
19/11/07]
general
- botulism is the neuroparalytic disorder resulting from intoxication
with the exotoxins produced by Clostrium botulinum & several other
strains of clostridia
- C. botulinum are spore-forming obligate anaerobes whose heat
resistant spores are widely distributed in soil & marine sediment
throughout the world
food-
borne
botulism
general:
- ingestion of contaminated food with absorption of toxin
from the duodenum jejunum causes food borne botulism
- the most commonly implicated foods include home-canned
fruit & vegetables due to failure to use a proper combination of
heat pressure & time to kill spores.
manifestations:
- generally develop within 12-36 hours of ingestion of contaminated
food with the acuity & severity of illness related to the amount of
toxin absorbed
- in general, a symmetrical descending paralysis with multiple cranial
neuropathies evolves rapidly in the absence of fever or altered sensorium
- in food borne botulism, the initial symptoms are often gastrointestinal
& include nausea, vomiting, diarrhoea & abdominal cramping which may
be due to ingestion of other bacterial metabolites along with botulinum
toxin
- parasympathetic dysfunction may present early with dry mouth & blurred
vision associated with dilated poorly reactive pupils
- diplopia often develops secondary to extraocular muscle weakness with
paretic dysconjungate eye movements. With paralysis of bulbar muscles,
patients may exhibit flaccid dysarthria, chewing difficulty & dysphagia
- the upper extremities, trunk & lower extremities may become paretic in
a descending fashion
- autonomic dysfunction may manifest as gastrointestinal dysmotility,
orthostatic hypotension, altered resting pulse, urinary retention or
hypothermia
- respiratory compromise may occur due to a combination of upper
airway compromise from weak oropharyngeal muscles & diaphragmatic
weakness
- clinical manifestations vary with the various types of botulinum toxin
wound
botulism
general:
- wound botulism results from in vivo toxin production in abscessed
* devitalised wounds
- wound botulism has been reported after iv drug use and repeated
heroine inhalation
manifestations:
- in contrast to the rapid onset of botulism in food-borne disease with
ingestion of pre-formed toxin, the incubation period for wound botulism
is 7 days (range 4-14 days)
- the neurological signs and symptoms are virtually identical to food-borne
botulism except for the absence of prodromal gastrointestinal symptoms
prognosis:
- the fatality rate for an index case is 25% while the the rate for cases after
recognition of an outbreak is 4%
infant
intestinal
botulism
general:
- results from the ingestion of c. botulinum spores that germinate,
colonise the large intestine & produce botulinum toxin in vivo
- ingestion of ambient C. botulinum spores, distributed widely in soils and
dust is thought to represent the primary route of exposure; honey is also
a significant risk for infant botulism
- peak susceptability is seen at between 2 and 4 months of age
manifestations:
- a clinical spectrum exists with some infants exhibiting relatively mild
& self limited disease involving several days of constipation, poor feeding,
& lethargy and other infants developing acute tetraparesis & respiratory
failure
- in classic cases, constipation is often the initial symptom followed by lethargy,
poor feeding, and weak cry
- examination reveals hypotonia with head lag, ptosis, reduced facial expression,
and reduced gag, suck & swallow reflexes. Deep tendon reflexes are reduced
or absent. Extraocular movements are often paretic & pupils may be large
& poorly reactive
prognosis:
- although course is variable most hospitalised infants reach maximal
paralysis at approximately 1-2 weeks after hospitalisation and begin
to improve after 1-3 weeks
- the case mortality is less than 1% in hospitalised patients
adult
intestinal
botulism
- children and adults may be susceptible to intestinal colonisation
& in vivo production by C. botulinum, C. baratii or C butyricum when
the gastric barrier is compromised & intestinal flora are altered
- occurs in the setting of intestinal surgery, gastric achlorhydria, broad
spectrum antibiotic treatment, and inflammatory bowel disease
inhalational
botulism
- inhalation botulism does not occur in nature but is the
result of an attempt to use the toxin as a bioweapon
- release of aerosolised toxin has the potential to produce a botulism
outbreak. The features of such an outbreak might include numerous
cases within an outbreak, outbreaks with a common geographic factor
without a common dietary exposure & multiple simultaneous outbreaks
iatrogenic
botulism
- therapeutic use of botulism for dystonia, spasticity and other conditions
occasionally results in inadvertent paralysis of nearly muscles & has been
reported to cause paresis of distant muscles in rare reports](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-62-320.jpg)
![brain
abscess
[created
by Paul
Young
12/11/07]
general
pathophysiology
clinical
course
imaging
therapy
- pyogenic brain abscess is a localised suppurative infection of parenchymal CNS tissue
- differentiating brain abscess from other CNS infections or brain tumours may be
challenging as there is significant overlap between the clinical and radiological presentation
- even with modern antibiotic therapy and radiographic
techniques, mortality remains as high as 20%
- a brain abscess begins as a localised area of parenchymal
(cerebritis), which evolves to necrosis & frank suppuration
- the initial stage, characterised by vascular congestion, petechial
haemorrhage, cerebral oedema and tissue softening is demonstrable
by MRI
- as cerebritis progresses, CT findings become abnormal, revealing
a capsule like hyperaemic zone surrounding the area of inflammation
- as the abscess matures, a dense capsule is formed. In relatively avascular
areas of the brain, capsule formation is delayed. Once it forms, however,
the capsule resolves slowly.
- in the preantibiotic era, contagious foci (middle ear, sinuses, mastoids) caused
most brain abscesses; however, more commonly now cases are due to distant
foci of infection or originate for unknown sites
- with haematogenous spread, abscesses tend to seed along the middle cerebral
artery distribution
aetiology
- In brain abscess or subdural empyema, the infecting organism(s) vary with the underlying predisposing cause.
- variable signs & symptoms of brain abscess relate to variations in location,
size, and rapidity of development. At one extreme, the course may span
weeks with few constitutional symptoms. At the other extreme, a previously
assymptomatic brain abscess may rupture into the subarachnoid space and
cause death within hours
- brain abscess usually progresses subacutely for 7 to 14 days. Classic symptoms
include excruciating headache, low grade fever, and focal neurological signs.
- occasionally, a patient has no symptoms referable to the CNS and fever may
be absent in as many as 50% of cases
- parameningeal foci spread to brain abscess as inflammatory process erodes
through bone and meningeal tissues
- chronic otitis, sinusitis or post-traumatic dural defects with progressive neurological
deficit strongly suggests brain abscess
- bacterial pathogens also invade neural tissues via haematogenous spread
- the presence of chronic extrameningeal suppurative foci or illicit iv drug use predisposes
to brain abscess; in as many as a third of patients there is no obvious source of infection
- filtration by the pulmonary vasculature protects the brain; cardiac shunts
& pulmonary AV fistulae bypass this protection
- CNS complications of brain abscess relate to both tissue inflammation
& increased ICP from a space occupying lesion
- non specific complications common to all critically ill patients include aspiration,
GI bleeding and thromboembolism
- specific complications include focal neurological deficits, altered mental state or seizures
- when surrounding oedema is excessive, aggressive therapy with corticosteroids is warranted
- if a brain abscess ruptures into the subarachnoid space or into a cerebral ventricle,
rapid deterioration in mental state is the rule and mortality is high
- CT and MRI are both useful in monitoring progress of a brain abscess. An expanding
lesion may be aggressively drained or a stable or shrinking abscess can be observed
- CT scanning has some limitations particularly if performed without contrast.
It may miss early cerebritis and the cerebellum and brainstem may be poorly seen.
In particular, it may miss lesions 1.5cm or smaller as are typically seen in endocarditis
General
- Aspiration or biopsy is essential to guide antimicrobial therapy.
- Consultation with a clinical microbiologist or an infectious diseases physician in
addition to surgical assessment is advised
antimicrobials - general principles:
- choice of antimicrobials should be guided by culture results, given the
diversity of pathogens and the need for prolonged therapy (eg 6-8 wks)
- additional pharmacological considerations include CNS penetration and parenteral administration
- empirical therapy should be commenced after aspiration while awaiting culture results and should
be guided by likely pathogens
- additional tests for culture negative brain abscess include HIV serology, serum crytococcal
antigen, and toxoplasmosis titres
- in selected cases brain abscesses can be treated with antimicrobials alone,
particularly when the causative agent is known and the lesion is <2.5cm
- medical management may also be necessary when the lesion is inaccessible
or surgical intervention poses unacceptable risk
- In the immunosuppressed, Nocardia species, Toxoplasma and fungi such as Aspergillus or Scedosporium
are more likely to occur.
- In the nonimmunosuppressed, most brain abscesses are polymicrobial with microaerophilic cocci, including
Streptococcus anginosus/milleri, and anaerobic bacteria predominating. However, where the likely site of
origin is the ear, enteric Gram-negative bacilli are commonly involved, while after trauma or surgery,
staphylococci predominate.
antimicrobials - non immunocompromised patients without prior neurosurgery
- For empirical therapy following aspiration,
use:
benzylpenicillin 2.4 g (child: 60 mg/kg up to 2.4 g) IV, 4-hourly
PLUS
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 8-hourly
PLUS EITHER
ceftriaxone 4 g (child: 100 mg/kg up to 4 g) IV, daily
or ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV, 12-hourly
OR
cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly.
antimicrobials - non immunocompromised patients with prior neurosurgery
For postneurosurgical brain abscess, use:
vancomycin 12.5 mg/kg up to 500 mg (child <12 years: 15 mg/kg up to 500 mg) IV, 6-hourly
[current evidence for this indication is based on 6hrly dosing]
PLUS EITHER
ceftazidime 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly
OR
meropenem 2 g (child: 40 mg/kg up to 2 g) IV, 8-hourly.
- steroids should not be routinely used but are often used if oedema is severe
- Modify therapy on the basis of Gram stain and culture results.
- The duration of treatment depends on clinical response and radiological evidence of resolution.
Treatment of the immunocompromised patient
(i) Nocardiosis
- Brain abscess is a common manifestation of disseminated nocardiosis in
the immunocompromised.
- For Nocardia asteroides and other species susceptible to sulfonamides,
IV or oral trimethoprim+sulfamethoxazole is the usual initial treatment:
trimethoprim+sulfamethoxazole 160+800 mg (child: 4+20 mg/kg up to
160+800 mg) IV or orally, 6-hourly for 3 to 4 weeks
FOLLOWED BY
trimethoprim+sulfamethoxazole 160+800 mg (child: 4+20 mg/kg up to
160+800 mg) orally, 12-hourly for 3 to 6 months.
- Combination therapy with trimethoprim+sulfamethoxazole PLUS amikacin
has shown promise as empirical therapy, and in difficult cases that were
slow to respond to trimethoprim+sulfamethoxazole alone.
Alternative therapy using drugs such as amoxycillin+clavulanate, meropenem,
ceftriaxone, minocycline, amikacin or linezolid have all been reported to be
successful in small numbers of cases, particularly for some of the more unusual species.
Ongoing treatment for 6 to 12 months with oral trimethoprim+sulfamethoxazole may be needed
(ii) Toxoplasmosis:
- In AIDS, cerebral infection with Toxoplasma gondii is common. Use:
sulfadiazine 1 to 1.5 g (child: 50 mg/kg up to 1 to 1.5 g) orally or IV, 6-hourly
PLUS
pyrimethamine 50 to 100 mg (child: 2 mg/kg up to 50 to 100 mg) orally, for the first
dose, then 25 to 50 mg (child: 1 mg/kg up to 50 mg) orally, daily.
- Duration of therapy is for 3 to 6 weeks depending on clinical response. Relapse is
common, so maintenance therapy with half the above dosages is necessary while the
patient is immunosuppressed.
- Calcium folinate 15 mg orally daily is usually added to reduce bone marrow
suppression, and the white cell and platelet counts must be monitored closely.
- For patients allergic to sulfonamides, substitute for sulfadiazine, clindamycin 600 mg
(child: 15 mg/kg up to 600 mg) orally or IV, 6-hourly](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-63-320.jpg)
![brain
death
[created
by Paul
Young
29/11/07]
general
- the ability to certify death when there is irreversible cessation
of brain function enables withdrawal of treatment on humanitarian,
ethical & utilitarian grounds.
- certification of death by brain death provides an opportunity for
organ donation
- brain death in adults is usually the result of subarachnoid haemorrhage
or traumatic brain injury while trauma is the most common cause in children
definition
- In Australia, for the purposes of organ removal for transplantation, the
statutory definition of death is irreversible cessation of all brain function.
- In most jurisdictions the means to determine irreversible brain function
are not determined by law but have been drafted by medical bodies
- the concept of a clinical state of brain death was first proposed in 1968
by Harvard Medical School (Harvard criteria) & subsequently was shown
to be demonstrable without an EEG (Minnesota criteria)
- the UK statements on brain death made in 1976 & 1979 and the USA report
of 1981 provide the basis for current guidelines in Australiasia and many other
parts of the world
brainstem
function
- the brainstem maintains consciousness & the sleep-wake cycle
- pathways through the brainstem are required for cranial nerve reflexes
& voluntary & coordinated trunk & limb movements
- pathways serving eye movements pass through both the pons & midbrain
- spontaneous ventilation is dependent on medullary nuclei
- brain death will always result in cardiac asystole within days or weeks
& despite continuation of full support with deterioration of myocardial
function through poorly understood mechanisms
preconditions
Apnoeic coma not due to:
(i) neurodepressant drugs
- if overdose is suspected then a toxicology screen should be obtained
and assays may be necessary; if a depressant drug is present adequate
time must be present to allow its effects to be excluded with the
observation period dependent on drug pharmacokinetics, dose used,
and the patients hepatic and renal function
(ii) hypothermia
- core temperature should be at least 35 before testing is performed
(iii) neuromuscular relaxants
- effects of muscle relaxants if used must be excluded with a peripheral
nerve stimulator
(iv) metabolic or endocrine disturbance
- possible factors should be carefully assessed & there must be no profound
abnormality of serum urea, electrolytes, acid-base status or blood glucose
diagnostic
tests
(i) absent motor response to pain in cranial distribution
- motor responses in cranial distribution (eg grimacing) are absent
when painful stimuli are applied to any somatic area
[tests trigeminal sensory supply & facial cranial nerves]
NB: tendon and plantar reflexes are spinal reflexes and may be present
(ii) absent pupillary reflexes
- both pupils are fixed and unresponsive to light
- pupil size is irrelevant although pupils are usually dilated
[NB: tests the occulomotor nerve]
(iii) absent corneal reflex
- corneal reflexes are absent to a firm touch on the cornea using a cotton wool swab
[tests the trigeminal & facial nerves]
(iv) absent oculovestibular reflex (cold caloric test)
- no eye movement occurs after slow injection of ice
cold water into one or preferably each ear canal
- clear access to the tympanic membrane should be
confirmed by direct inspection with an auroscope
[tests the vestibulocochlear VIII, occulomotor III & abducen VI nerves]
(v) absent gag reflex & cough reflex
- gag & cough reflexes are absent in response to pharyngeal, laryngeal or
tracheal stimulation (tests the glossopharyngeal IX & vagus X cranial nerves)
(vi) absent respiratory movement on disconnection from the ventilator
- testing for apnoea involves disconnection from the ventilator when the PaCO2
is near normal, ensuring that it reaches the threshold required to stimulate the
medullary centre and observing the patient for respiratory movements
- a PaCO2 of greater than 60mmHg and a pH of <7.30 confirms adequate stimulus
[NB: the threshold in patients with chronic CO2 retention needs to be adjusted
eg 20mmHg above baseline]
- causes of auto-triggering of the ventilator in a brain dead patient include:
(i) cardiogenic oscillations
(ii) high sensitivity settings
(iii) circuit leaks
(iv) water condensation in the circuit
confirmatory
tests
general:
- some jurisdictions (not Australia or NZ) require confirmatory tests
- in Australiasia confirmatory tests are required if clinical criteria cannot be met
indications for confirmatory tests:
(i) no clear cause for coma exists
(ii) possible drug or metabolic effect on coma
(iii) cranial nerves cannot be adequately tested
(iv) cervical vertebra or cord injury is present
(v) cardiorespiratory instability that precludes apnoea testing
specific confirmatory tests include:
(i) four-vessel angiography
- brain death is confirmed by absence of blood flow to the brain
NB: in the unusual situation of absent brainstem reflexes due to primary
brainstem injury but residual blood flow to the supratentorium, brain death
cannot be diagnosed
(ii) Technetium 99 nuclear isotope brain scan
- uses imaging of radioactive substances that usually cross the blood
brain barrier to demonstrate absence of brain perfusion (hollow skull sign)
(iii) EEG
- recordings are obtained over 30 minutes using at least 8 scalp electrodes
to demonstrate absence of electrical activity; while EEG does not adequately
assess brainstem function is used in selected patients such as young children
(iv) MRI
- diffusion weighted MRI can show structural changes secondary to brain death
(v) transcranial doppler ultrasound
- occlusion of blood flow is manifest by oscillating signals, systolic spikes &
disappearance of flow signals
(vi) multimodality evoked potentials
- can demonstrate successful loss of function of various afferent pathways of
the brainstem but use in brain death testing has yet to be validated
other
considerations
(i) timing of testing & retesting
- two full & separate examinations are usually required to demonstrate
irreversibility. The first examination should be after at least 4 hours of
observed coma and absent cough, gag & muscle activity. The second
examination should be after at least 6 hours.
- for primary hypoxic brain damage and encephalitis prolonged observation
is recommended
(ii) assessors
- two doctors of appropriate standing should undertake examinations
- neither doctor should be involved in organ removal or transplantation
(iii) certification of death
- death must be certified by the two doctors who conducted the brain
death testing
- the time of death is the time of completion of the second confirmatory test
(iv) limb movements
- movement of the limbs, neck or body, deep tendon, abdominal &
Babinski reflexes may all be seen as they may be generated by the
spine; they do not preclude brain death
(vi) the oculocephalic reflex
- absence of the oculocephalic reflex is not a requirement & as it is often subjective
children
general:
- caution is recommended in applying standard brain death testing criteria to children
under 5 year of age on the assumption that the young brain has a greater capacity for
recovery after acute damage. In general, the same priniciples are applied as for adults
but a longer period of observation and a confirmatory test is usually conducted.
term to 2 months:
- clinical examination plus radionucleotide brain flow study
2 months to 1 year:
- two examinations and EEGs separated by 24hrs
- the second examination & EEG can be omitted if there
is absent cerebral blood flow on radionucleotide study
over 1 year:
- criteria are similar to adults but an observation period of >12hrs is recommended](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-64-320.jpg)



![calcium
disorders
[created
by Paul
Young
18/12/07]
calcium
homeostasis
general
- Calcium is a highly regulated, ubiquitous cation that has multiple roles in the body.
- changes in intracellular calcium concentration affect a myriad of cell functions,
including cell death or apoptosis; the duration and strength of cardiac muscle
contraction; and smooth muscle contraction in blood vessels, airways, and the uterus
- Calcium exists in the extracellular plasma in a free ionized state as well as bound to
other molecules.
- "Normal" plasma concentrations of total calcium vary between laboratories, but the
range of (bound and unbound) calcium is 2.2 - 2.5 mmol/L). The biologically inert
bound fraction (55% of the total) binds to proteins.
- Changes in albumin alter total calcium concentrations significantly, since the majority
of protein-bound calcium associates with albumin.
- A small percentage of calcium is associated with other proteins, such as beta-globulins,
or nonprotein molecules such as phosphate and citrate.
- Forty-five percent of the total calcium is biologically active and exists in the ionized
form. Ionized calcium concentrations are inversely affected by the pH of blood; an
increase in pH will decrease the ionized calcium concentration by 0.36 mmol/L, such that
patients with metabolic alkalosis often are hypocalcemic.
symptoms of
hypercalcaemia
- Gastrointestinal symptoms result from smooth muscle relaxation and include
constipation, anorexia, nausea, and vomiting.
- Neurologically, patients with hypercalcemia can be lethargic, hypotonic,confused, or
even comatose.
- Effects on the kidneys include polyuria, dehydration, and nephrolithiasis. Dehydration
leads to proximal tubule resorption of sodium and calcium in an effort to expand the
extracellular volume, but this paradoxically worsens hypercalcemia
- Hypercalcemia also affects the electric conduction pathways of the heart. Patients
with elevated calcium concentrations have electrocardiographic changes marked by
shortened QTc intervals. In addition, severe hypercalcemia can cause the Osborn,
or J wave, seen at the tail end of the QRS complex, which usually is associated
with hypothermia.
- Increased calcium concentrations also have been shown to cause pancreatitis
causes of
hypocalcemia
management of
hypercalcemia.
general
- Mild asymptomatic hypercalcemia discovered on preoperative assessment should be
evaluated further, whereas symptomatic hypercalcemia requires more urgent therapy.
- Pharmacologic agents associated with hypercalcemia should be discontinued; specifically,
digoxin potentiates arrhythmias in the setting of hypercalcemia and should be discontinued.
Fluids and diuretics
- In the setting of hypercalcemia, initial management is medical and promotes the renal excretion of calcium.
- Intravenous fluids, preferably normal saline, are administered at a rapid rate (200-300 mL/hr) to reverse
intravascular volume contraction and promote renal excretion of calcium.
- Loop diuretics are added to the regimen to reduce the risk of volume overload and inhibit calcium
resorption in the loop of Henle. Patients with renal failure often cannot tolerate this large volume resuscitation;
instead, they should be dialyzed with low-calcium dialysate.
Steroids
- Steroids lower calcium by inhibiting the effects of vitamin D. They also have been shown to
decrease intestinal absorption of calcium, increase renal calcium excretion, and inhibit osteoclast-
activating factor.
- Steroids are particularly effective in the setting of hypercalcemia secondary to granulomatous
diseases, where hypercalcemia stems from vitamin D toxicity. The initial dose of hydrocortisone is
200-400 mg intravenously per day for 3-5 days.
- Steroids are ineffective in most cases of hypercalcemia associated with malignancy.
Calcitonin
- Calcitonin acts quickly (within 24-48 hrs) to lower serum calcium concentrations and is more
effective when used in combination with steroids.
Bisphosphonates
- Bisphosphonates are pyrophosphate analogs that have a high affinity for hydroxyapatite
in bone. They potently inhibit osteoclast activity for up to a month.
- In the hypercalcemia of malignancy, pamidronate (90 mg intravenously) or zoledronic acid (4 mg
intravenous initial treatment, 8 mg on retreatment) normalizes calcium concentrations in most
patients
- A single dose of a bisphosphonate lowers calcium concentrations, although recent evidence
suggests that zoledronic acid might become the bisphosphonate of choice because of its rapid onset
of action and its ability to lengthen the time to relapse two-fold; however, there also has been an
association between zoledronic acid and compromised renal function.
Surgery
- If a patient is diagnosed with primary hyperparathyroidism, parathyroidectomy can achieve cure.
management of
hypocalcaemia
- Patients with hypocalcaemia who are clinically stable can receive oral calcium.
- In emergent situations, 100-200 mg of calcium can be given intravenously as a bolus, and a central
vein should be used whenever possible. One milliliter of calcium chloride provides 27 mg of
elemental calcium, and 1 mL of calcium gluconate gives 9 mg.
- Calcium chloride elevates the calcium concentration after plasmapheresis for longer periods and is
the historically favored calcium replacement because there is a higher dose of elemental calcium in 1mL.
some specific
causes of
hypercalcemia
Hyperparathyroidism
(i) primary hyperparathyroidism
- The most common cause of primary hyperparathyroidism is a parathyroid adenoma (85%).
- Parathyroid hyperplasia affects all glands and is the underlying cause of primary
hyperparathyroidism in 10% of cases. It can be associated with the multiple endocrine
neoplasia I and IIa syndromes. Multiple endocrine neoplasia I includes hyperparathyroidism,
pituitary adenoma, and pancreatic tumors (most commonly insulinomas or gastrinomas).
Multiple endocrine neoplasia IIa includes hyperparathyroidism, medullary carcinoma of the
thyroid, and pheochromocytoma.
- Parathyroid carcinoma is a rare (<1% of cases) cause of primary hyperparathyroidism.
(ii) secondary hyperparathyroidism
- Secondary hyperparathyroidism results from stimuli outside the normal feedback loop.
For example, patients with renal failure have decreased renal conversion of 25-
hydroxyvitamin D to 1,25(OH)2D, resulting in less calcium absorption. In addition, these
patients have hyperphosphatemia. The cumulative effect is that these patients are
hypocalcemic, and PTH is secreted from the parathyroid glands.
(iii) tertiary hyperparathyroidism
- Tertiary hyperparathyroidism occurs when the parathyroid glands of these patients
become overactive and autonomous from normal negative feedback mechanisms. Patients
who fail medical therapy and acquire tertiary hyperparathyroidism develop clinical
sequelae such as calciphylaxis, and they should be referred for parathyroidectomy.
Hypercalcemia of Malignancy.
- Hypercalcemia of malignancy is most commonly secondary to the inappropriate release
of PTH-related peptide (PTHrp) from tumor cells. This leads to increased bone
resorption and decreased renal calcium excretion.
- PTHrp induced hypercalcemia is associated with squamous cell (e.g., lung), breast, prostate,
and (rarely) colon cancer as well as adult T-cell malignancies and multiple myeloma
Granulomatous Diseases.
- The association between hypercalcemia and granulomatous diseases such as sarcoidosis
occurs secondary to increased 1,25(OH)2D production that is independent from the
normal negative feedback mechanisms.
- Macrophages in granulomas produce 1,25(OH)2D.
- Other granulomatous disease such as tuberculosis, leprosy, coccidioidomycosis, and
histoplasmosis all have been associated with hypercalcemia via a similar pathway.
Diet and Drugs.
- Patients with elevated calcium concentrations should be screened to exclude dietary causes.
Large amounts of supplemental calcium or vitamin D (e.g., in the form of antacids) can cause
hypercalcemia.
symptoms
of hypocalcaemia
- Early symptoms of hypocalcemia include perioral numbness, paresthesias,
muscle cramps, and mild mental status changes such as irritability.
- As hypocalcemia becomes more severe, there can be neuromuscular and cardiac
findings, including Chvostek's and Trosseau's signs, as well as mental status changes,
seizures, tetany, hypotension, and acute heart failure.
- Chvostek's sign is elicited by tapping the facial nerve anterior to the ear, which
produces spasm of the muscles of the face; it has been shown to be positive in 10-30% of
people with normal calcium concentrations.
- Trousseau's sign is positive when pressure on the wrist induced by inflation of a blood
pressure cuff for 3-5 mins or tapping on the median nerve induces carpal spasm.
- Acute hypocalcemia decreases cardiac function by lengthening phase 2 of the
cardiac action potential, which results in prolongation of the ST segment and the
QT interval on electrocardiogram and can lead to VT
- Hypocalcemia can lead to cardiac failure, and this can be reversed with administration
of calcium.
causes
of hypercalcaemia
causes
of hypocalaemic
with metabolic
acidosis
indications for calcium administration:
investigation
of hypocalcaemia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-68-320.jpg)


![carbon monoxide
poisoning
[created by
Paul Young
02/10/07]
definition
aetiology
investigation
treatment
disposition
symptoms
- institute immediate oxygen therapy with 100% oxygen via non-rebreather
- institute cardiac monitoring and monitor pulse ox
- intubate comatose patients
CO is a colourless, odourless gas produced by incomplete combustion
of carbonacious materal
potential exposures include:
- fires
- stoves
- portable heaters
- automobile exhaust
- cigarette smoke
- charcoal grills
- propane-fueled forklifts
- gas powered concrete saws
- inhaling spray paint
- swimming behind a motor boat
- inhalation of methylene chloride which is found in degreasers,
solvents and paint removers (metabolised to CO in liver)
High index of suspicion is required when any of the suggestive symptoms are present
HbCO:
- elevated levels are significant; however, low levels do not rule out exposure
(especially if the patient has received 100% oxygen or if significant time has elapsed)
- smokers may have levels as high as 10%
- presence of fetal Hb may be read as an elevation of HbCO to 7%
ABG
- PaO2 should remain normal. Oxygen saturation is accurate only if measured
but not if calculated from PaO2
Bloods
- troponin (because myocardial ischaemia is frequently associated with exposure)
- FBE - look for mild leukocytosis
- coags
- lactate (may have lactic acidosis from tissue hypoxia)
- hyperglycaemia and hypokalaemia occur with severe intoxication
- Cr (acute renal failure may occur secondary to myoglobinuria)
- LFTs may be deranged
- MetHb (in differential for cyanosis with low oxygen saturation but normal PaO2)
- ethanol (confounding factor in may intential and unintentional poisonings)
- cyanide level (if cyanide toxicity is also suspected - eg industrial fire; cyanide
exposure is suggested by unexplained metabolic acidosis)
- admitted patients will require monitoring
- some patients require hyperbaric oxygen
- toxicity results from cellular hypoxia caused by impedance of oxygen delivery
- CO reversibly binds Hb 230-270xs more avidly than oxygen resulting in relative
anaemia. Binding of CO to Hb causes an increased binding of oxygen at the other
3 oxygen binding sites resulting in a leftward shift of oxyHb dissociation curve &
decreased availabiliity of oxygen the already hypoxic tissues
- CO binds cardiac myoglobin with even greater avidity than Hb resulting in myocardial
depression and hypotension that further exacerbates tissue hypoxia
- CO binds to cytochrome p450; also may cause brain lipid peroxidation and leukocyte
mediated inflammatory changes in the brain (a process inhibited by hyperbaric oxygen)
neonates and the in utero fetus are more vulnerable to CO toxicity because of the natural
leftward shift of the dissociation curve of fetal Hb, a lower baseline PaO2 and levels of HbCO
at equilibrium that are 10-15% higher than maternal levels
Acute poisoning:
- malaise, flu-like symptoms and fatigue
- dyspnoea on exertion
- chest pain and palpitations
- lethargy
- confusion
- depression
- impulsiveness
- distractability
- hallucinations
- agitation
- nausea, vomiting & diarrhoea
- abdominal pain
- headache and drowsiness
- dizziness, weakness and confusion
- visual disturbance, syncope and seizure
- incontinence
- memory disturbance
- bizarre neurological symptoms, coma
Chronic exposures:
- similar symptoms to above but also loss of dentations, gradual
onset of neuropsychiatric symptoms and cognitive impairment
signs
vital signs:
- tachycardia
- hypertension or hypotension
- hyperthermia
- tachypnoea (marked only occurs with severe intoxication)
classic cherry red skin is rare ("when you're cherry red you're dead")
ophthalmological signs:
- flame-shaped haemorrhages
- bright red retinal veins (a sensitive early sign)
- papilloedema
- homonymous hemianopsia
pulmonary oedema
- memory disturbance including retrograde amnesia and confabulation
- emotional lability, impaired judgement and decreased cognition
- coma
- gait disturbance
- brisk reflexes, apraxia, agnosia, blindness and psychosis
- long-term exposures or severe acute exposures frequently
result in long-term sequelae
- some individuals develop delayed neuropsychological symptoms;
2/3rds recover completely from these
Urine:
urinanalysis (+ve for albumin and glucose in chronic intoxication)
Imaging:
- obtain a CXR if significant pulmonary symptoms or prior to hyperbaric O2
- CT head with severe intoxication or change in mental status that does not
rapidly resolve (typically get low density lesions in the basal ganglia); positive
CT findings predict poor outcome
ECG
- sinus tachycardia is the most common abnormality
- arrhythmia may occur secondary to ischaemia or infarct
- continue 100% oxygen until patient is assymptomatic and levels of
CO are below 10% (some have suggested continuing until below 2%
in patients with cardiovascular or pulmonary compromise)
- consider immediate transfer of patients with cardiovascular or neurological
impairment to a hyperbaric facitiliy; persistent symptoms after 4 hours of
normobaric oxygen necessitate transfer to a hyperbaric center
- do not aggressively treat acidosis with a pH >7.15 because acidosis
shifts Hb dissociation curve right increasing tissue oxygen availability
(acidosis generally improves with oxygen therapy)
- be aware that nitrites used in cyanide poisoning kits cause metHb
and shift Hb dissociation curve further left. Combined CO and
cyanide intoxications may be treated with sodium thiosulphate 12.5g iv
to prevent leftward shift
all pregnant women and neonates need to be discussed with hyperbaric center](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-71-320.jpg)
![mechanisms
of arrhythmia
[created by
Paul Young
02/10/07]
general
1. fast or slow?
2. ventricular or supraventricular?
3. compromised or not?
4. does arrhythmia need management?
5. what is underlying substrate predisposing?
6. what is trigger?
7. will arrhythmia recur?
bradycardia
- blocks and bradys are caused by
impaired automaticity or conduction
- if one pacemaker fails another generally
takes over at a lower rate
- factors that impair pacemaker automaticity
or myocardial impulse conduction:
1. hypoxia
2. drugs (eg beta blockers)
3. electrolyte & pH disturbances
4. myocardial ischaemia
5. anything that enhances parasympathetic tone
(eg carotid sinus hypersensitivity)
tachycardia
general
mechanisms
1. reentrancy
2. increaed automaticity
3. triggered activity
reentrancy
- basic concept is that impulse reaches a point where it can go two
ways (path A or path B). If path A is blocked, then impulse travels
down path B only. However, when impulse reaches point where
paths A & B re-join, impulse is retrogradely conducted up path A
until it reaches then beginning and travels down path A creating a
reentry loop
- the blocks that lead to rentry are often transient & timing dependent.
- sometimes they do not even occupy a fixed anatomical
location (eg some forms of AF)
increased
automaticity
- cardiac tissue has a normal tendency to spontaneous depolarisation
- a variety of insults can lead to 'ectopic activity' such as:
1. local ischaemia
2. hypokalaemia
3. drugs
triggered
activity
- key concept is 'afterdepolarisation' where after a normal action potential,
the cellular transmembrane potential suddenly swings positive again,
& if the upswing is sufficient, a full depolarisation may occur again & again
- there are (at least) two different mechanisms of triggered activity and
these result in:
(i) early afterdepolarisations (EADs)
(ii) delayed afterdepolarisations (DADs)
- EADs occur before repolarisation has finished - there is a sudden upswing
in the transmembrane potential, which usually occurs in the context of a
prolonged action potential - for example with partial blockade of Ik, the inwardly
rectifying current that normally terminates the action potential
- DADs occur after membrane potential has returned to normal - here the
upswing occurs due to raised intracellular calcium levels
Vaughan-Williams
classification of
anti-arrhythmics
class I - sodium channel blockade
class II - beta adrenergic blockade
class III - prolongation of repolarisation often due to potassium channel blockade
class IV - calcium channel blockade
factors
contributing to
arrhythmogenesis
Structural influences:
(i) myocardial infarction - acute, healed, aneurysm
(ii) hypertrophy
(iii) myopathic ventricle - dilation, fibrosis
Transient influences:
(i) transient ischaemia / reperfusion
(ii) systemic factors
- hypoxia
- acidosis
- electrolyte abnormalities
(iii) neurophysiological factors
- autonomic tone
- endogenous catecholamines
(iv) toxicity
- proarrythmic drugs
- exogenous catecholamines
factors
facilitating
anti-arrhythmic
proarrythmia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-72-320.jpg)
![cardiac
output
measurement
general
- the standard is the Fick technique whereby CO = VO2/(CaO2 - CvO2)
; however, this requires sampling of the mixed venous blood & measurement
of VO2 by indirect calorimetry under steady state conditions
- measurements of equal accuracy can be obtained
by indicator or thermal dilution methods
measurement of cardiac output can be by several means:
1. invasive methods:
(i) indicator dilution
(ii) thermal indicator dilution
(iii) PICCO
(iv) LiDCO
(v) oesophageal doppler
(vi) TOE
2. non-invasive methods:
(i) doppler ultrasound
(ii) thoracic electrical bioimpedence
(iii) TTE
indicator
dilution
- a bolus of indicator is injected into the vena cava,
right heart or preferably the pulmonary artery
- the concentration of indicator reaching the systemic
circulation is plotted against time and cardiac output
is thereby calculated:
CO L/min = 60 x indicator dose [mg] / (average concentration [mg/L] x time [s])
- one of the problems with this technique is that recirculation
of the indicator occurs before the downslope is complete
- of the dyes used for this technique, indocyanide is the most popular.
It is non-toxic and has a relatively short half-life allowing repeated
measurement to be made; indicator dilution has also be described using
radioactive tracers such as human serum albumin or chromium labelled red
cells
thermal
indicator
dilution
- thermal indicator dilution is used routinely in the intensive care unit
- the principle is the same as for indicator dilution but the injection &
sampling are performed on the right side of the heart
-thermal dilution techniques have a number of advantages:
(i) the indicator is cheap and non-toxic
(ii) arterial puncture and blood withdrawal is not necessary
(iii) absence of recirculation (particularly important at low
output states where recirculation makes dye dilution inaccurate)
- disadvantages of thermal dilution include:
(i) requires passage and placement of a special catheter
(ii) mixing with venous blood may be incomplete
(iii) pulmonary arterial blood flow varies greatly with respiration
doppler
ultrasound
- when doppler ultrasound with a frequency of 1-10MHz is directed
along the long axis of the ascending aorta from a transducer in the
suprasteral notch, the sound is reflected back with a frequency
shift proportional to the velocity of blood flow.
- the blood flow velocity curve is integrated to give the average velocity
over time & the troke volume is the calculated by multiplying the average
velocity during each heart beat by the cross-sectional area of the aorta
- both continuous and pulsed doppler systems are in use.
- the continuous system can measure high velocities but averages the
frequency shifts along the whole length of the ascending aorta so that the
exact point at which the velocity is measured is unknown. It is therefore difficult
to know where to measure the diameter of the aorta.
- the pulsed Doppler again uses the same transducer to generate and receive
ultrasound but this produces shorter pulses instead of continuous ultrasound.
The advantage is that the beam can be focussed so that measurement is being
made
disadvantages of ultrasound measurement of cardiac output include:
(i) need for accurate measurement of aortic diameter (since area is pi R2)
(ii) fact aorta expands by up to 12% during systole
(iii) site of diameter measurement may not correspond to position velocity
is measured
(iv) shape of the velocity profile means that if beam is not aligned along
the aortic axis the measured velocity will be measured falsely low
thoracic
electrical
bioimpedence
- electrical impendence of tissues fluctuates according to the blood volume contained
therein. Changes in impedence occur due to cardiac & respiratory activity
- thoracic electrical bioimpedence underestimates cardiac output in septic shock
& aortic regurgitation & is inaccurate when there are intracardiac shunts or arrhythmias
partial
CO2
rebreathing
method
General:
- with this method, cardiac output is measured every 3 minutes
- a segment of dead space (150ml) is introduced into the breathing circuit
of a ventilated patient for 30-50s (it is assumed that although pulmonary
end-capillary, arterial and end-tidal PCO2 rise promptly, mixed venous PCO2
does not change during this brief period of rebreathing)
- CO = deltaCO2 elimination / (S x delta end-tidal CO2) where S is the slope of
the blood CO2 dissociation curve
- a correction for venous admixture is added based on FiO2 and SaO2
Problems:
(i) unsuitable for non-intubated patients
(ii) CO2 elimination may not reach steady state in the time available
(esp in chronic lung disease)
(iii) the value of S varies with Hb concentration
(iv) venous admixture cannot be calculated reliably from FiO2 and SaO2 when
there is significant V/Q scatter (eg chronic lung disease)
(v) overall lack of validation in chronic lung disease
inaccuracies arise from:
(i) motion artefact
(ii) electrical interference
(iii) tachycardia
(iv) dysrhythmias
(v) conduction defects
(vi) variations in functional residual capacity
(vii) chest deformities
(viii) pneumonectomy
(ix) pleural and pericardial effusion
(x) pulmonary oedema
(xi) chest tubes
(xii) pregnancy
(xiii) metal prostheses
(xiv) intracardiac shunts](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-73-320.jpg)
![cardiac
physiology
[created by
Paul Young
09/10/07]
morphology
electrical
properties
mechanical
properties
metabolism
cardiac ion
channels
general
key
features
1. branching cells
2. single central nucleus
3. visible striations
4. intercalated discs
5. T-tubules are located Z-lines rather than A-I junction
have intercalated discs where one fibre abuts another
& membranes of both fibres parallel each other through
an extensive series of folds (provide a strong unit between
fibres so that pull is transmitted)
along sides of fibres next to discs, cell membranes fuse
forming gap junctions allowing spread of conduction
compared
to skeletal
- contraction begins just after depolarisation
& lasts one & a half times as long as skeletal
- calcium entry via dihydropyridine receptors
triggers calcium release from the SR
isoforms
length-tension
relationships
- cardiac muscle is slow & has relatively low
ATPase activity (fibres are dependent on oxygen)
- two isoforms of MHCs (alpha predominates
in atria; beta predominates in ventricles)
phase 0 is depolarisation
phase 1 is initial repolarisation
phase 2 is plateau
phase 3 is late repolarisation
phase 4 is baseline
under basal conditions:
- 35% of caloric needs come from carbohydrate
- 5% from ketones & amino acids
- 60% from fat
supply
dependency](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-74-320.jpg)
![CPR & support
in pregnancy
[created by
Paul Young
02/10/07]
incidence
incidence of cardiac arrest during pregnancy is
estimated to be about 1 in 30,000 pregnancies
causes
ACLS
in pregnancy
modifications for the late-term pregnant woman are the following:
(i) more aggressive or prompt airway management,
(ii) attention to lateral displacement of the uterus, and
(iii) early consideration of perimortem cesarean delivery
drugs
- The use of sodium bicarbonate to reverse metabolic acidosis during cardiac
arrest has been questioned; its role in managing maternal acidosis is also
controversial.
- Animal studies suggest that bicarbonate crosses the placenta poorly
(although this finding may not be true in humans).
- Rapid correction of maternal (but not fetal) acidosis could lead to reduced
compensatory hyperventilation and normalization of maternal PaCO2, which
could result in a concomitant increase in fetal PaCO2 and potential worsening
of fetal acidosis
- There is little information regarding pharmacologic therapy during ACLS in
pregnant patients. The use of a-adrenergic agents theoretically may reduce
uteroplacental blood flow, but their actual clinical effect is unknown.
- In general, the same protocols for pharmacologic management of ACLS
should be used in pregnant and nonpregnant patients with cardiac arrest.
-The best chance for survival for the mother and fetus depends on rapid
resuscitation of the mother.
perimortem
caesarian
section
- recommended initiation of cesarean delivery within 4 minutes of maternal
cardiac arrest if circulation has not been restored and recommended fetal
delivery within 5 minutes.
- Given the number of reports of neonatal survival without adverse neurologic
sequelae when delivery occurred well after 5 minutes of maternal cardiac
arrest, this rule should not be taken as absolute.
somatic
support
of brain
dead
mother
- longest period of somatic support after maternal brain death (107 days) and the
earliest gestational stage (15 weeks) at which such support was begun and led to
successful delivery (at 32 weeks’ gestation)
issues include:
(i) cardiovascular support
(ii) respiratory support
(iii) nutritional support
(iv) endocrine support
(v) temperature regulation
(vi) fetal monitoring](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-75-320.jpg)

![cerebral
neoplasm
[created
by Paul
Young
24/11/07]
general
- Malignant primary tumors of the central nervous system (CNS) have a mortality rate of
6 per 100,000. An approximately equal number of benign tumors of the CNS are
diagnosed, with a much lower mortality rate.
- Glial tumors account for 50 to 60% of primary brain tumors, meningiomas for 25%,
schwannomas for 10%, and all other CNS tumors for the remainder.
- Brain and vertebral metastases from systemic cancer are more prevalent than primary
CNS tumors. About 15% of patients who die of cancer have symptomatic brain
metastases; an additional 5% suffer spinal cord involvement. Brain and spinal metastases
therefore pose a major problem in the management of systemic cancer.
clinical
features
- Brain tumors usually present with one of three syndromes:
(1) subacute progression of a focal neurologic deficit;
(2) seizure; or
(3) nonfocal neurologic disorder such as headache, dementia, personality change, or gait
disorder.
- The presence of systemic symptoms such as malaise, weight loss, anorexia, or fever
suggests a metastatic rather than a primary brain tumor.
- Progressive focal neurologic deficits result from compression of neurons and white
matter tracts by expanding tumor and surrounding edema.
- Less commonly, a brain tumor presents with a sudden stroke-like onset of a focal
neurologic deficit. Although this presentation may be caused by hemorrhage into the
tumor, often no hemorrhage can be demonstrated and the mechanism is obscure. Tumors
frequently associated with hemorrhage include high-grade gliomas and metastatic
melanoma and choriocarcinoma.
- Nonfocal neurologic dysfunction usually reflects increased intracranial pressure (ICP),
hydrocephalus, or diffuse tumor spread. Tumors in some areas of the brain may produce
behavioral disorders; for example, frontal lobe tumors may present with personality
change, dementia, or depression.
- Seizures may result from disruption of cortical circuits. Tumors that invade or compress
the cerebral cortex, even small meningiomas, are more likely to be associated with
seizures than subcortical neoplasms.
- Headache may result from focal irritation or displacement of pain-sensitive structures or
from a generalized increase in ICP. A headache that worsens rather than abates with
recumbency is suggestive of a mass lesion.
- Headaches from increased ICP are usually holocephalic and episodic, occurring more
than once a day. They typically develop rapidly over several minutes, persist for 20 to 40
min, and subside quickly. They may awaken the patient from a sound sleep, generally 60
to 90 min after retiring, or may be precipitated by coughing, sneezing, or straining.
Vomiting may occur with severe headaches.
- As elevated ICP becomes sustained, the headache becomes continuous but varying in
intensity. Elevated ICP may cause papilledema, although it is often not present in infants
or patients >55 years.
investigation
Laboratory Examination
- Primary brain tumors typically do not produce serologic abnormalities such as an
elevated sedimentation rate or tumor-specific antigens associated with systemic cancers.
- Lumbar puncture may precipitate brain herniation in patients with mass lesions and should be
performed only in patients with suspected CNS infection or meningeal metastasis. Findings in
the cerebrospinal fluid (CSF) of patients with primary and metastatic nervous system tumors
may include raised opening pressure, elevated protein level, and a mild lymphocytic pleocytosis.
- The CSF rarely contains malignant cells, with the important exceptions of leptomeningeal metastases,
primary CNS lymphoma, and primitive neuroectodermal tumors, including medulloblastoma.
Neuroimaging
- Computed tomography (CT) and magnetic resonance imaging (MRI) can reveal mass
effect and contrast enhancement.
- Mass effect reflects the volume of neoplastic tissue as well as surrounding edema.
- Brain tumors typically produce a vasogenic pattern of edema, with accumulation of
excess water in white matter.
- Contrast enhancement reflects a breakdown of the blood-brain barrier within the tumor, permitting
leakage of contrast agent. Low-grade gliomas typically do not exhibit contrast enhancement.
primary
tumours
Astrocytomas
- Tumors with astrocytic cytologic features are the most common primary intracranial neoplasms.
The most widely used histologic grading system is the World Health Organization four-tiered grading system.
Grade I is reserved for special histologic variants of astrocytoma that have an excellent prognosis after surgical
excision. These include juvenile pilocytic astrocytoma, subependymal giant cell astrocytoma (which occurs in
patients with tuberous sclerosis), and pleiomorphic xanthoastrocytoma. At the other extreme is grade IV,
glioblastoma multiforme, a clinically aggressive tumor. Astrocytoma (grade II) and anaplastic astrocytoma
(grade III) are intermediate in their histologic and clinical manifestations.
Oligodendrogliomas
- Oligodendrogliomas, which comprise about 15% of gliomas in adults, have a more benign course and are more
responsive to cytotoxic treatment than astrocytomas. Five-year survival is >50%, and 10-year survival is 25 to 34%.
- As a rule, oligodendrogliomas are less infiltrative than astrocytomas, permitting more complete surgical excision.
Histologic features of mitoses, necrosis, and nuclear atypia are associated with a more aggressive clinical course.
If these features are prominent, the tumor is termed an anaplastic oligodendroglioma.
Ependymomas
- In adults ependymomas are typically located in the spinal canal, especially in the
lumbosacral region. Imaging with CT or MRI scans reveals ependymomas as uniformly
enhancing masses that are relatively well demarcated from adjacent neural tissue.
Germinomas
- These tumors most commonly present during the second decade of life, generally at
sites within or adjacent to the third ventricle, including the pineal region.
- Germinomas are the most frequent variety of germ cell tumor, a tumor type arising in midline structures and
including teratoma, yolk sac tumor (endodermal sinus tumor), embryonal carcinoma, and choriocarcinoma.
- Germinomas of the CNS may be benign but are more often aggressive and invasive.
- Germinomas are generally radiosensitive and chemosensitive. Five year survival is >85%.
Primary CNS Lymphoma
- These are high-grade B cell malignancies that present within the neuraxis without evidence of systemic lymphoma.
They occur most frequently in immunocompromised individuals, specifically organ transplant recipients or patients
with AIDS. In immunocompromised patients, CNS lymphomas are invariably associated with Epstein-Barr virus
infection of the tumor cells.
- The prognosis of primary CNS lymphoma is poor compared to histologically similar lymphoma occurring outside
the CNS. Many patients experience a dramatic clinical and radiographic response to glucocorticoids; however, relapse
almost invariably occurs within weeks. The mainstay of definitive therapy is chemotherapy followed in patients <60
years with whole-brain irradiation.
Meningiomas
- Meningiomas are derived from mesoderm, probably from cells giving rise to the arachnoid granulations. These tumors
are usually benign and attached to the dura. They may invade the skull but only infrequently invade the brain.
- Meningiomas may be found incidentally on a CT or MRI scan or may present with a focal seizure, a slowly
progressive neurologic deficit, or symptoms of raised ICP. The radiologic image of a dural-based, extraaxial
mass with dense, uniform contrast enhancement is essentially diagnostic, although a dural metastasis must
also be considered.
- Total surgical resection of benign meningiomas is curative. If a total resection cannot be achieved,
local external beam radiotherapy or stereotaxic radiosurgery reduces the recurrence rate to <10%.
Medulloblastomas and Primitive Neuroectodermal Tumors (PNET)
- These highly cellular malignant tumors are thought to arise from neural precursor cells. Medulloblastomas of the
posterior fossa are the most frequent malignant brain tumor of children. PNET is a term applied to tumors
histologically indistinguishable from medulloblastoma but occurring either in adults or supratentorially in children.
In adults, >50% present in the posterior fossa. These tumors frequently disseminate along CSF pathways.
- Aggressive treatment can result in prolonged survival, although half of adult patients
relapse within 5 years of treatment.
Schwanomas:
- These tumors are also called neuromas, neurinomas, or neurolemmomas. They arise from Schwann cells
of nerve roots, most frequently in the eighth cranial nerve (vestibular schwannoma, formerly termed
acoustic schwannoma). The fifth cranial nerve is the second most frequent site; however, schwannomas
may arise from any cranial or spinal root except the optic and olfactory nerves
secondary
tumours
- The large majority of brain metastases disseminate by hematogenous spread. The anatomic distribution
of brain metastases generally parallels regional cerebral blood flow, with a predilection for the gray matter
-white matter junction and for the border zone between middle cerebral and posterior cerebral artery distributions.
- The lung is the most common origin of brain metastases; both primary lung cancer (adenocarcinoma
and small cell lung cancer) and cancers metastatic to the lung can metastasize to the brain.
- Breast cancer (especially ductal carcinoma) has a propensity to metastasize to the cerebellum
and the posterior pituitary gland. Moreover, breast cancer that metastasizes to bone tends not
o metastasize to the brain.
- Other common origins of brain metastases are gastrointestinal malignancies, and melanoma.
- Certain less common tumors have a special propensity to metastasize to brain, including germ
cell tumors and thyroid cancer.
- By contrast, prostate cancer, ovarian cancer, and Hodgkin's disease rarely metastasize to the brain.
treatment
symptomatic treatment:
- Glucocorticoids decrease the volume of edema surrounding brain tumors and improve neurologic
function; dexamethasone (12 to 20 mg/d in divided doses orally or intravenously) is used because
it has relatively little mineralocorticoid activity.
- Gliomas and primary CNS lymphomas are associated with an increased risk for deep vein thrombosis
and pulmonary embolism, probably because these tumors secrete procoagulant factors into the systemic
circulation. Even though hemorrhage within gliomas is a frequent histopathologic finding, patients appear
to be at no increased risk for symptomatic intracranial bleeding following treatment with an anticoagulant.
- Prophylaxis with low-dose subcutaneous heparin should be considered for patients with brain
tumors who have lower limb immobility, which places them at risk for deep venous thrombosis.
- Tumors that involve the cerebral cortex or hippocampus may produce epilepsy. Anticonvulsants
are therefore used therapeutically and prophylactically; phenytoin, carbamazepine, and valproic
acid are equally effective. If the tumor is subcortical in location, prophylactic anticonvulsants are
unnecessary.
specific therapies:
- include surgical excision or debulking, radiotherapy, chemotherapy
- experimental therapies include gene therapy, immunotherapy, intraarterial chemotherapy, and chemotherapy
administered following osmotic disruption of the blood-brain barrier.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-77-320.jpg)
![cerebral
oedema
[created
by Paul
Young
26/11/07]
general
- Cerebral edema is a potentially devastating complication of various acute neurologic
disorders.
- Its successful treatment may save lives and preserve neurologic function.
- Cerebral edema may be comprehensively defined as a pathologic increase in the
amount of total brain water content leading to an increase in brain volume.
patho-
physiology
- Edema in the brain may be topographically classified into focal or global.
(i) Focal edema generates a pressure gradient with adjacent regions and may result in tissue
shift and herniation. Examples of focal edema can be found around tumors, hematomas,
and infarctions.
(ii) Global edema diffusely affects the whole brain and, when critical, it may cause intracranial
hypertension, compromise perfusion, and lead to generalized ischemia. Cardiopulmonary arrest,
severe traumatic injury, and fulminant liver failure are common causes of global cerebral edema.
- A different classification based on the pathophysiologic mechanisms responsible for the production
of the edema classifies it into 3 types: cytotoxic, vasogenic, and interstitial.
(i) In cytotoxic edema, the increased water content is localized intracellularly and is due to the failure
of ionic pumps that normally maintain cellular homeostasis. Ischemia and profound metabolic
derangements are the most common causes. Cytotoxic edema preferentially affects gray matter
(ii) In vasogenic edema the main problem is centered in a disruption of the blood-brain barrier,
leading to increased permeability and escape of fluid from the intravascular to the extravascular,
extracellular space. It accompanies tumors, inflammatory lesions, and traumatic tissue damage.
Vasogenic edema tends to predominate in the white matter.
(iii) Interstitial edema results from increased transependymal flow from the intraventricular
compartment to the brain parenchyma; it typically occurs in the setting of obstructive hydrocephalus.
- the clinical manifestations of brain edema tend to be similar regardless of whether the edema is
cytotoxic or vasogenic. In fact, both types frequently coexist. For example, early after an
ischemic brain infarction cytotoxic edema predominates, but later vasogenic edema becomes
the major cause of mass effect as the blood-brain barrier loses continuity and local inflammation
develops.
clinical
manifestations
- It is often not simple to distinguish the contribution of brain edema to the condition of a
patient solely on the basis of the clinical examination.
- Worsening focal deficits may be seen in patients with localized edema, but most
commonly the development or progression of edema results in diminished level of
consciousness due to raised intracranial pressure (ICP).
- Herniation is the most feared consequence.
investigation
- CT scan reveals edema as an abnormal hypodense signal. When diffuse, it provokes
effacement of the gray white matter junction, loss of differentiation of the lenticular
nucleus, and decreased visualization of the sulci, insula, and cisterns while the presence
of vasogenic edema can be inferred from the appearance of hypodensity following the
course of white matter tracts,
- CT is not very helpful to distinguish vasogenic from cytotoxic edema.
- MRI shows edema as hypointense signal in T1-weighted sequences and hyperintense
signal in T2-weighted and FLAIR sequences. Delineation of the spread of edema
is much clearer with MRI.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-78-320.jpg)
![cerebral
venous
sinus
thrombosis
[created
by Paul
Young
22/11/07]
causes,
risk
factors
&
locations
pathogenesis
(i) occlusion of the cerebral veins
- causes localized edema of the brain and venous infarction. Pathological examination shows
enlarged, swollen veins, edema, ischemic neuronal damage, and petechial hemorrhages. The
latter can merge and become large hematomas, which have a characteristic appearance on
computed tomographic scans.
(ii) occlusion of major venous sinuses
- lead to the development of intracranial hypertension. Normally, the cerebrospinal fluid is
transported from the cerebral ventricles through the subarachnoid spaces at the base and surface
of the brain to the arachnoid villi, where it is absorbed and drained into the superior
sagittal sinus. Thrombosis of the sinuses leads to increased venous pressure, impaired
absorption of cerebrospinal fluid, and consequently, increased intracranial pressure.
The obstruction to the drainage of cerebrospinal fluid is located at the end of its transport
pathway, and no pressure gradient develops between the subarachnoid spaces at
the surface of the brain and the ventricles. Hence, the ventricles do not dilate, and hydrocephalus
does not normally complicate sinus thrombosis.
- About one fifth of patients with sinus thrombosis have intracranial hypertension only, without
signs of cortical vein thrombosis
clinical
features
- Infectious cavernous sinus thrombosis is characterized by headache, fever, and
eye symptoms such as periorbital edema, proptosis, chemosis, and paralysis of eye
movements due to involvement of the oculomotor, abducent, or trochlear nerves.
- Fundoscopic examination will reveal papilledema. Severe papilledema can cause
transient visual impairments, and even permanent blindness, if left untreated.
- The most frequent but least specific symptom of sinus thrombosis is severe headache,
which is present in more than 90 percent of adult patients. It usually increases gradually
over a couple of days but can also start in a split second, mimicking a subarachnoid
hemorrhage.
- Cerebral lesions and neurologic signs develop in half of patients with sinus thrombosis.
Characteristic, but rare, is the occurrence of unilateral hemispheric symptoms such as
hemiparesis or aphasia, followed within days by symptoms from the other hemisphere;
these are caused by the development of cortical lesions on both sides of the
superior sagittal sinus.
- Seizures occur in about 40 percent of patients, a far higher percentage than in
patients with arterial stroke. Seizures are limited and focal in 50 percent of these patients
but may generalize to a life-threatening status epilepticus.
- Thrombosis of the deep venous system - the straight sinus and its branches - causes
centrally located, often bilateral thalamic lesions, with behavioral symptoms such as
delirium, amnesia, and mutism, which can be the only manifestation of sinus thrombosis.
- If large unilateral infarcts or hemorrhages compress the diencephalons and brain stem,
patients may become comatose or die from cerebral herniation if untreated. Other
causes of coma are involvement of the thalamus and generalized seizures.
- Patients with isolated intracranial hypertension have headache but no other neurologic
symptoms, with the exception of diplopia due to involvement of the sixth nerve when the
intracranial pressure is quite high.
investigation
General:
- Although the clinical presentation is highly variable, the diagnosis should be considered in young and
middle-aged patients with recent unusual headache or with stroke-like symptoms in the absence of the
usual vascular risk factors, in patients with intracranial hypertension, and in patients with CT evidence
of hemorrhagic infarcts, especially if theinfarcts are multiple and not confined to the arterial vascular
territories. The average delay from the onset of symptoms to the diagnosis is seven days.
MRI:
- The most sensitive examination technique is MRI in combination with magnetic resonance venography.
T1-weighted and T2-weighted MRI will show a hyperintense signal from the thrombosed sinuses. The
characteristics of the signal depend on the age of the thrombus and are isointense on T1-weighted images
during the first five days and after one month.
- The combination of an abnormal signal in a sinus and a corresponding absence
of flow on magnetic resonance venography confirms the diagnosis of thrombosis
CT scanning
- CT scanning is a useful technique for the initial examination, to rule out other acute cerebral
disorders and to show venous infarcts or hemorrhages, but its results can also be entirely
normal. High-resolution CT equipment may show the thrombus as a hyperintense signal
in a sinus or even in the cortical veins (the "cord sign"). CT venography is a promising
new technique for creating images of the cerebral venous system.
Cerebral angiography
- If the diagnosis is still uncertain after MRI or CT venography has been
performed, cerebral angiography may be indicated.
- Angiography provides better details of the cerebral veins and hence is useful in the
diagnosis of rare cases of isolated thrombosis of the cortical veins without sinus thrombosis.
- Angiography also shows dilated and tortuous ("corkscrew") veins, which are evidence of
thrombosis downstream in the sinuses.
treatment
general measures
- The combination of acutely increased intracranial pressure and large venous infarcts is dangerous, and
patients may die within hours from cerebral herniation. Impaired consciousness and cerebral hemorrhage
are associated with a poor outcome,but even patients with these manifestations can make a remarkable
recovery.
- The priority of treatment in the acute phase is to stabilize the patient's condition and to prevent or reverse
cerebral herniation. This may require the administration of intravenous mannitol, surgical removal of the
hemorrhagic infarct, or decompressive hemicraniectomy.
- It is not known whether the administration of corticosteroids in the acute phase improves outcome.
- Possible causes of sinus thrombosis, such as infections, should be searched for and treated.
anticoagulation
- The most obvious treatment option is anticoagulation with heparin to arrest the thrombotic process
- However, anticoagulant treatment has raised much controversy because of the tendency of venous
infarcts to become hemorrhagic: about 40 percent of all patients with sinus thrombosis have a
hemorrhagic infarct even before anticoagulant treatment is started.
- The effect of anticoagulant treatment has been examined in three small, randomized clinical trials.
- The first trial compared the effect of intravenous heparin with that of placebo and was stopped
after only 10 patients had been included in each treatment group, because an interim analysis showed
a significant benefit with heparin, according to the investigators.
- A repeated analysis, which was based on the usual scales of stroke outcome, did not show a statistically
significant difference between the effect of heparin and that of placebo. Also, the average delay of four
weeks from the onset of symptoms to the beginning of treatment was exceptionally long.
- The second study compared the effect of fixed high-dose, subcutaneous nadroparin
with that of placebo in 60 patients and found no statistically significant difference. This study was criticized
for an imbalance at baseline, which may have favored the placebo group.
- The third study compared the effect of intravenous unfractionated heparin with that of placebo in 57
women from India who had puerperal sinus thrombosis but in whom the diagnosis had not been confirmed
by MRI or angiography.
- A meta-analysis of these studies showed a nonsignificant reduction in the pooled relative risk of death or
dependency of 0.46 (95 percent confidence interval, 0.16 to 1.31).
- A new trial with enough power to demonstrate a similar effect of treatment would require the recruitment of
300 patients. With a rare disease such as sinus thrombosis, this would be challenging but feasible.
- Most neurologists now start treatment with heparin as soon as the diagnosis is confirmed, even in the presence
of hemorrhagic infarcts. This treatment was applied to more than 80 percent of the 624 patients in a recent
prospective study. In this study, 79 percent of the patients recovered, 8 percent had minor handicaps, 5
percent were severely handicapped, and 8 percent died.
- The optimal duration of oral anticoagulant treatment after the acute phase is unknown. Recurrent sinus
thrombosis occurs in 2 percent of patients, and about 4 percent of patients have an extracranial thrombotic event
within one year.
- Usually, vitamin K antagonists are given for six months after a first episode of sinus thrombosis, or longer in the
presence of predisposing factors, with a target international normalized ratio of 2.5.
thrombolysis
- Endovascular thrombolysis can be attempted with the administration of a thrombolytic enzyme, usually
urokinase, into the sinus, sometimes in combination with mechanical thrombo-aspiration. Published reports
are limited to case reports and uncontrolled studies, from which it is impossible to conclude that the results
associated with endovascular thrombolysis are superior to those with systemic heparin.
- Until better evidence is available, endovascular thrombolysis may be applied at centers where the staff have
experience in interventional radiology, and this treatment method should be restricted to patients with a poor prognosis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-79-320.jpg)

![clinical
features
of DKA
& HONK
[created
by Paul
Young
01/12/07]
general
- DKA & HONK are life threatening syndromes caused by metabolic
derangement associated with diabetes mellitus
- DKA is approximately three times as common as HONK in patients
presenting with hyperglycaemic syndromes
- most deaths due to diabetic emergencies that are appropriately managed
are due to coexisting disease such as myocardial infarction
DKA
pathophysiology
- DKA is a syndrome of hyperglycaemia, metabolic acidosis, ketosis & severe volume depletion.
- DKA occurs in insulin dependent diabetics & severe insulin deficiency is the hallmark of this syndrome;
raised levels of stress hormones (GH, glucagon, catecholamines & cortisol) are also a feature
- hyperglycaemia results in a glucose load that overwhelms the resorptive capacity
of the renal tubules resulting in osmotic diuresis with fluid & electrolyte depletion
- the lack of insulin causes increased lipolysis & the formation of ketoacids
epidemiology
- accounts for approximately 6% of all diabetic admissions to hospital
& occurs in a younger age group than HONK
precipitating factors
- precipitating factors associated with the development of DKA include:
(i) lack of insulin due to previously undiagnosed diabetes mellitus or non-compliance
(ii) physical stressors such as acute infective illness, myocardial infarction, SIRS (eg
pancreatitis), glucocorticoid, phenytoin or diuretic therapy
(iii) post surgical management
(iv) substance abuse
clinical features
- presenting clinical features of DKA reflect the underlying metabolic
derangements of dehydration, ketosis & metabolic acidosis & include:
(i) thirst & polyuria
(ii) tachycardia and hypotension
(iii) reduced skin turgor
(iv) dry mucous membranes
(v) Kussmaul respiration & ketotic fetor
(vi) core temperature is often reduced
laboratory tests
- laboratory tests supporting the diagnosis of DKA include
(i) hyperglycaemia
(ii) spurious hyponatraemia
(iii) preserved or high levels of serum potassium (reflecting the acid-base
status and not the severe total body depletion of potassium that is present)
(iv) variable levels of calcium, magnesium & phosphate (although these are
usually low or become low on commencement of therapy)
(v) hyperosmolality
(vi) elevated serum urea and creatinine levels
(vii) elevated serum ketone levels as measured by the concentrations of beta hydroxybutyrate
and acetoacetate [3-hydroxybutyrate concentrations in plasma are 2-3 times those of
acetoacetate but in acidotic states this ratio is increased further. As therapy improves acidosis,
levels of acetoacetate rise and methods that measure only acetoacetate concentrations in urine
may suggest ketonuria is worsening
(viii) white cell count may be elevated and does not necessarily reflect infection
(ix) amylase is often elevated (without pancreatitis)
HONK
pathophysiology
- the defining features of HONK include hyperglycaemia, dehydration,
& hyperosmolality without ketoacidosis
- the main differentiation from DKA appears to be the presence of at least some insulin (ie relative,
rather than absolute lack of insulin), more variable levels of stress hormones or conterregulatory
hormones & the fact renal dysfunction is commonly present
- renal dysfunction & impaired tubular function results in less capacity to deal with high solute &
osmotic loads. This together with impaired water intake results in severe dehydration.
epidemiology:
- less common that DKA, occurs in an older age group & has a higher mortality rate
precipitating factors include all of those listed for DKA plus:
(i) mental obtundation, dementia or physical impairment limiting access to water
(ii) severe dehydration
(iii) renal dysfunction
(iv) inappropriate diuretic use as well as steroids, beta blockers & phenytoin are risk factors
clinical features
- more commonly associated with obtundation than DKA
laboratory tests
- laboratory tests are similar to those for DKA but differ in degree
(i) serum glucose levels are usually higher
(ii) serum sodium levels may be normal ( inappropriately for serum glucose)
(iii) markers of renal dysfunction are worse
(iv) hyperosmolality is more marked
(v) metabolic acidosis is not as severe
(vi) anion gap & serum ketone ketone levels are normal
metabolic
derangement
- the main metabolic derangements that result in morbidity & must be urgently
addressed in the management of both DKA & HONK are dehydration, insulin
deficit, electrolyte depletion & metabolic acidosis
- although there is no consensus on the ideal approach to fluid management
in these patients, prompt restoration of the circulation with isotonic fluid,
followed by more moderate replacement of the water deficit using hypotonic
fluid are the underlying principles
- electrolyte depletion is treated by appropriate replacement of sodium,
potassium, magnesium, phosphate & calcium as indicated by frequent
testing during the early phase after presentation
- metabolic acidosis rarely requires specific therapy & corrects with volume
expansion and insulin therapy. Bicarbonate is not generally advocated
due to the possibilities of hypokalaemia, intracellular acidosis, reduced
myocardial contractility and reduced tissue oxygenation
neurological
sequelae
altered mental state
- patients who present with DKA or HONK commonly have an altered mental
state which may range from delirium to coma. Often the patient is very unwell
and as a consequence is stuporous and uncommunicative; less commonly
delerium is the major feature.
- often improves rapidly with rehydration and correction of acidosis
- there is no good correlation between glucose level, osmolality or pH and the
patient's presenting mental status which appears to be more a function of the
patient's general health, comorbidities and the precipitating cause
- localising signs and lack of improvement with correction of metabolic disturbance
mandate further investigation
cerebral oedema
- rapid correction of hyperglycaemia and hyperosmolality is associated with the
development of cerebral oedema in patients with hyperglycaemic syndromes
[animal studies suggest it is correction of hyperglycaemia and hyperosmolality
rather than sodium movement or acidosis that are important]
- the use of isotonic rather than hypotonic solutions for rehydration and avoidance
of over rapid correction of hyperglycaemia appear to offer protection against the
development of cerebral oedema
- cerebral oedema is more common in DKA than HNKS & is more common in the young
- manifests with either prolonged altered mental state or a new development of altered
mental state
- in adults good supportive care is generally all that is required & manifestations
gradually abate over a few days; however, in children cerebral oedema is associated
with considerable mortality & urgent treatment with mannitol is often required
seizures:
- focal and generalised seizures are common in patients with
hyperglycaemic syndromes and may be resistant to treatment](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-81-320.jpg)
![clinical
features
of thyroid
storm
[created
by Paul
Young
02/12/07]
clinical
features of
thyrotoxicosis
general
- In the spectrum of endocrine emergencies, thyroid storm ranks as one of the most
critical illnesses. Recognition and appropriate management of life-threatening
thyrotoxicosis is vital to prevent the high morbidity and mortality that may accompany
this disorder.
- The incidence of thyroid storm has been noted to be less than 10% of patients
hospitalized for thyrotoxicosis; however, the mortality rate due to thyroid storm ranges
from 20 to 30%.
definitions
- hyperthyroidism refers to disorders that result from overproduction of hormone from
the thyroid gland, thyrotoxicosis refers to any cause of excessive thyroid hormone
concentration. Thyroid storm represents the extreme manifestation of thyrotoxicosis.
- The point at which thyrotoxicosis transforms to thyroid storm is controversial.
However, clinically, it is prudent to assume that someone with severe thyrotoxicosis has
impending thyroid storm, and to treat them aggressively, rather than focus on specific
definitions.
aetiology
diagnostic
criteria
Underlying aetiology
- The most common underlying cause of thyrotoxicosis in cases of thyroid storm is
Graves' disease. Graves' disease is mediated by the thyrotropin receptor antibodies that
stimulate excess and uncontrolled thyroidal synthesis and secretion of thyroid hormones
(thyroxine [T4] or triiodothyronine [T3]).
- thyroid storm can also occur with a solitary toxic adenoma or toxic multinodular goiter.
- Rare causes of thyrotoxicosis leading to thyroid storm include hypersecretory thyroid
carcinoma, thyrotropin-secreting pituitary adenoma, struma ovarii/teratoma,
and human chorionic gonadotropia-secreting hydatidiform mole.
- Other causes include interferon alpha and interleukin-2-induced thyrotoxicosis during
treatment for other diseases, such as viral hepatitis and HIV infection
Precipitating events
- a precipitating event usually ignites the transition from thyrotoxicosis to thyroid
storm. Thyroid storm can be precipitated by systemic insults such as surgery, trauma,
myocardial infarction, pulmonary thromboembolism, diabetic ketoacidosis, parturition, or
severe infection.
- Thyroid storm has also been reported to be precipitated by the discontinuation of
antithyroid drugs, excessive ingestion or intravenous administration of iodine (eg,
radiocontrast dyes, amiodarone), radioiodine therapy, and even pseudoephedrine
and salicylate use.
Investigation
- In thyroid storm, the pattern of elevated free T4 and free T3 with a depressed
thyrotropin (less than 0.05 mU/mL) are comparable to the levels seen in thyrotoxicosis.
- Other possible laboratory findings associated with thyrotoxicosis include
hyperglycemia, hypercalcemia, elevated alkaline phosphatase, leukocytosis,
and elevated liver enzymes.
- The hyperglycemia tends to occur because of a catecholamine-induced inhibition of
insulin release, and increased glycogenolysis. Mild hypercalcemia and elevated alkaline
phosphatase can occur because of hemoconcentration and enhanced thyroid hormone-
stimulated bone resorption
- Radiologic imaging is not required to make the diagnosis of thyrotoxicosis or thyroid
storm. Although not always indicated for diagnosis, given the urgency and clinical
context, nuclear medicine imaging with radioactive iodine uptake and scanning would
reveal a greatly increased uptake of radioiodine as early as 1 or 2 hours after
administration of the isotope, indicating rapid intraglandular turnover of iodine.
- It is frequently helpful, and generally easier in the setting of an intensive care unit, to
obtain a thyroid sonogram with Doppler flow to assess thyroid gland size, vascularity,
and the presence of nodules that may require further attention. Typically, a thyroid gland
secreting excessive hormones would be enlarged and have enhanced Doppler flow. On
the other hand, in the setting of subacute, postpartum, or silent thyroiditis, or exogenous
causes of hyperthyroidism, the thyroid gland would be expected to be small, with
decreased Doppler flow.
- Electrocardiogram manifestations of thyrotoxicosis most commonly include sinus
tachycardia and atrial fibrillation. Sinus tachycardia occurs in approximately 40% of
cases, whereas atrial fibrillation occurs in 10% to 20% of patients who have
thyrotoxicosis, with a tendency to occur more commonly in patients older than 60, who
are more likely to have underlying structural heart disease.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-82-320.jpg)



![coma
[created
by Paul
Young
05/11/07]
general
consciousness:
- a state of awareness of the self and the environment
- depends on
(i) wakefulness (arousal) and its underlying neural substrate the reticular activing system & thalamus
(ii) awareness which relies on the functioning cerebral cortex
arousal:
(i) alert refers to a normal state of arousal
(ii) stupor describes a state where a strong stimulus can transiently restore wakefulness
(iii) lethargy describes a state between alertness and stupor
(iv) coma is characterised by an uninterrupted loss of capacity for arousal
structural
causes of
coma
- intracranial mass lesions that cause coma may be located in supratentorial compartment or infratentorial compartment
- coma is caused by compression of the RAS and disruption of axoplasmic flow
- The rate of evolution of a mass dictates whether the anatomical distortion precedes
(in slowly evolving lesions) or parallels the patient's deterioration of wakefulness
supratentorial herniation syndromes:
(i) central herniation:
- results from caudal displacement by deep midline supratentorial masses, large space
occupying hemisphere lesions or large unilateral or bilateral extra-axial lesions
- bilateral symmetrical displacement of the supratentorial contents occurs
through the tentorial notch into the posterior fossa
- clinical manifestations progress as follows with increasing herniation:
1. Impaired alertness (early)
2. Pupils become small but remain reactive
3. Bilateral upper motor neuron signs develop
4. Cheyne stoke breathing, grasp reflexes and roving eye movements develop
5. Midbrain compression leads to fixed mid position pupils
6. Spontaneous extensor posturing may occur
7. Variable breathing patterns develop
8. Autonomic cardiovascular and respiratory functions cease as medullary centres fail
(ii) uncus herniation
- results from laterally placed hemisphere lesions which cause side to side cerebral
displacement as well as transtentorial herniation
- focal hemisphere dysfunction precedes ipsilateral compression of the 3rd cranial nerve resulting in an enlarged pupil that
responses sluggishly followed by a fixed dilated pupil and an oculomotor palsy (with eye turned downward and outward)
- the ipsilateral posterior cerebral artery can become compressed as it crosses the tentorium causing occipital lobe ischaemia on the same side
- a hemiparesis may develop on the same side of the lesion due to compression of the opposite cerebral peduncle against
the contralateral tentorial edge (Kernohan's notch)
- with increased mass effect herniation proceeds in the same pattern as seen with central herniation
infratentorial lesions:
- acute intrinsic lesions of the brainstem cause abrupt onset of coma and are
associated with abnormal neuro-ophthalmological findings
- pinpoint pupils are caused by disruption of pontine sympathetic fibres
- dilated pupils are caused by distruction of the 3rd cranial nerve nuclei exiting fibres
- disconjugate eye movements and nystagmus occur whereas vertical eye movements are relatively spared
- upper motor neuron signs develop and patients can become quadriplegic
- flaccidity in the upper limbs and flexor withdrawal responses in the lower limbs often accompany midbrain/pontine damage
- downward herniation of the cerebellar tonsils through foramen magnum causes acute medullary dysfunction and abrupt respiratory and circulatory
collapse; less severe impaction of the tonsils can lead to obstructive hydrocephalus and consequent bihemispheric dysfunction with altered arousal
- upward herniation is initially characterised by coma, reactive miotic pupils, asymetric or caloric eye responses and
decerebrate posturing; caudal-rostral brainstem dysfunction the occurs with midbrain failure and midposition fixed pupils
non-
structural
causes
of coma
differential
diagnosis
general
management
investigations
prognosis
- non structural disorders produce coma by diffusely depressing the function of the brainstem and cerebral arousal mechanisms
- metabolic encephalopathy is often characterised by fluctuations in the patient's level
of arousal and consciousness; motor abnormalities are usually symmetrical if present
hypoglycaemia:
- leads to dysfunction of the cerebral cortex before the brainstem
- acute symptoms of hypoglycaemia are more correlated with the rate at which the blood glucose falls that its absolute level
- the pathophysiology of hypoglycaemic coma is not well understood and a patient in hypoglycaemic coma may survive for up to 90
minutes without suffering irreversible brain damage
hepatic encephalopathy:
- not caused merely by accumulation of ammonia but also involves the accumulation
of neurotoxins such as short and medium chain fatty acids, mercaptans and phenols
- altered neurotransmission may play a role with the accumulation of benzodiazepine like substances, imbalances of
serotonergic and glutaminergic neurotransmitters and the accumulation of false neurotransmitters
uraemic encephalopathy:
- the neurotoxin involved is uncertain and includes urea itself, guanidine, phenols, aromatic hydroxy acids, amines and various peptides
vegetative state
- can be defined as wakefulness without awareness and is the consequence of various diffuse brain insults
- vegetative patients may demonstrate spontaneous eye movements and stereotypical facial and limb movements; however,
they have no evidence of cognitive function or purposeful movement
- vegetative patients generate normal body temperature and usually have normally functioning cardiorespiratory, respiratory and GI systems but are incontinent
- the vegetative state may be a transient phase through which comatose patients pass
as they wake due to cerebral cortex recovering more slowly than the brainstem
- vegetative state should be termed persistent after 1 month and permanent after 3 months after non-traumatic injury and 12 months after traumatic injury
locked in syndrome
- patients who are locked in are voluntarily capable of only vertical eye movements and/or blinking
- the most common cause is pontine infarction due to basilar artery thrombosis but other
causes include pontine haemorrhage, central pontine myelinolysis and brainstem masses
- involves bilateral anterior pontine lesion which transects all descending motor pathways but spares the ascending
sensory and RAS systems
- neuromuscular causes of locked in syndrome are differentiated by the lack of sparing of vertical eye movements
and may be caused by acute inflammatory demyelinating polyradiculoneuropathies, myaesthenia gravis and botulism
akinetic mutism
- describes a rare subacute or chronic state of altered behaviour in which an alert appearing patient is both silent and immobile but not paralysed
- external evidence of cognitive activity is not obtainable
- lesions that cause akinetic mutism include bilateral frontal lobe lesions, hydrocephalus & 3rd ventricular masses
catatonia
- a symptom complex often associated with psychiatric disease
- characterised by stupor or excitement and variable mutism, posturing, rigidity and grimacing
- patients in catatonic stupor do no move spontaneously and appear unresponsive to the
environment despite normal arousal. Passive movement demonstrates waxy flexibility
- choreoform jerks of the extremities and facial grimaces are common
immediate management:
(i) protect the airway
(ii) ensure adequate oxygenation and ventilation
(iii) ensure circulation adequate to maintain cerebral perfusion
NB: throughout the initial resuscitation it is important to gather as much information about the neurological
state as possible as neurological examination is limited by intubation & sedation
seizures:
- repeated generalised seizures damage the brain and should be controlled with
benzodiazepines +/- phenytoin (the latter is ineffective in toxicological seizures)
immediate specific therapies:
(i) glucose should be administered to hypoglycaemic patients
(ii) thiamine should be given prior to or with glucose to prevent Wernicke's
encephalopathy in malnourished thiamine depleted patients
(iii) naloxone 0.4-2mg iv provides effective reversal or opioid induced coma
(iv) flumazenil 1-5mg reverses benzodiazepines (but may produce refractory seizures in benzodiazepine dependent patients)
(v) physostigmine 1-2mg iv reverses the anticholinergic sedative effects of tricyclics
history:
witnessed events - head injury, seizure, details of accident, circumstances under which patient was found
evolution of coma - abrupt or gradual, headache, progressive or recurrent weakness, vertigo, nausea and vomiting,
recent medical history - surgical procedures, infections, medications
past medical history - epilepsy, head injury, drug or alcohol abuse, stroke, hypertension, diabetes, heart disease, cancer, uraemia
previous psychiatric history - depression, suicide attempts, social stressors
access to drugs - sedatives, narcotics, illicit drug
imaging
- CTB is currently the most expedient imaging technique in a comatose patient and gives
the most rapid information about possible structural lesions with the least risk
- CTB has value in demonstration of mass lesions, haemorrhage and hydrocephalus; however, early infarction (less than 12 hours), encephalitis
and isodense subdural haemorrhage may be difficult to visualise and posterior fossa pathology may be somewhat obscured by bone artifact
- MRI can be performed depending on the clinical setting and stability of the patient's condition; however, its use in the urgent setting is limited
by the length of time required for the procedure, the relative inaccessibility of the patient for emergencies that may occur during the procedure
& the limitations of monitoring associated with the modality
- MRI is particularly useful in demonstration of early stroke, encephalitis, central pontine myelinolysis and traumatic shear with greater resolution
and at an earlier time than CT
EEG:
- with metabolic and toxic disorders, the EEG changes generally reflect the degree and severity of altered arousal or delirium
characterised by a decreased frequency of the background rhythm and the appearance of diffuse slow activity in the theta
(4-7Hz) &/or delta (1-3Hz) range
- bilaterally synchronous and symmetrical medium to high voltage broad triphasic waves
are seen in various metabolic encephalopathies most often hepatic coma
- rapid beta activity (greater than 13Hz) in a comatose patient suggests the ingestion of sedative hypnotics
- acute focally destructive lesions show focal slow activity; when lateralised epileptiform discharges appear
in one or both temporal lobes, herpes simplex encephalitis should be strongly considered
- a non reactive, diffuse alpha pattern in a comatose patient usually implies a poor prognosis
and is most often seen after anoxic insults to the brain
- a normally reactive EEG in an unresponsive patient suggests psychiatric disease; however,
a relatively normal EEG is also seen in locked in syndrome and akinetic mutism
- attempts to correlate the pattern and frequency of a post-resuscitative EEG with neurological outcome have been unsatisfactory
- non-convulsive generalised status epilepticus and repeated complex partial seizures may
produce altered levels of awareness or arousal
- continuous EEG monitoring optimises management of status epilepticus and continuous EEG
monitoring in critically ill neurological patients shows a high incidence of unsuspected seizure activity
jugular venous oximetry:
- changes in jugular venous oximetry measure the relationship between cerebral metabolic rate and
cerebral blood flow; there are no data to show it improves outcome
transcranial doppler:
- allows non invasive measurement of blood flow in the basal cerebral arteries and allows early
detection of vasospasm in subarachnoid haemorrhage
evoked potentials:
- evoked potentials are used to follow the level of CNS function in comatose patients
- clinical use of brainstem auditory evoked potential and short latency somatosensory evoked potential
responses stem from the correlation between EP waveform and presumed generators within the CNS
- EPs are less affected than EEG readings by sedative medications and septic or metabolic encephalopathy
- absent bilateral SEPs in patients with hypoxic coma are associated with very poor outcome; however, in
traumatic coma they may be a less definitive prognostic indicator.
icp monitoring:
- a review of published randomised controlled studies of ICP monitoring in acute coma versus no ICP monitoring
looking a mortality and severe disability concluded that there are insufficient data to clarify the role of routine
ICP monitoring in all severe cases of acute coma; however, it is of value in traumatic brain injury
non-traumatic acute coma:
- numerous descriptive scoring systems are used to assess the severity of neurological outcome and the predicted
outcome of patients. A 2 year prospective study of 286 patients with non-traumatic coma demonstrated that the GCS
was as acute as the APACHE-II for this purpose.
- onlly 15% of patients in a medical coma will make a good recovery while 61% will die. Prognosis depends on the aetiology
of medical coma with patients in coma due to stroke, subarachnoid haemorrhage or cardiorespiratory arrest having only a
10% chance of rcovery to independent function; 35% will achieve a moderate to good outcome if coma is due to a metabolic
cause whilealmost all patients who reach hospital after a sedative overdose will recover
- absent pupillary responses at any time and absent vestibulocaloric reflexes after 1 day indicate very poor prognosis
(except in barbiturate or phenytoin poisoning)
- except for sedative drug poisoning, no patient with absent pupillary light reflexes, corneal reflexes, oculocephalic or caloric
responses, or a lack of motor response to noxious stimulation at 3 days after onset is likely to ever regain independent function
- post anoxic convulsive status epilepticus or myoclonic jerks reflect a poor prognosis. Occasional patients will regain
consciousness but remain handicapped but most patients die or become vegetative
traumatic coma:
- outcome of traumatic coma is generally better than that of medical coma
- patients in a coma for longer than 6 hours have a 40% chance to recover to moderate disability or better at 6 months
- the most reliable predictors of outcome at 6 months are:
(i) patient age (worse outcome especially after 60 years)
(ii) depth and duration of coma
(iii) pupil reaction and eye movements (absence at 24 hours predicts death or a vegetative state in 90%)
(iv) motor response in the 1st week of injury
- sustained elevated ICP >20mmHg is an independent predictor of poor prognosis
- subdural haematomas that result in coma have a less than 10% chance of recovery](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-86-320.jpg)


![Community
acquired
pneumonia
- specific
pathogens
pneumococcal
pneumonia
- Antibiotic choice should be guided by microbiological susceptibility data.
- However, unlike in the United States and some regions of Europe and
South-East Asia, penicillin-resistant strains of Streptococcus pneumoniae
(MIC >2 mg/L) are a rare cause of pneumonia in Australia. Furthermore,
S. pneumoniae strains that display intermediate-resistance to penicillin
(MIC 0.125 to <2 mg/L), respond appropriately to routine doses of penicillin.
- For pneumococcal pneumonia due to all strains other than those demonstrated
to be penicillin-resistant, use:
benzylpenicillin 1.2 g (child: 30 mg/kg up to 1.2 g) IV, 6-hourly until significant
improvement,
then amoxycillin 1 g (child: 25 mg/kg up to 1 g) orally, 8-hourly for a total treatment
duration of 7 days.
- For pneumonia due to S. pneumoniae strains that are resistant to penicillin
(MIC >2 mg/L), seek advice from an infectious diseases physician or clinical
microbiologist.
- In patients hypersensitive to penicillin (excluding immediate hypersensitivity, use:
ceftriaxone 1 g (child: 25 mg/kg up to 1 g) IV, daily until significant improvement,
then cefuroxime 500 mg (child: 10 mg/kg up to 500 mg) orally, 12-hourly for a total
treatment duration of 7 days
OR
cefotaxime 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly until significant improvement,
then cefuroxime 500 mg (child: 10 mg/kg up to 500 mg) orally, 12-hourly for a total
treatment duration of 7 days.
- in adult patients with immediate penicillin hypersensitivity, use:
moxifloxacin 400 mg orally or IV, daily for 7 days.
- Alternatively, consider the use of vancomycin
- A number of retrospective observational studies (and one prospective study) have
suggested that improved clinical outcomes may be achieved among critically ill patients
with community-acquired pneumonia (primarily those with pneumococcal bacteraemia)
if initial combination therapy (beta lactam plus macrolide/doxycycline) is used. However,
these findings are yet to be confirmed in randomised prospective studies.
staphlococcal
pneumonia
- Staphylococcal pneumonia may occur as a primary diagnosis, or secondary
to right-sided endocarditis, influenza or aspiration.
- It is commonly severe, especially in children, and may be either community- or
hospital-acquired.
- An initial sputum Gram stain will usually show predominantly Gram-positive cocci
in clusters.
- Recently, there has been an increase in the incidence of severe community-acquired
pneumonia caused by community strains of MRSA, especially among some populations
(eg intravenous drug users, Indigenous and Pacific Island children and adults).
- These strains are genetically different from routine hospital MRSA strains. Sometimes
they are clinically more aggressive (related to the presence of virulence factor Panton-
Valentine leucocidin [PVL]) and may be susceptible to some routine antibiotics such as
clindamycin and trimethoprim+sulfamethoxazole.
- Appropriate susceptibility testing of all Staphylococcus aureus isolates is therefore crucial.
- Antibiotic therapy for these new community MRSA strains should be guided by
microbiological susceptibility data and specialist advice may be necessary.
- In contrast, in many other clinical settings, the presence of S. aureus or MRSA in sputum
culture may simply represent colonisation.
- For non-MRSA staphylococcal pneumonia, use:
dicloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
OR
flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
OR
cephalothin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
OR
cephazolin 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly.
- For patients with immediate penicillin hypersensitivity and severely ill patients with suspected
staphylococcal pneumonia, until antibiotic susceptibility data are available, use:
vancomycin 25 mg/kg up to 1 g (child <12 years: 30 mg/kg up to 1 g) IV, 12-hourly
- For severely ill patients with suspected MRSA staphylococcal pneumonia, vancomycin should
be given together with the beta-lactam regimen above until susceptibility data are known.
- Consultation should be sought on the timing and type of subsequent oral therapy, but generally
7 to 14 days is required for uncomplicated staphylococcal pneumonia.
- Although some recent studies have suggested that linezolid may be more effective than
vancomycin in patients with MRSA pneumonia, each of these studies suffers from significant
methodological flaws. Thus, vancomycin should remain the treatment of choice, except for
pneumonia caused by vancomycin-intermediate strains of S. aureus (VISA or heteroVISA [hVISA])
when linezolid should be used.
Legionella
- Pneumonia due to Legionella species may present with a variety of nonpulmonary symptoms such
as mental confusion, diarrhoea and hyponatraemia, as well as severe respiratory distress.
- Diagnosis can be made by sputum or bronchoalveolar lavage (BAL) culture, serology, urinary antigen
detection or polymerase chain reaction (PCR) of respiratory specimens.
- The new Legionella urinary antigen assay has aided early diagnosis in some cases since it can be
performed easily on routine urine specimens (either before or after commencing antibiotics) and appears
to have acceptable sensitivity. However, this assay detects only Legionella pneumophila type 1 (the
commonest cause of Legionella pneumonia), not other Legionella species.
- For patients with Legionella pneumonia, use:
azithromycin 500 mg IV or orally, daily
OR
doxycycline 100 mg IV or orally, 12-hourly
OR
erythromycin 500 mg to 1 g IV (preferably through a central line), 6-hourly
or erythromycin 500 mg orally, 6-hourly
or erythromycin (ethyl succinate formulation) 800 mg orally, 6-hourly
- PLUS for very severe cases requiring ICU care, consider adding
ciprofloxacin 400 mg IV, 12-hourly
or ciprofloxacin 750 mg orally, 12-hourly
OR
rifampicin 600 mg IV or orally, daily.
- Total (IV + oral) treatment duration for Legionella pneumonia is 7 to 14 days for
immunocompetent patients, but 14 to 21 days for the immunocompromised.
specific
therapy
for other
pathogens](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-89-320.jpg)
![AMI
complications
[created by
Paul Young
09/10/07]
postinfarction
ischaemia
- causes of ischaemia after infarction include:
(i) coronary reocclusion or spasm
(ii) anaemia
(iii) hypotension
(iv) hypermetabolic states
- immediate management includes aspirin, beta blocker,
iv GTN, heparin, consideration of calcium channel blockers
& diagnostic coronary angiography
- post-infarction angina is an indication for revascularisation
- CABG should be considered for patients with left main disease
- if angina cannot be medically controlled or there is haemodynamic
instability consideration should be given to an IABP
ventricular
free wall
rupture
- typically occurs in the first week after infarction
- the classic patient is elderly, female and hypertensive
- free wall rupture presents as a catastrophic event with shock & EMD
- salvage is possible with prompt recognition, pericardiocentesis and repair
- occurs in 1-3% of all patients hospitalised with MI & often occurs very early
ventricular
septal
rupture
- septal rupture manifests as severe heart failure or cardiogenic
shock with a pansystolic murmur and parasternal thrill
- the hallmark finding is left to right intracardiac shunt with an increase
in oxygenation from the RA to the RV although echo is most easy way
to make the diagnosis
- rapid institution of IABP and pharmacological support is required and
operative repair is required for long-term survival
- occurs in 1-2% of cases of MI usually in large infarctions
acute MR
- ischaemic MR is usually associated with inferior AMI &
ischaemia or infarction of the posterior papillary muscle
- papillary muscle rupture typically occurs 2 to 7 days after AMI and presents
dramatically with pulmonary oedema, hypotension and cardiogenic shock
- when a papillary muscle ruptures, the murmur of acute MR may be limited to
early systole because of the rapid equalisation of pressures in the left atrium
& left ventricle [the murmur may be inaudible if cardiac output is low]
- management includes afterload reduction including IABP +/- inotropes
- definitive therapy is surgical repair or valve replacement which should be
undertaken as soon as possible
right
ventricular
infarction
- right ventricular infarction occurs in up to 30% of patients with inferior infarction
- clear CXR with distended jugular veins in an inferior AMI suggests RV infarction
- ST elevation in V3R to V5R and characteristic haemodynamic findings on right
heart catheterisation (elevated right atrial and RV EDP with normal to low PAoP
& low cardiac output) confirm the diagnosis
- right ventricular preload should be maintained with iv fluids; overfilling can lead to
overdilation of the right ventricle and compromised left ventricular filling
- inotropes may be required
- maintainance of AV synchrony is important for optimisation or RV filling
- IABP may be useful particularly when RV pressures are elevated
- reperfusion is critical
arrhythmias
- rhythm disturbance is common following acute myocardial infarction
& is most likely within the first few hours of onset and during reperfusion
- risk of arrhythmia is decreased by correcting hypoxaemia, hypovolaemia
& acid base disturbance; K+ & Mg should be maintained (risk of VT declines
as potassium increases until it is greater than 4.5mmol/L. there is no evidence
that Mg levels have any effect on ventricular arrhythmia in this setting; however,
ILCOR recommends Mg>1.0mmol/L
cardiogenic
shock
epidemiology & pathophysiology:
- leading cause of in-hospital death after myocardial infarction
- has a mortality rate of approximately 50%
initial management:
- maintenance of oxygenation and ventilation are critical
- patients may require intubation [which entails a high risk of arrest]
- arrhythmia should be promptly treated as they may be poorly tolerated
- if the patient is hypotensive fluids should be administered
unless there is frank pulmonary oedema
- inotropes +/- vasopressors may be required if the blood pressure is inadequate
reperfusion therapy:
- RCTs have not demonstrated a mortality benefit for thrombolytics
in the presence of cardiogenic shock
- emergency revascularisation is the only intervention that has been shown to
reduce mortality [GUSTO-1 trial showed that emergency revascularisation within
24 hours of shock leads to better outcomes; SHOCK showed that early intervention
leads to better outcomes at 6 months than initial medical stabilisation followed by later
intervention]
- the presence of cardiogenic shock is a class I
indication for emergency revascularisation
- prophylactic lignocaine tends to increase mortality
and is thus reserved for the treatment of VT & VF.
- prophylactic iv magnesium (<4hr) was of benefit in the LIMIT II study but
not in the ISIS-4 trial and is not recommended
cardiac
failure
- with large MI there is progressive thinning of the affected myocardium, with stretching
& dilatation of the ventricle & sometimes aneurysm formation. ACE inhibitors appear to
limit dilatation, preserve LV function and improve prognosis. Benefits are maximal in those
with poor LV function
- RV failure secondary to RV infarction is often responsive to volume loading (guided by clinical
response, echocardiography or PCWP titrated to optimal LV filling eg 16-18mmHg)
- diuretic therapy, afterload reduction & unrecognised hypovolaemia may aggravate hypotension
in these patients
- reinfarction in the 10 days following MI occurs in 5-10% of patients
thromboembolism
- embolic stroke occurs in 1-3% of patients (mostly following extensive AMI)
- 30-40% of anterior Q wave MIs may be complicated by mural thrombus
- embolism is uncommon following inferior infarction
- patients with large anterior AMI and extensive anterior RWMIs or with
proven mural thrombus are usually put on anticoagulation for 3 months
Post-MI
syndrome
(Dressler's)
& pericarditis
- pericarditis is a common early complication of extensive infarction
- pericardial friction rub may be heard in 10-15% of patients with anterior infarction
- occurs 24-72 hours after infarction & may mimic ischaemia
- Dressler's syndrome is now uncommon but is thought to be an immunopathic
response to myocardial necrosis. It is characterised by fever, elevated ESR, a
pericardial friction rub &arthralgia & may occur some weeks after MI.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-90-320.jpg)
![conduction
disturbances
[created by
Paul Young
13/10/07]
normal
cardiac
conduction
- the electrical impulse leading to cardiac contraction is generated by
specialised groups of cells with the ability to depolarise spontaneously
- the SA node is located in the posterior & superior portion of
right atrium & its depolarisation is not visible on an ECG
- the p wave is generated by spread of the electrical impulse
through the atria
- the impulse reaches the AV node approximately half way through the
p wave with with remainder of the p wave due to left atrial depolarisation
- in the normal heart the atria and ventricles are electrically isolated
except at the AV node which is located in the atrial septum
- conduction through the AV node accounts for the majority of the PR interval
- from the AV node the the impulse travels through the bundle of His and from
there travels down the right and left bundle branches and their fasicles to the
Purkinje network which causes ventricular contraction
causes of
conduction
failure
- narrow QRS complexes suggest supranodal site of block
- wide QRS complexes suggest and infranodal site of block
- AV nodal blocks are usually reversible except where infarction
permanently damages a portion of the conduction pathway
- Causes of AV blocks include:
(i) drugs:
- digoxin
- beta blockers
- calcium channel blocks
(ii) primary cardiac disease
- ischaemic heart disease
- fibrosis of the conduction system
- congenital heart disease
- calcific valvular heart disease
- cardiomyopathy
(iii) metabolic
- hyperkalaemia
- hypermagnesaemia
(iv) infiltrative disease
(v) infectious / inflammatory disease
(vi) collagen vascular disease
(vii) Addisons disease
(viii) radiation
(ix) neurally mediated conditions
- carotid sinus syndrome
- vasovagal syncope
- neuromyopathic disorders
- infranodal blocks are usually caused by structural heart disease &
anatomical disruptions of the conduction system
- rare causes of infranodal block include disruption of the Bundle of
His from aortic valve calcification & Chagas disease
clinical
presentation
- syncope and presyncope are the most dramatic symptoms of conduction
disturbances; palpitations, dyspnoea, angina & fatigue are also seen
- a significant number of patients develop bradydysarrhythmias after an AMI
sinus
node
abnormalities
sinus bradycardia:
- can be divided into appropriate and inappropriate pathological bradycardia
- pathological bradycardia does not increase appropriately with exercise
- medications are the most common cause of inappropriate sinus bradycardia;
other causes include autonomic influences, electrolyte abnormalities, increased
vagal tone (eg due to ischaemia) and intrinsic structural disorders
sinus arrest:
- sinus arrest occurs when the pacemaker cells in the SA node fail to depolarise
- pauses of less than 3 seconds may be normal; however, pauses of longer than
3 seconds are usually pathological and should be evaluated
carotid sinus hypersensitivity:
- diagnosed when ventricular asystole greater than 3 seconds of a drop in
systolic BP >50mmHg occurs in response to carotid sinus massage
- treatment is permanent pacing in symptomatic individuals
post-surgical bradydysrhythmia:
- bradyarrhythmias are common after cardiac surgery
- valve surgery and septal myectomy can cause significant damage to the conduction
system; prolonged ischaemia during heart transplant can also cause sinus node or
conduction system damage
- medication and reversible ischaemia are often implicated therefore the decision
to place a permanent pacemaker should defered until 5-7 days post-operatively
- permanent pacing is required in 2% of patients after valve surgery &
approximately 10% of heart transplant recipients
AV node
dysfunction
1st degree AV block:
- characterised by a PR interval of greater than 0.2s in adults and 0.18s in children
- potential causes of 1st degree AVB include:
(i) delayed conduction through the atria from the SA to the AV node
- typically due to structural causes such as right atrial enlargement or ASD
(ii) delay in AV nodal conduction
- most common cause of 1st degree AVB
(iii) prolonged infranodal conduction
- typically associated with a wide QRS due to disease in the fascicles or bundle of His
- typically benign and seen in 0.5% of young adults without heart disease; in older patients
is most commonly due to idiopathic degenerative disease
2nd degree block type I:
- Mobitz type I or Wenkebach rhythm is defined by progressive PR interval
prolongation followed by a dropped beat
- caused by a block in AV conduction
- a stable rhythm
- if due to a medication it will resolve on discontinuation of the medication
2nd degree block type II:
- 2nd degree block type II (or Mobitz type II) is characterised by a sudden non-conducted beat
- this is an inherently unstable & may be associated with serious pathology
- almost always due to infranodal conduction disturbance
- is described as a high degree AV block with P to QRS
ratios of 3:1 to 4:1 & can progress to complete heart block
2:1 AVB
- can be caused by Mobitz type I (usually narrow QRS) or Mobitz type II (usually wide QRS)
3rd degree AVB:
- characterised by complete AV dissociation
- ventricular complexes may be junctional (narrow QRS complex at 40-60)
or ventricular (wide QRS at <40)
- congenital 3rd degree AVB is more common in females and often has an
escape rhythm with an adequate rate
- acquired 3rd degree AVB usually requires permanent pacing and occurs most often in males.
Specific causes include medication, ischaemia, progression from Mobitz type II rhythm and infarction.
Third degree heart block complicating inferior MI is usually temporary and can be treated with
temporary pacing whereaswhen it complicates anterior infarction it usually requires a permanent
pacemaker
Therapy
- medical therapy for AV block consists of atropine & adrenergic agents
- atropine decreases vagal tone & is useful in inferior myocardial infarction
than anterior mocardial infarction (because it is not helpful for AV node ischaemia)
- atropine will not improve 3rd degree heart block or Mobitz type II block if the
pathology is below the AV node & it is not effective in heart transplant patients
- digibind should be used in symptomatic patients with digoxin-induced AV block.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-91-320.jpg)
![primary
aldosteronism
[created by
Paul Young
05/12/07]
subtypes
initial
investigation
approach
to primary
aldosteronism
general
- primary aldosteronism is recognized to be the most common form of secondary
hypertension. Using the plasma aldosterone to plasma renin activity ratio as a case-
finding test, followed by aldosterone suppression confirmatory testing, has resulted in
much higher prevalence estimates of 5-13% of all patients with hypertension.
treatment
general
- Unilateral adrenalectomy in patients with APA or unilateral adrenal hyperplasia results
in normalization of hypokalaemia in all these patients; hypertension is improved in all
and is cured in approximately 30-60% of them.
- In bilateral adrenal forms of primary aldosteronism, unilateral or bilateral
adrenalectomy seldom corrects the hypertension and they should be treated medically
with a mineralocorticoid receptor antagonist.
features
- Patients with marked hypokalaemia may have muscle weakness and cramping,
headaches, palpitations, polydipsia, polyuria, nocturia, or a combination of these. The
polyuria and nocturia are a result of hypokalaemia-induced renal concentrating defect and
the presentation is frequently mistaken for prostatism in men.
- The degree of hypertension is usually moderate to severe and may be resistant to usual
pharmacological treatments.
- Hypokalaemia is frequently absent; thus, all patients with hypertension are candidates
for this disorder
- Because of a reset osmostat, the serum sodium concentration tends to be high-normal or
slightly above the upper limit of normal. This clinical clue is very useful when initially
assessing the potential for primary aldosteronism.
- Mineralocorticoid receptor antagonists (e.g. spironolactone and eplerenone) and
high-dose amiloride are the only medications that absolutely interfere with interpretation
of the ratio and should be discontinued at least 6 weeks before testing.
- Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor antagonists
(ARB) and diuretics have the potential to 'falsely elevate' PRA. Therefore, in a patient
treated with an ACE inhibitor, ARB or diuretic the finding of a detectable PRA level or a
low PAC:PRA ratio does not exclude the diagnosis of primary aldosteronism. However, a
very useful clinical point is that when a PRA level is undetectably low in a patient taking
an ACE inhibitor, ARB or a diuretic, primary aldosteronism should be highly suspect.
- Adrenergic inhibitors (e.g. beta-adrenergic blockers and central alpha-2 agonists) suppress
renin secretion, but also in turn suppress aldosterone secretion (although to a lesser degree
than renin) in normal individuals; thus, although the PAC/PRA may rise in hypertensive
patients without primary aldosteronism treated with adrenergic inhibitors, the PAC remains
less than 416 pmol/l (15 ng/dl) and the case finding test is not significantly affected.
confirmatory
testing
- It is impossible to interpret data obtained from patients receiving treatment with
mineralocorticoid receptor antagonists (e.g. spironolactone, eplerenone) or high-dose
amiloride when PRA is not suppressed. Therefore, treatment with a mineralocorticoid
receptor antagonist should not be initiated until the evaluation has been completed and
the final decisions about treatment have been made
- Aldosterone suppression testing can be performed with orally administered sodium
chloride and measurement of urinary aldosterone or with intravenous sodium chloride
loading and measurement of PAC.
surgical treatment
- Unilateral laparoscopic adrenalectomy is an excellent treatment option for patients with
APA or unilateral hyperplasia. Although blood pressure control improves in nearly
100% of patients postoperatively, average long-term cure rates of hypertension after
unilateral adrenalectomy for APA range from 30% to 72%.
Pharmacological treatment
(i) General
- IHA and GRA should be treated medically. In addition, APA patients may be treated
medically if the medical treatment includes mineralocorticoid receptor blockade.
- No placebo controlled randomized trials have evaluated the relative efficacy of drugs in
the treatment of primary aldosteronism.
(ii) Spironolactone
- Spironolactone has been the drug of choice to treat primary aldosteronism for more than
three decades. The dosage is 12.5-25 mg per day initially and is increased to 400 mg
per day if necessary to achieve normokalaemia without the aid of oral potassium chloride
supplementation. Hypokalaemia responds promptly, but hypertension may take as long as
4-8 weeks to be corrected. After several months of therapy, this dosage often can be
decreased to as little as 25-50 mg per day
(iii) Eplerenone
- Eplerenone is a steroid-based antimineralocorticoid that acts as a competitive and selective
aldosterone receptor antagonist and was approved by the FDA for the treatment
of uncomplicated essential hypertension in late 2003. The 9,11-epoxide group in
eplerenone results in a marked reduction of the molecule's progestational and anti-
androgenic actions compared with spironolactone
- Treatment trials comparing the efficacy of eplerenone vs. spironolactone for the
treatment of primary aldosteronism have not been published.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-92-320.jpg)
![Contrast-induced
nephropathy
[created by
Paul Young
02/10/07]
general
risk
factors
strategies
for prevention
defined as increase of 44umol/L from
baseline or 25% rise in creatinine after
exposure to contrast
Nash et al found it to be 3rd most common
cause of renal failure in hospitalised patients
1. pre-existing renal disease
- risk only 8% if less than 135 umol/L
in one study and none had a rise of
greater than 89umol/L
2. diabetes mellitus
3. age >75 years
4. periprocedural volume depletion
5. heart failure
6. nephrosis
7. cirrhosis
8. hypertension
9. proteinuria
10. NSAIDS and other nephrotoxins
11. high doses of contrast
Mehran et al have devised a score
which can be used to predict the risk
of an acute decline in kidney function
after percutaneous coronary intervention
1. fluid administration
- generally recommended to give prehydration
- optimal duration and type of fluid not well defined
- several small trials exist comparing iv saline with
oral fluid, shorter regimens and 0.45% saline
- iv 0.9% saline a 1ml/kg/hr for 24 hours beginning
2-12 hours before administration of contrast medium
if GFR is less than 50, particularly if there are risk factors then
consideration should be given to alternative imaging approaches
2. contrast medium
- metanalysis of several RCTs show that low osmolality
contrast media are lower risk
- use lowest dose possible to complete the procedure
3. N-acetylcysteine
- most commonly given 600mg orally every 12 hours for 4
doses beginning before administration of contrast medium
- multiple RCTs and meta-analyses performed
with inconsistent trial results for unknown reasons
- may decrease release of creatinine from skeletal
muscle than effecting renal function directly
4. intravenous sodium bicarbonate
- proposed that alkalinisation of renal tubular
fluid might be beneficial by reducing the levels
of pH-dependent free radicals
- dose in trial 154mEq HCO3 at 3ml/kg/hr before
contrast & then 1ml/kg/hr for 6 hours afterwards
- one trial which showed benefit from bicarb; however,
study was terminated early despite the fact the timing
of interim analysis and the stopping values were not
prespecified and the p value for the difference in event
rates (P=0.02) was higher than is standard for stopping
a trial early
6. other approaches
(i) diuretics
- lead to similar or higher rates of nephropathy
(ii) various vasodilators
- dopamine, fenoldopam, atrial natriuretic peptides, calcium
blockers, PGE2 & a non-specific endothelin receptor antagonist
are not beneficial
(iii) captopril
- small trial showed a benefit from captopril but confirmation is needed
(iv) ascorbic acid
- one trial showed apparent benefit from this; however,
baseline renal function was worse in placebo group
(v) theophylline and aminophylline
- metanalysis shows lower risk but
significant heterogeneity between studies
(vi) haemodialysis or haemofiltration
- appears to reduce mortality when used prophylactically; however,
results need confirmation and intervention is very labour intensive
5. cease nephrotoxins prior
- NB: metformin should be ceased because of
risk of lactic acidosis if nephrotoxicity develops
pathogenesis](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-93-320.jpg)

![corticosteroids
in sepsis
[created by
Paul Young
02/10/07]
cellular
mechanisms
of action
(genomic)
- Cells from most tissues are responsive to corticosteroids,
which freely cross cell membranes.
- Binding of corticosteroids to the glucocorticoids receptor induces the
release of chaperone proteins and the dimerization of the complex,
which then, enters into the nucleus and interacts with specific
binding sequences, the glucocorticoid responsive element
- The glucocorticoids receptor forms an inactive intracytosolic
complex with chaperone proteins like heat shock protein (HSP) 40,
HSP56, HSP70, and HSP90, immunophillins, P23, and other
unknown proteins
- Subsequent transcription of genes (e.g.most cytokines, adhesion
molecules, lipoxygenase, etc.) initiated by various transcriptional factors
such as AP1, NF-AT and NF-kB are prevented.
- Glucocorticoids receptor dimers induce the inhibitor of NFkB (IkB).
- In contrast, other GRE sites upregulate the transcription of numerous
other genes (e.g. lipocortin-1, thymosin-b4 sulfoxide)
cellular
mechanisms
of action
(non-genomic)
- there are membrane binding sites for different
corticosteroids in many tissues, including liver
plasma membranes and neuronal synaptic membranes
- physicochemical interactions occur in-between the cell’s
membrane and corticosteroids inducing very rapid (within
seconds), nonspecific, nongenomic effects
- neural modulation by corticosteroids may explain the rapid
restoration of sympathetic modulation on heart and vessels,
and may account for the hydrocortisone induced rapid pressure
sensitization to exogenous catecholamine in septic shock
corticosteroids
in immune
modulation
- by interacting with NF-IL6, corticosteroids enhance the synthesis
of the acute phase reactants; with AP-1 and NF-kB, they inhibit
the synthesis of various proinflammatory factors.
- corticosteroids prevent the migration of inflammatory cells from
circulation to tissues by blocking the synthesis of various chemokines
- prevent the synthesis of almost all proinflammatory cytokines including
several interleukins (IL-1, IL-2, IL-3, IL-6), interferon-g (IFN-g), granulocyte
macrophage colony stimulating factor, and tumor necrosis factor-a (TNF-a).
- They also enhance the production of the
macrophage migration inhibitory factor (MIF)
- by stimulating the synthesis of lipocortin-1, corticosteroids inhibit the
synthesis of soluble phospholipase A2 (PLA2) and the subsequent
arachidonic acid cascade, reducing the production of leukotrienes
- inhibit the synthesis of inducible cyclooxygenase-2 (COX2)
and of inducible but not constitutive nitric oxide synthase
corticosteroids
in cardiovascular
modulation
- chronic corticosteroid excess induces hypertension,
whereas adrenal insufficiency induces hypotension
- Animal studies have demonstrated that both glucocorticoids and
mineralocorticoids enhance the vasoconstrictor response to epinephrine
- underlying mechanisms remained unclear, and may involve multiple
pathways like iNOS and COX-2 inhibitions or the stimulation of the
phosphoinositide system
- In septic shock, adrenal insufficiency was associated with a marked
hyporesponsiveness to norepinephrine, which was fully reversed 1 h
after 50 mg of intravenous hydrocortisone
diagnosis
of steroid
insufficiency
in sepsis
- Annane et al (2006) have demonstrated that both free and total cortisol response can be
used to determine whether adrenal insufficiency is present in septic shock by comparing
with a metyrapone stimulation test as a gold standard:](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-95-320.jpg)
![CRP
[created by
Paul Young
02/10/07]
General
- A major and common question in clinical practice in the ICU is to differentiate
between noninfectious systemic inflammation (such as SIRS) and sepsis.
- Most of these potential laboratory markers are elements (and mediators) of the host
inflammatory response to infection
- The most frequently reported as potential markers include C-reactive protein (CRP),
procalcitonin (PCT), interleukin (IL)-6, IL-8, and other cytokines, as well as diverse
immunologic and endothelial molecules.
Normal
range
- Acute phase responses come from changes in liver gene
expression occurring after an inflammatory stimulus (injury,
trauma, infection).
- CRP is a positive APP whose plasma concentration increases rapidly,
up to 1000-fold from around 1mg/mL, during inflammatory disorders.
The median plasma concentration of CRP measured in healthy young
adults is 0.8 mg/L.
- The 90th and 99th percentiles reported from these studied samples
were 3 mg/L and 10 mg/L, respectively.
- Plasma CRP concentrations are determined only by the synthesis
rate of CRP, and this rate increases markedly depending on the
intensity of inflammatory stimuli.
- When the stimulus is no longer present, CRP levels quickly fall.
- The plasma half-life of CRP appears to be around 19 hours.
- CRP expression and its induction in the hepatocyte is mainly regulated
transcriptionally by IL-6 through activation of several transcription factors
function
of CRP
- The biologic functions of CRP are protective:
(i) it exhibits both proinflammatory and anti-inflammatory activities.
(ii) CRP has several calcium-dependent binding properties and
biologic functions, related to nonspecific innate immune response
causes of
elevated CRP
- CRP was discovered in 1930 by studying patients with
Streptococcus pneumoniae infection, and it was so named for
its ability to bind to the somatic C-polysaccharide of such bacteria.
- Belongs to the family of pentraxins, which are calcium-dependent
ligand-binding plasma proteins.
- bacterial and fungal infections are potent inflammatory stimuli that induce
a major acute phase response producing markedly elevated CRP levels
- some autoimmune diseases (arthritis and vasculitides), organ tissue necrosis,
intense trauma, surgery, and various neoplasias, may also significantly increase
the circulating levels of CRP.
- minor acute phase responses with slightly elevated CRP levels may also
occur in association with low-grade inflammatory states.
- CRP levels are associated with prognosis in acute myocardial infarction and
in acute coronary syndromes.
- Recently, it has been demonstrated that there is an association between minor
elevated plasma concentrations and the risk of developing cardiovascular disease
that may represent a subclinical state of low-grade chronic inflammation, which may
reflect vascular inflammation. It seems that CRP is not only an inflammatory marker
and predictor of cardiovascular disease, but also a mediator of disease because it is
involved in the pathogenesis of atherosclerosis and atherogenesis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-96-320.jpg)




![central venous
catheterisation
techniques
[created by
Paul Young
02/10/07]
subclavian
internal jugular
femoral
PICC lines
indications
complications
1. vascular access
2. central venous monitoring
3. administration of drugs or TPN
4. renal replacement therapy
1. immediate
- pneumothorax
- failure to locate vein
- accidental arterial puncture
- haemothorax
- haematoma
- arrhythmia
- thoracic duct injury
2. early
- haemopericardium and tamponade
- pneumothorax
- catheter blockage
- chylothorax
- catheter knots
3. late
- infection
- catheter fracture
- vascular erosion
- thrombosus
- osteomyelitis of the clavicle
contraindications
1. coagulopathy
- use femoral approach
2. respiratory failure
- use femoral approach
3. raised ICP
- use femoral approach
general
technique
- use seldinger technique
- consider ultrasound visualisation of central vein
- if using a neck approach then prep neck so that
all approaches can be used; head down at least 15 degrees
relevant
anatomy
1. internal jugular
course:
- runs from its origin at the jugular foramen in the skull where it
continues the sigmoid sinus, to its termination behind the sternal
extremity of the clavicle where it joins the subclavian vein to form
the brachiocephalic vein
- lies lateral first to the internal and then to the common carotid artery
within the carotid sheath
- in its upper part it lies quite superficially in the anterior triangle of the
neck, superficial to the external carotid artery and then it descends
deep to sternomastoid
relationships:
- anterolaterally: skin, superficial fascia, platysma, investing layer of
cervical fascia, sternomastoid, sternohyoid & omohyoid. Ansa cervicalis
crosses the vein. Higher up it is crossed by the accessory nerve
- posteriorly: transverse process of the cervical vertebrae, levator scapulae,
scalenus medius and anterior, cervical plexus, phrenic nerve, thyrocervical
trunk, vertebral vein, 1st part of subclavian artery
- medially: internal carotid artery and 9th to 12th cranial nerve above and
common carotid and vagus nerve
tributaries:
(i) inferior petrosal sinus
(ii) facial vein
(iii) pharyngeal vein
(iv) lingual vein
(v) superior thyroid vein
(vi) middle thyroid vein
(vii) occipital vein
3. femoral vein
- boundaries of femoral triangle are adductor longus and sartorius
- structures are NAVEL (from lateral to medial)
approaches:
1. supraclavicular
2. infraclavicular
approaches:
1. central
- needle puncture is 1cm below apex of triangle
formed by head of scm and clavicle aiming 60
degrees to skin towards ipsilateral nipple in a plane
parallel to the medial border of the lateral head of
the scm
- blood should be obtained within 3cm
2. lateral or posterior approach
- turn head away from selected side and insert
needle at the posterior margin and deep to the scm
2-3 finger breadths above clavicle and directed towards
the jugular notch
- blood should be aspirated within 4-5cm
3. anterior approach
- identify the carotid and insert the needle in the midpart
of the medial border of scm aiming towards the ipsilateral
nipple
- turn hip neutral to slight external rotation
- order of structures lateral to medial is NAVL
- boundaries of femoral triangle are adductor longus and sartorius
2. subclavian vein:
relationships:
- superior: the vein is most cephalad at the midpoint of the clavicle. Overlying
the vein is firstly the clavicle and the medially fascia and skin.
- lateral: lies anterinferiorly to the subclavian artery as it crosses the first rib,
scalenus anterior separates the vein from the artery
- posterior: the subclavian vein crosses in front of the phrenic nerve and Sibsons
fascia overlying the pleura
- anterior: the external jugular vein joins the subclavian vein after passing through
the deep fascia above the clavicle](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-101-320.jpg)



![DVT
[created by
Paul Young
02/10/07]
epidemiology
- deep-vein thrombosis (DVT) has an estimated annual
incidence of 67 per 100 000 among the general populations
- despite adequate therapy, 1% to 8% of patients in whom
pulmonary embolism develops will die
- others will experience long-term complications such as:
(i) postphlebitic syndrome (40%)
(ii) chronic thromboembolic pulmonary hypertension (4%)
- Among patients who died while in the ICU, PE has been reported
in 7 to 27% (mean, 13%) of postmortem examinations, and PE was
thought to have caused or contributed to death in 0 to 12% (mean, 3%).
- A clinical suspicion of PE was present in only 30% of these before death.
- among four prospective studies the DVT rates varied between
13% and 31% in critically ill patients who did not receive prophylaxis.
Although the clinical consequences of asymptomatic DVT detected
by routine screening are uncertain, a recent study showed that patients
documented to have DVT by Doppler ultrasound had a significantly
greater frequency of subsequent PE during their hospitalization
(11.5% vs 0%, p < 0.01). Furthermore, even small PE may be poorly
tolerated by critically ill patients, many of whom have reduced cardio-
respiratory reserve.
DVT
prophylaxis
in critical
illness One study compared strategies to improve thromboprophylaxis
use among 1,827 patients in three similar critical care units.
Strategies to improve compliance with DVT prophylaxis:
- Appropriate thromboprophylaxis was used in 38% of patients in
the ICU in which no special compliance intervention was used, in
62% of patients in the unit in which education about DVT prophylaxis
was provided to physicians, and in 97% of the patients in the third ICU
in which prophylaxis education was combined with mandatory computer
order entry (p < 0.01 for all comparisons).
suggested
approach
risk
factors
- The vast majority of patients admitted to a critical care unit have
a major risk factor for VTE, and most have multiple risk factors.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-105-320.jpg)

![diabetes
insipidus
[created
by Paul
Young
30/11/07]
general
physiology
- diabetes insipidus is a syndrome characterised by polyuria,
excessive thirst & polydipsia
central DI
- central or neurogenic DI results from an inappropriately low amount
of ADH being released in response to an osmotic stimulus
- persistent severe central DI occurs rarely, as does DI which is
precipitated by excessive intake of water caused by abnormalities
of thirst or psychogenic function (dipsogenic or psychogenic DI)
- transient, usually incomplete, central DI is common severe head injury
nephrogenic DI
- caused by deficient action of ADH
- occurs very uncommonly in its classical form
- may be recognised as a less severe form acquired in patients on lithium
therapy
(i) factors increasing ADH secretion:
- hyperosmolality
- hypotension
- stress, emotional stimuli
- pain, surgery, trauma
- exercise
- positive pressure ventilation
- cholinergic and beta adrenergic drugs
- nicotine, angiotensin II, barbiturates
(ii) ADH action is potentiated by:
- carbamazepine
- clofibrate
- thiazide diuretics
- prostaglandin synthetase inhibitors
(iii) ADH secretion is inhibited by:
- central DI
- opioid antagonists
(iv) ADH action is antagonised by:
- hypokalaemia
- hypercalcaemia
- prostaglandin E2
- lithium, amphotericin B
- excess vasopressinase
actions of ADH:
(i) antidiuresis
- results from ADH action on V2 receptors in the distal renal tubule, mainly
in the collecting duct. V2 agonist action stimulates cAMP leading to activation
of microtubule passages for water ingress
(ii) vasoconstriction
- vasoconstriction results from V1a receptor stimulation which occurs when higher
concentrations of ADH exist. This is clinically significant in hypotensive states,
where high concentrations of ADH contribute to the maintenance of blood pressure
(iii) coagulation
- coagulation effects are extrarenal V2 receptor mediated
- prostacyclin generation is stimulated; tPA, factor VIII coagulant activity and von
Willebrand's factor all increase
- ADH & its analogues, in pharmacological doses, induce coagulant activity in healthy
patients & in disease states and after cardiac surgery
central
DI
nephrogenic
DI
aetiology:
- causes of persistent central DI invariably involves destruction of the hypothalamus
or pituitary gland & sometimes produce defects in thirst mechanisms
- complete central DI may follow severe head injury & rarely even minor head trauma
- incomplete central DI occurs quite commonly with severe head injuries & particularly with brain death
- pituitary apoplexy continues to be described after hypovolaemia & septic shock
- transient DI has been described with thoracic trauma & CABG
- some causes (lithium & sarcoidosis) may have variable components of central &
nephrogenic DI and thirst disorder
pathophysiology:
- the syndrome of DI results from a failure of appropriate ADH secretion or action,
in response to the physiological stimulus of water deficiency which is characterised
by relative plasma hyperosmolality
- if ADH deficiency is complete, over 20L/day of very dilute urine may be passed
- frequently ADH deficiency is relative with a reduction in the slope & sensitivity of the
ADH response to a change in plasma tonicity, resulting in lesser amounts of hypotonic
urine (3-6L/day)
- central DI is less severe in the presence of simultaneous failure of the anterior pituitary
due to a lower cortisol level resulting in a lower metabolic rate, renal solute load, GFR &
inhibition of free water excretion
presentation:
- usual clinical manifestations are sudden onset of polyuria with resultant
thirst and polydipsia (in patients who are able to drink). In patients who
are unable to drink hypernatraemia and volume depletion develop
- urine volumes >4-6L/day or 3ml/kg/hr for 4-6 consecutive hours in
neurosurgical patients suggests DI
- in severe forms urine is very hypotonic (50-200mosm/kg) but in incomplete
forms, particularly if hypovolaemia is present, urine osmolality may well rise
well above plasma osmolality. [the essential feature is that urine osmolality
is low compared to plasma osmolality]
- following neurosurgery on the hypothalamus and pituitary, four patterns of urine output have
been observed:
(i) temporary polyuira lasting several days
(ii) transient polyuria followed by a period of normal urine output followed by permanent DI
(iii) an immediate and permanent polyuria
(iv) a variation of the triphasic pattern in which there is decreased urine output in the interphase
investigation:
- subjects with DI have higher plasma osmolalities but there is considerable overlap
with the normal range and this determination is not diagnostic in individuals; urine
osmolality is low (often 50-100mosm/kg) but the degree varies inversely with the
severity of the polyuria
- solute diuresis (rather than DI) is suspected if the urine osmolality is between 250
& 320mosm/kg and particularly if there is an increased osmolar gap
- further testing include dehydration tests, DDAVP tests and ADH assays
- in practice DDAVP is administered 1-2mcg/kg sc 12hrly and response is observed
general management:
- management problems in the ICU are usually focussed on the polyuria & hypovolaemia with
associated hyperosmolality
- rapid return to normal plasma osmolality is not always the major objective, particularly where an
increase in cerebral volume is undesirable
- provided there is cardiovascular stability, mild polyuria (eg 3ml/kg/hr) is often best observed with
frequent determinations of plasma and urine osmolality, unless hyperosmolaemia develops
- if polyuria is persistent or severe (eg>7ml/kg for >4-6hrs) drug therapy should be considered
- the priority is almost always restoration of circulatory stability rather than reversal of hyperosmolality
- if parasellar pathology is the suspected as the cause then anterior pituitary deficiency with steroid
deficiency may coexist
differential
diagnosis
of polyuria
normal relationship between plasma and urine osmolality
plasma osmolality urine osmolality
>288 >125
>290 >200
>292 >400
>294 >600
1. excess water load
(i) exogenous - iatrogenic, thirst disorders, hypothalamic disease, psychogenic polydipsia
drugs (eg chlorpromazine, anticholinergics)
(ii) endogenous - recovery from unrecognised overload
2. solute (osmotic) diuresis
(i) exogenous or endogenous solute load - glucose, urea, mannitol, iv contrast, sodium choride
(ii) abnormal solute handling - chronic renal disease, diuretics
3. renal tubular unresponsiveness of ADH
(i) nephrogenic DI - congenital & familial
(ii) acquired nephrogenic DI - drug induced (lithium, clozapine, rifampicin, gentamycin), chronic
electrolyte disturbance (hypercalcaemia), renal disease, post ATN,
post renal transplant, amyloid, multiple myeloma, sickle cell disease,
pregnancy
4. central DI
(i) neoplastic, infective or infiltrative lesions of the hypothalamus or pituitary
(ii) pituitary or hypothalamic surgery or ablative radiotherapy
(iii) head injury
(iv) vascular lesions (post partum necrosis, haemorrhage or hyperviscosity
(v) congenital (usually autosomal dominant)
specific therapy:
(i) vasopressin
- may be given by continuous infusion & is effective in reversing polyuria
- doses of 0.04U-0.1U per hour may be used
(ii) DDAVP (desmopressin)
- 1 to 2 mcg iv (larger doses are often required in early central DI) or 10-40mcg intranasally
- duration of action is 12-24hrs when given intranasally due to slow absorption
(iii) non-hormonal management
- these agents either increase renal sensitivity to ADH or potentiate ADH release & are
only considered in partial central DI (eg thiazides, chlorpropamide, carbamazepine)
congenital nephrogenic DI
- include congenital X-linked form (90%) & a less common autosomal form which
may be either recessive or dominant
- hypercalcaemia, hypokalaemia & drugs that antagonise ADH will worsen the
disorder & should be avoided
acquired nephrogenic DI
- occurs commonly in association with various drugs
- drug induced DI is always the nephrogenic type
- nephrogenic DI occurs in 10% of patients on long-term lithium even if it is in the therapeutic range
transient DI of pregnancy
- a vasopressin resistant DI of pregnancy is recognised
- this transient condition is caused by excessive placental generated vasopressinase
- there is a brisk response to DDAVP which is not metabolised by vasopressinase
- associated acute fatty liver and liver failure ahve been described](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-107-320.jpg)

![use of
CRP &
procalcitonin
[created by
Paul Young
02/10/07]
general
- CRP and PCT are the most common biomarkers to distinguish between
sepsis and noninfectious SIRS at the moment although they show suboptimal
diagnostic performance.
- Seemingly, the PCT test has shown marginally better overall diagnostic accuracy
than the several varieties of CRP test, especially in some clinical conditions.
- PCT assays are more costly, slower, and less accessible than those of CRP.
- Generally, research demonstrates that PCT is a better indicator of illness severity than CRP.
- Considering CRP kinetics, serial determinations of CRP can be useful for monitoring
inflammatory activity, the onset of infections, and patient responses to therapy.
- Both biomarkers have been tested in a large number of diagnostic studies
on infections and sepsis but have yielded great variability of results with wide
ranges of sensitivity and specificity.
- These diagnostic studies were performed in heterogeneous clinical settings,
and many of them had other methodological limitations in either their design or
in data analysis and reporting, which makes it difficult to interpret their overall
results and to draw practical conclusions.
uses
evaluated
1. distinguishing infectious and non-infectious SIRS
2. distinguishing sepsis from septic shock
3. recognition of the presence of nosocomial infection in ICU
patients by serial determinations (CRP)
4. diagnosis of ventilator associated pneumonia
5. diagnosis of community acquired pneumonia
6. monitoring the response of infection to therapies (particularly CRP)
7. guidance of duration of antibiotic therapy (PCT)
8. decision on whether to initiate antibiotic therapy in non-ICU setting (PCT)](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-109-320.jpg)
![diagrams
of renal
replacement
modes
[created by
Paul Young
06/01/08]
slow
continuous
ultrafiltration
continuous
venovenous
haemofiltration
continuous
venovenous
haemodialysis
continous
venovenous
haemodiafiltration
continuous
high flux
dialysis
continous
plasmafiltration
absorption](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-110-320.jpg)
![diarrhoea
in critical
illness
[created
25/10/07
by Paul
Young]
pathophysiology
aetiology
general
- Diarrhoea is a common finding in critically ill patients, whatever
the initial cause of admission into the intensive care unit (ICU).
- Reported incidences of diarrhoea may vary over a very wide range
because of the lack of standardisation in the definition of diarrhoea.
enteral
feeding
associated
diarrhoea
General
- The commonly reported presence of diarrhoea during the enteral infusion
of feeds can be explained by the composition of enteral formulas, as well as
by the characteristics of administration, including the site and the mode
of infusion.
- Enteral feeding is sometimes interrupted or its infusion rate is decreased,
in contradiction with current recommendations and with the available evidence.
- Many experimental and clinical studies have demonstrated that, in comparison
with total parenteral nutrition, enteral nutrition can actually reduce the incidence
of diarrhea via a better preservation of the gastrointestinal mucosal structure
and function.
Site of infusion
- In a large multicentre prospective randomized study, Montejo et al. compared
the efficacy and rate of complications associated with the early gastric versus the
early jejunal route in 101 patients. The incidence of diarrhoea was identical (14%)
in both groups, although the total number of gastrointestinal complications (mainly
high gastric residues) was lower in the group fed in the jejunum than in the group
fed in the stomach.
- These findings somewhat challenge previous beliefs that intragastric infusion
favours diarrhoea via the stimulation of fluid secretion into the ascending colon,
or of intrajejunal infusion favouring diarrhoea via hyperosmolarity (> 400 mosm/l)
in the small intestine or via a neurohumoral reflex.
Mode of administration
- The administration of enteral feeding can be pump-driven or controlled by
gravity, continuous or intermittent. These aspects also affect the incidence of
diarrhoea.
- For example, the use of pump-assisted infusion dramatically reduced the
incidence of diarrhoea compared with gravity-controlled infusion
- Similarly, new data recently recorded in trauma and elderly patients confirmed
a better prevention of diarrhoea with the use of continuous rather than intermittent
enteral infusion of feeds, although the advantage of the continuous mode was no
longer observed during diarrhoea
Composition of enteral formulas
- Several characteristics of enteral formulas have been associated with an increased
incidence of diarrhoea, including the amount of carbohydrates, fat, high osmolarity
and bacterial contamination.
antibiotic-
associated
diarrhoea
- Although the changes in gut microflora are not specific and the associated diarrhoea
usually resolves spontaneously, only the finding of C. difficile requires a specific therapy.
- C. difficile is an anaerobic toxin-producing Gram-positive bacillus. The toxin triggers
inflammation, necrosis of the bowel mucosa, and even colon dilatation up to perforation.
- The diagnosis of C. difficile colitis is confirmed by the presence of the toxin in the stools.
- C. difficile is the most common cause of infectious nosocomial diarrhoea,
- Clostridial colitis actually occurs when the equilibrium of gut flora is severely perturbed,
thereby allowing the growth of C. difficile.
- Risk factors for the development of C. difficile-related diarrhoea include:
(i) recent or current antibiotic therapy,
(ii) a prolonged stay in the ICU
(iii) treatment with a proton pump inhibitor
(iv) female gender
(v) enteral nutrition
- Among antibiotic agents, there are striking differences in the prevalence of Clostridium-associated
diarrhoea. In particular, the use of quinolones and Cephalosporins are commonly associated with
an increased risk, whereas the use of macrolides was found to be less risky
- Once diagnosed, if symptoms are mild, no specific treatment is required in addition to the
discontinuation of antibiotic therapy. Metronidazole is presently recommended in moderate to
severe C. difficile-associated diarrhoea.
- In the case of failure of metronidazole treatment, oral vancomycin can be
given; other potential therapy includes fucidic acid, vancomycin and teicoplanin.
other
risk
factors
- In a multicentre study published in 1997, Bleichner and colleagues identified the following risk factors for diarrhoea:
(i) fever or hypothermia,
(ii) the presence of an infection site,
(iii) malnutrition, & hypoalbuminaemia (< 26 g/l),
(iv) sepsis syndrome,
(v) multiple organ failures,
(vi) open feed container, and
(vii) previous total parenteral nutrition.
effects
- In adult ICUs in western countries, diarrhoea is more often a cause than a consequence
of malnutrition, in contrast to less developed areas, where the opposite holds true
- If left untreated, diarrhoea-induced malnutrition can increase morbidity. The management
of diarrhoea-induced malnutrition can be complicated by the poor absorption of nutrients
given enterally; in this case the adjunction of parenteral support may be justified.
- Besides malnutrition, critically ill patients presenting with severe diarrhoea are particularly
at risk of haemodynamic instability, as a result of sudden shifts in the blood circulating volume
related to diarrhoea itself.
- Similarly, metabolic acidosis is often observed as a consequence of massive digestive losses
of electrolytes and bicarbonate ions. Not surprisingly, the mineral balance is always altered when
diarrhoea persists over a few hours; accordingly, the stores of potassium, magnesium and zinc can
be significantly depleted and must be compensated, because of their roles in the prevention of arrhythmias,
membrane stability, and wound healing.
preventive &
therapeutic
measures
General:
- In addition to generous hydration with sodium and sugar-containing solutions,
oral opioids or anticholinergic medications can be considered.
NB: the use of opioids including loperamide can induce a paralytic
ileus when used with other drugs, impairing gut motility.
1. Composition of enteral formulas
- Enteral feeding formulas of low osmolarity and enriched with fibres should be preferred.
- Dietary fibres have been added to enteral nutrition formulas to normalise bowel function.
The beneficial effect on bowel function results from the release of short chain fatty acids
(SCFAs) after the fermentation of carbohydrates of fibres in the colon. SCFAs (butyrate,
propionate and acetate) play an important role in salt and water absorption in the colon,
with butyrate being the main energetic fuel for colonocytes.
- Soy polysaccharides, which contain 94% insoluble fibre, are the most common source of fibre in
enteral formulas, but can be less efficient for the prevention of diarrhoea than water soluble fibres.
- Water-soluble fibres, such as pectin and guar gum, have better potential trophic effects, increase the
viscosity of the solutions, can delay gastric emptying and absorption in the small intestine, and reduce
luminal flow by causing resistance to the propulsive action of intestinal contractions.
2. Modulation of gut microflora
(i) probiotics: a preparation or a product containing viable defined microorganisms in sufficient
numbers, which alter the microflora by implantation or colonization in a compartment of the host
and that exert beneficial effects in the host),
(ii) prebiotics: a non-digestible food ingredient that beneficially affects the host by selectively stimulating
the growth or activity of one or a limited number of bacteria in the colon, and thus improving host health
(iii) synbiotics: a combination of prebiotics and probiotics able to modulate gut immunity and facilitate
nutrient/factor interaction necessary for gut recovery
3. antimotility drugs:
- Antimotility drugs may be of symptomatic benefit in adults with mild or moderate acute diarrhoea.
- They are contraindicated in patients with severe or bloody diarrhoea, where there is a possibility
of invasive organisms, and in patients with severe inflammatory bowel disease because of the risk
of toxic megacolon.
- If an antimotility drug is considered appropriate, it is reasonable to use:
loperamide 4 mg orally, initially, followed by 2 mg orally, after each unformed stool, up to 16 mg per day
OR
diphenoxylate+atropine 5+0.05 mg orally, 3 to 4 times daily initially, reducing dose as soon as symptoms improve
OR
codeine 30 to 60 mg orally, up to 4 times daily.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-111-320.jpg)





![ectopic
pregnancy
[created by
Paul Young
02/10/07]
definition
aetiology
investigation
treatment
- an ectopic pregnancy is a fertilised ovum
which implants outside the lining of the uterus
symptoms
signs
- most important part of the examination is the pelvic. Look for:
1. adnexal tenderness & masses
2. state of cervix & material passing through it (large
amount of blood is inconsistent with ectopic pregnancy)
- important things from the history are:
1. presence & amount of PV bleeding (occurs in 80%)
2. location of pain
3. risk factors for ectopic pregnancy
4. LMP
5. shoulder pain (suggests large
amount of peritoneal blood)
6. faintness
- perform a pregnancy test (a negative urine
test essentially excludes ectopic pregnancy -
it has a negative predictive value of 99%)
perform blood tests for:
- exclusion of other causes of abdominal pain
- rhesus status
risk factors for ectopic pregnancy include:
- history of tubal ligation
- history of ectopic pregnancy
- prior tubal infection
- fallopian and endometrial anomalies
- fertility drugs
- endometriosis
- IUCDs
NB: 50% of patients with proven ectopic
pregnancy have no risk factors
- most people with ectopic (97%)
present with abdominal or pelvic pain
rate of coexistent intrauterine & ectopic pregnancy
is about 1/5000 in patients not on fertility treatment
- listen for fetal heart tones (they are almost never heard in ectopic)
perform MSU
- most important test is a transvaginal pelvic USS
- if bHCG is <1200 an IUP is seen on only 20% of scans
- if bHCG is >1200 and there is no IUP seen this
is very good evidence of an ectopic pregnancy
- serial bHCG is useful in patients with non-diagnostic
scans
- normal increase in bHCG in the 1st trimester is 1.66Xs
every two days. 20% of normal pregnancies do not
show this rise & 20% of ectopics show this rise
- treat patiients with haemorrhagic shock or peritonitis
with fluid resuscitation & transfer to theatre
treatment options are:
1. surgery. Used for:
- unstable patients
- large ectopics
- patients with peritonitis
2. methotrexate. Used for:
- no peritonitis
- ectopic <3.5cm
- no free fluid on USS
- ability to closely monitor as an outpatient](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-117-320.jpg)


![emergent
valvular
disorders
[created by
Paul Young
11/10/07]
general
- includes both acute valve dysfunction resulting in
acute heart failure & chronic valve disease with
decompensation due to increased metabolic demands
- regurgitation is the most common type of acute valve
dysfunction; with rare exceptions stenosis is a chronic, slowly
progressive condition.
- in patients with asymptomatic chronic stenosis, decompensation
can occur due to a superimposed haemodynamic burden
- examples of this include mitral stenosis presenting with acute
pulmonary oedema in the setting of systemic infection & aortic
stenosis presenting with cardiogenic shock in the setting of acute
GI bleeding
causes of
acute valve
dysfunction
mitral regurgitation:
- myxomatous disease with flail leaflet
- spontaneous chordal rupture
- endocarditis
- in acute myocardial infarction due to:
(i) papillary muscle rupture
(ii) regional wall motion abnormality
(iii) left ventricular dilation and systolic dysfunction
aortic regurgitation:
- endocarditis
- spontaneous rupture of a congenital fenestration
- aortic dissection
tricuspid regurgitation:
- endocarditis
- penetrating chest trauma
- blunt chest trauma
prosthetic valves:
- endocarditis
- valve thrombosis
- paravalvular dehiscence
- leaflet tear
aortic
regurg
general:
- chronic aortic regurg is most often due to a congenital bicuspid
aortic valve, rheumatic valve disease or aortic root dilation
- there are numerous causes of aortic root dilation including hypertension,
cystic medial necrosis, Marfan syndrome & congenital bicuspid aortic valve
- the most common causes of acute aortic regurgitation are endocarditis,
rupture of a congenital fenestration and acute aortic dissection
- endocarditis results in aortic regurgitation by destruction of valve leaflet tissue
& is often associated with paravalvular abscess
- aortic dissection can cause AR by either enlargement of the aortic annulus
or extension into the valve region causing flail
clinical presentation:
- acute backflow from the aorta into the LV results in elevated LVEDP
which leads to acute pulmonary oedema
- because there is no time for compensatory LV dilatation, forward cardiac
cardiac output falls abruptly due to regurgitant flow in diastole so that patients
with acute AR may be in cardiogenic shock
- decreased coronary perfusion pressure results in subendocardial ischaemia
further impairing LV function
mitral
stenosis
management:
- acute aortic regurgitation is a surgical emergency
- preoperative management is supportive with ventilatory support and haemodynamic monitoring
- if aortic aortic regurgitation is due to aortic dissection, acute surgical intervention is needed.
The surgical approach may be replacement of the ascending aorta and valve with a Dacron or
Gore-Tex valved conduit. When the valve leaflets are normal, some centres will preserve the
native valve in a prosthetic conduit (called the David procedure)
- when acute aortic regurgitation is due to endocarditis, surgical options include a mechanical
valve, heterograft tissue valve or cryopreserved homograft aortic valve
general:
- mitral stenosis is nearly always due to Rheumatic heart disease & is
a slowly progressive disease with insidious onset over many years
- rarer causes are left atrial myxoma, ball-valve thrombus, annular calcification, SLE
clinical presentation:
- in asymptomatic patients with compensated moderate or severe mitral
stenosis, acute decompensation can occur in the setting of increased
systemic haemodynamic demands
- because mitral stenosis most commonly occurs in women (80%) and
occurs in the reproductive years, the most common emergency presentation
is of a pregnant or post-partum woman with heart failure
- the clinical presentation may also be caused by or exacerated by atrial fibrillation
- main symptoms are breathlessness on exertion, recurrent bronchitis, fatigue, palpitations,
AF, haemoptysis and stroke
- classic signs are mitral facies, small volume pulse, right ventricular hypertrophy, a tapping
apex due to a palpable first heart sound, a loud first heart sound & an opening snap with a
diastolic murmur
management:
- most patients with mitral stenosis and acue decompensation can
be managed conservatively with treatment of the superimposed illness
- efforts should be directed towards increasing oxygen delivery and
decreasing oxygen demand
- if atrial fibrillation is present rate and/or rhythm control is required
- beta blockers may improve ventricular function by improving diastolic filling
- in patients who do not respond to conservative therapy, urgent percutaneous balloon mitral
valvotomy should be performed; patients with left atrial thrombus, co-existing moderate to
severe MR or deformed valves may require urgent valve replacement
right-
sided
disease
- pulmonic valve disease is nearly always congenital in origin with a chronic disease course
- tricuspid valve stenosis is rare and usually accompanies rheumatic mitral valve disease
- tricuspid regurgitation can present acutely with severe aortic regurgitation due to
endocarditis or to blunt or penetrating chest wall trauma
mechanical
valves
- mechanical heart valves are very durable and complications are most
often due to valve thrombosis or paravalvular regurgitation
- valve thrombosis occurs in the setting of inadequate anticoagulation & may result in either functional
stenosis or regurgitation (depending on whether the clot impedes opening or closing of the valve)
- treatment of valve thrombosis is controversial with options including
systemic anticoagulation, thrombolysis and occasionally urgent surgery
- paravalvular regurgitation early after valve replacement may be related to suture
dehiscence at a site of annular calcification. There may be associated haemolytic anaemia.
- can be treated conservatively, but may require re-operation if severe
- new onset of paravavular leak shold prompt careful evaulation for endocarditis
tissue
valves
- tissue valves are subject to degeneration of the leaflets with
superimposed calcification that may result in stenosis or regurgitation
- degeneration is usually a slowly progressive process with presentation 10-15 years after valve replacement
- as with native valve disease, acute decompensation can occur with superimposed haemodynamic stress
aortic
stenosis
general:
- valvular aortic stenosis in adults is most commonly due to calcification
of a normal trileaflet or bicuspid aortic valve
clinical features:
- aortic stenosis is a chronic, slowly progressive disease that presents acutely
only at a late stage or in the face of increased haemodynamic demands due to
intercurrent illness
- the main symptoms are angina, syncope & breathlessness
- typical signs are a slowly rising pulse, evidence of LVH & a harsh systolic murmur
radiating into the neck
management:
- most patients with decompensated aortic stenosis can be managed conservatively
by treating the underlying disease process that led to the acute decompensation
- a preliminary study has shown that cautious use of nitroprusside may improve
haemodynamics before valve replacement in patients with severe decompensated
aortic stenosis and a mean arterial pressure greater than 60mmHg
mitral
regurg
general:
- MR may be caused by disease of distortion of any component of the mitral valve apparatus
including the mitral valve annulus, leaflets, chordae & papillary muscles as well as by alterations in
left ventricular geometry or systolic function
clinical presentation:
- although patients with chronic mitral regurgitation may be asymptomatic for many years, the regurgitant
lesion imposes a volume load on the left ventricle because an increased total stroke volume is needed to
maintain a normal forward cardiac output
- chronic mitral regurgitation is usually well tolerated even when there is a superimposed
haemodynamic load such as systemic infection, pregnancy or trauma
- chronic mitral valve severity may suddenly worsen due to:
(i) a sudden increase in afterload for example due to hypertensive crisis
(ii) alteration in LV geometry resulting in a larger regurgitant oriface area (for
example left ventricular dilatation due to decompensated heart failure)
- acute mitral regurgitation presents with pulmonary oedema and is a surgical emergency
management:
- in chronic MR and heart failure, management is directed at treating the
process that lead to decompensation & optimising loading conditions
- acute severe MR is a surgical emergency. Medical stabilisation should occur
concurrently with cardiac surgical referral. Acutely, placement of an IABP provides
optimal afterload reduction while improving diastolic coronary blood flow.
- timing of surgical intervention depends on the aetiology of the acute MR:
(i) spontaneous chordal rupture can usually be treated with mitral valve repair
(ii) timing of repair in endocarditis varies but most centres favour repair as early as
possible and recent studies suggest delaying surgery does not decrease infection
(iii) acute ischaemic MR due to RWMAs may improve after percutaneous revascularisation
& IABP and medical therapy may be sufficient to get patient through as myocardial
function improves
(iv) acute ischaemic MR due to papillary muscle rupture requires urgent surgery
[urgent surgery has a 50% mortality; however, without surgery complete rupture has
a 95% two week mortality]. Some surgeons advocate a period of medical stabilisation
in the presence of partial papillary muscle rupture](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-120-320.jpg)
![Endocarditis
[created by
Paul Young
02/10/07]
therapy
rare cause
of endocarditis
that are culture
negative
risk factors
- Risk of native-valve disease is classically associated with
congenital heart disease and chronic rheumatic heart disease.
- mitral valve prolapse is a more controversial issue; patients with
valve regurgitation have an increased risk of infective endocarditis.
- Degenerative valve lesions are a primary cause of senile aortic
stenosis or mitral regurgitation, which are risk factors for infective
endocarditis.
- 1–5% of individuals with infective endocarditis have prosthetic-
valve endocarditis. Whether mechanical valves or bioprostheses
are more prone to infection remains unresolved.
- IV drug use
prosthetic
valve
endocarditis
- PVE is classified as either early or late infection, depending on
whether the infection arises within 60 days of surgery or later.
- The condition peaks during the first 2 months after valve implantation
and is often due to Staphylococcus epidermidis or Staph aureus.
- Progressive endothelialisation of the prosthetic material over
2–6 months reduces the susceptibility of the valve to infection.
- Late PVE is often due to other organisms:
eg, streptococci and gram-negative bacteria of the HACEK group,
Haemophilus spp, Actinobacillus actinomycetemcomitans, Cardiobacterium
hominis, Eikenella corrodens, and Kingella kingae
iv
drug use
- Intravenous drug users represent a risk group of fairly
young people (median age 30–40 years).
- The tricuspid valve is infected in more than 50% of cases, followed by
the aortic valve in 25% and the mitral valve in 20%, with mixed right-sided
and left-sided infective endocarditis in a few instances.
- 60–80% of patients have no known preexisting valve lesions.
- The pathogens usually originate from the skin, explaining the predominance
of Staph aureus. Pseudomonas aeruginosa and fungi are also encountered
and produce severe forms of infective endocarditis.
- In HIV-1-positive intravenous drug users, both the risk of and mortality from
infective endocarditis rise inversely to the CD4 count; risk is unaffected in
patients with CD4 counts of more than 500 cells per microL, but increases
four-fold in those with CD4 counts of less than 200 cells per microL
- HIV-1-positive patients sometimes present with infective endocarditis
caused by unusual organisms, including bartonella, salmonella, and listeria.
- Nosocomial endocarditis
- Haemodialysis
nosocomial
endocarditis
- Nosocomial endocarditis is a growing category
- Less than 50% of patients had cardiac predisposing factors.
- Predominant pathogens were staphylococci and enterococci,
and were frequently associated with catheters or medicosurgical
procedures.
- The authors of one study estimated that up to 13% of nosocomial Staph
aureus bacteraemia were responsible for subsequent infective endocarditis.
Moreover, possible right-sided nosocomial endocarditis was reported in
5% of bone-marrow transplant recipients who had central venous catheters.
- Nosocomial endocarditis is important because its case fatality rate is
greater than 50%.
- Another iatrogenic risk for infective endocarditis is haemodialysis. The
disease is two to three times more frequent in haemodialysis patients
than in peritoneal dialysis patients or in the general population. More
than 50% of cases are due to Staph aureus.
Brucella
C. burnetti
Bartonella
Chlamydia
Mycoplasma
Legionella
Whipples](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-121-320.jpg)
![endotracheal
tubes
[created by
Paul Young
21/12/07]
standard
Pilot balloon
onewayvalve
Pilot tube
Cuff
Connector
Radio-opaqueline
indicator mark
Sizemarking
Murphy‘s eye
Intubationdepthmarkings
Angledtip
Features
- 33cm length, size is the internal diameter in mm
Materials
- Non-toxic, clear, thermo sensitive siliconised PVC which gets soft when warm
Parts
- All tubes are fitted with 15 mm standard connector, which insures compatibility with circuit connectors
- Smooth tip aids atraumatic intubations
- Full-length radio-opaque line to assess exact location of tube 1 cm graduation markings to ascertain
insertion depth
- 2 cm indicator mark assists positioning of tube past the vocal cord
- Latex free
laser
tube
- Used in ENT laser surgery
- laser resistant coat
- one or two cuff balloons (blocked with water)
Edgar
tube
- EDGAR tube, for endobronchial drug and gas application during resuscitation
Oxford
tube &
RAE
tube
- non kinking oxford tube with a right angle shape for difficult airway
cuff
pressure
- above 18 mmHg to reduce aspiration
- below 25 mmHg to minimize the risk of pressure necrosis
- Patients whose peak airway pressures exceed 48 cmH2O will require
cuff pressures greater than 25 mmHg in order to avoid a cuff leak.
paediatric
tube size
ID (mm) = (16 + age) /4intubation depth length (cm )/10
- If unsure choose size of the pinkie
double
lumen
tubes
RAE tube
- RAE (Ring-Aldair-Elwyn )
- for ENT, ophthalmic and neurosurgery
so tube is directed away from operative field
Oxford tube
cuff
pressure
- above 18 mmHg to reduce aspiration
- below 25 mmHg to minimize the risk of pressure necrosis
- Patients whose peak airway pressures exceed 48 cmH2O will require
cuff pressures greater than 25 mmHg in order to avoid a cuff leak.
tubes for
premature
infants
Reinforced
Woodbridge
tube
- Tubes are made of silicone with an integral steel reinforcing wire
- Used to provide a safe, kink-resistant airway regardless of head or neck position.
- Requires a biteblocker because biting can lead to tube blocking tube](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-122-320.jpg)

![Enterobacter
[created by
Paul Young
02/10/07]
general
- Enterobacter spp. are motile Gram-negative bacilli that produce ornithine
decarboxylase and are urease negative.
- These features distinguish them from Klebsiella spp.
- Enterobacter spp. are ubiquitous organisms found in human and animal
faeces and in the environment, including water, plants and plant materials.
infections
& colonisation
- Of the 14 species, Enterobacter aerogenes and Enterobacter cloacae are
the most commonly isolated and are particularly important nosocomial
pathogens in the ICU.
- They cause a variety of infections including bacteraemia, pneumonia,
urinary tract and surgical wound infections.
- The most frequently cited risk factor for Enterobacter infection is prior
exposure to antibiotics. It appears that the combination of severe debility
and the effect of antibiotics on normal flora provide a selective environment
favouring colonisation and subsequent infection with Enterobacter spp
- The majority of infections are likely to be endogenous in origin from
chronically colonised patients, which implies that infection control
practices are unlikely to have a major effect on the overall incidence of
Enterobacter infection.
resistance
- All species of Enterobacter possess an inducible, chromosomally encoded
beta-lactamase known as AmpC. This enzyme confers resistance to broad-
spectrum penicillins, second and third generation cephalosporins and aztreonam,
and is not affected by beta-lactamase inhibitors like clavulanate.
- Treatment with broad-spectrum penicillins and cephalosporins, while able to
eliminate 'wild-type' strains with inducible AmpC beta-lactamase, preferentially
selects out these so-called stably derepressed mutants; this results in treatment failure.
- Resistance to aminoglycosides and other antibiotics is often encoded
on the plasmids carrying extended-spectrum beta-lactamases, and it is
postulated that this may be one of the selective forces behind acquisition
of extended-spectrum beta-lactamases in Enterobacter
- Resistance to carbapenems can occur when high level AmpC expression
coincides with loss of outer membrane porin proteins; fortunately, this is rare
- The only agents that maintain activity against the mutants are the
carbapenems and newer fourth generation cephalosporins like cefepime.
therapy
- While AmpC beta-lactamase production is the main mechanism of antibiotic resistance in
Enterobacter spp., plasmid-borne extended-spectrum beta-lactamases are also encountered.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-124-320.jpg)
![enterococcus
[created by
Paul Young
02/10/07]
general:
- Enterococci are enteric Gram-positive cocci
originally included in the genus Streptococcus.
- Although over a dozen species have been identified, only two are
responsible for the majority of human infections, Enterococcus faecalis
and Enterococcus faecium. They account for 85–90% and 5–15% of
clinical isolates, respectively, although infections caused by the latter are
on the increase.
- Other species (E. gallinarum, E. casseliflavus, E. durans,
E. avium and E. raffinosis) account for less than 5% of isolates
epidemiology
& resistance
- Vancomycin has been used widely for the treatment of
E. faecium and E. faecalis infections since the 1980s.
- Enterococci were the first bacteria to develop vancomycin
resistance. Vancomycin-resistant Enterococci have now been
identified world-wide.
- The appearance of resistance coincides with an increase
in the use of cephalosporins, to which Enterococci
are naturally resistant.
- Also implicated is the oral use of vancomycin in the treatment
of Clostridium difficile, and its parenteral use in the treatment
of methicillin-resistant S. aureus infections.
- Vancomycin resistance is mediated through a complex interplay
of many genetic elements found on the van gene clusters
colonisation
& infection
- Enterococci are a part of the normal enteral flora of both humans and animals
- Although vancomycin-resistant Enterococci are most commonly isolated from the
gastrointestinal tract, they have also been recovered from the groin, intact skin of the
upper arm, oropharynx and gastric and tracheal aspirates in hospitalised
patients.
- Enterococci have low pathogenic potential except in patients who are severely
ill or immunocompromised. Hence reports of vancomycin resistant enterococcal
infections are mainly from ICUs, organ transplant and renal units and oncology wards.
- Colonisation of healthy individuals with vancomycin resistant
Enterococci, unlike methicillin-resistant S. aureus, does not necessarily
increase the risk of subsequent infection with these organisms.
- In many affected institutions, most vancomycin-resistant Enterococci are
isolated from colonised rather than infected patients and are found in
association with other more virulent organisms.
- There is an association between colonisation with VRE and the oral or
parenteral use of vancomycin, cephalosporins and anti-anaerobic drugs
(metronidazole, clindamycin and imipenem).
- Eradication of species which normally compete with Enterococci produces a selective
environment where small numbers of vancomycin-resistant Enterococci may multiply.
- However, exposure to antibiotics alone will not select for VRE if resistant bacteria are
not already present therefore need to be exposed to VRE to become colonised with it
transmission
- Hand-washing with soap and water is ineffective in removing VRE and
aqueous chlorhexidine and povidone-iodine solutions are unreliable.
- Only alcoholic chlorhexidine and alcohol have been found to be effective
- The extent to which environment surfaces act as a source from which VRE are able to
spread is still uncertain. However, it is known that VRE may remain viable on surfaces
for weeks because they are resistant to desiccation and to extreme temperatures
- At present, there is no evidence that VRE are spread by the airborne route
infections
- Enterococci are the second or third most common pathogen identified
in urinary tract infections, bacteraemia and wound infections.
- They are rarely responsible for respiratory tract infections, cellulitis or
osteomyelitis.
- Although unusual, endocarditis is well-described. Enterococci are responsible
for 5–15% of all cases of endocarditis and are associated with considerable morbidity
and mortality. Endocarditis is a potential complication of enterococcal bacteraemia and
is becoming increasingly difficult to treat because of multiple antibiotic resistances.
- Enterococcal meningitis is also rare and is usually
associated with surgery and other instrumentation
antimicrobial
therapy
- The treatment of sensitive enterococcal infections is difficult for several reasons:
(i) Enterococci are intrinsically resistant to many commonly used antimicrobials.
(ii) Many useful agents are only inhibitory at clinically unachievable
concentrations, which limits the effectiveness of therapy.
(iii) Where bactericidal action is required, dual or triple therapy becomes necessary.
It is often unclear if an enterococcal isolate requires treatment, especially if isolates
are recovered from polymicrobial bacteraemias or mixed wound infections
(iv) Enterococci easily acquire resistance to available antibiotics, either by
mutation or by receipt of foreign genetic material through plasmids and transposons.
- The resistances that cause the most severe therapeutic problems include high level
ampicillin resistance, which is seen in some isolates of E. faecium, high level
resistance to aminoglycosides, seen in both E. faecium and E. faecalis, and
vancomycin resistance, which has developed preferentially in E. faecium
- The optimum antibiotic for documented infection with VRE is not established
- Although E. faecalis and particularly E. faecium are intrinsically resistant to
penicillin, nearly all E. faecalis isolates are at least moderately susceptible to ampicillin
Thus, most vancomycin-resistant E. faecalis isolates can be treated with ampicillin.
- bactericidal combination of a cell wall inhibiting agent plus an aminoglycoside
is considered standard treatment for deep-seated infections. However, this synergistic
action may not always be suitable because of high-level gentamicin resistance, which
also confers resistance to tobramycin, netilmicin, amikacin and kanamycin, though not to
streptomycin, which may remain useful.
- Quinupristin / dalfopristin is approved for use against serious or life-threatening infections
caused by E. faecium. It is inactive against E. faecalis and is bacteriostatic against E. faecium;
the lack of bactericidal activity may compromise its clinical and bacteriological activity.
- Linezolid shows excellent inhibitory activity against most vancomycin-resistant isolates.
There are reports of the successful use of linezolid in the treatment of E. faecium meningitis
and bacteraemia
- Chloramphenicol is one of the few agents to retain in vitro activity against many strains of
multiply resistant E. faecium. It has been used with moderate success in the treatment of VRE
bacteraemia and remains a reasonable choice for the treatment of meningitis. However, two
factors may limit its clinical use. Firstly, resistance is increasing and secondly, there is a risk
the drug may cause fatal bone marrow suppression
- Nitrofurantoin is active against most Enterococci regardless of vancomycin resistance, and
it remains useful for the treatment of urinary tract infections](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-125-320.jpg)

![paradural
abscess
[created
by Paul
Young
17/11/07]
general
- the epidural space is the space between the dura and the bony
structure of the the skull and the vertebral column while the subdural
space is the space between the subarachnoid membrane and the
dura
- although subdural abscesses are more common within the cranium
& epidural abscesses are more common within the vertebral column,
the causes, pathophysiology & therapies are similar
subdural
abscess
- in the skull, the epidural tissues are dense and the abscess formation
is unusual; the subarachnoid membrane is much less adherent to the
dura, making the subdural space the more likely site of infection
- cranial subdural abscess may be clinically indistinguishable from
brain abscess
epidural
abscess
general
- within the vertebral column a thin layer of fat and blood vessels
separate the dura from the vertebral column making the epidural
space a more common site of infection than the subdural space
- once an infection develops in the epidural
space it may dissect for a considerable distance
causative organisms
- usually associated with infection of the paranasal sinuses & less commonly
of the ears and mastoids; trauma, surgical intervention, or haematogenous
sources cause the remaining cases
- organisms common to sinusitis, including streptococci, pneumococci,
H. influenzae, anaeoribes, and staphlococci cause most infections
- gram negative enteric bacilli may be associated with middle ear and
mastoid infections
clinical manifestations:
- usually begins with localised spinal pain
- higher functions are generally intact
- symptoms usually progress through four clinical phases of spinal ache, nerve
root pain, radicular weakness and paralysis
- back pain with fever, focal tenderness & sensory & motor deficits strongly
suggests this disease
aetiology
- S. aureus accounts for 2/3rds of epidural abscess
- 80% of spinal epidural abscess is community acquired while 20% of cases
occur after spinal instrumentation (surgery or epidural); in the latter population
causative organisms may include nosocomial infections such as MRSA or
pseudomonas
- a source of haematogenous seeding may be identified in 75% of patients
risk factors for epidural abscess include:
(i) spinal instrumentation
(ii) iv drug use
(iii) diabetes mellitus
(iv) trauma
(v) dialysis
treatment
- antibiotics alone are inadequate if there is evidence of nerve compression
& neurosurgical drainage remains the mainstay of treatment; if nerve compression
is present, decompression within 24 hours offers the best chance of recovery
investigation:
- diagnosis hinges on visualisation of a collection in the epidural space
- MRI is the diagnostic modality of choice because it defines cord compression
& the presence and extent of abscess, identifies drainable paraspinal collections
& detects concomitant vertebral osteomyelitis
- CT scanning can be performed in MRI is not available
- non surgical management might be considered if a pathogen is identified by
peripheral blood cultures or by needle biopsy if there is no progression of
neurological findings on frequent examination, if pain improves, white cell count
declines & fever settles with treatment
differential diagnosis:
- degenerative disease of metastatic tumour may mimic epidural
abscess (especially if fever is present); MRI will distinguish these
- treatment should be based on the Gram stain and culture results of operative material.
- Initial empirical therapy should be commenced prior to surgery. Antibiotic guidelines
recommend:
flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
PLUS
gentamicin 4 to 6 mg/kg (child <10 years: 7.5 mg/kg; =10 years: 6 mg/kg) IV, daily
(adjust dose for renal function, see Monitoring and dosing of aminoglycosides).
- For patients with penicillin allergy, substitution of vancomycin for flucloxacillin is
recommended
- antibiotic guidelines recommend subdural empyema be treated with the same
antibiotic regime as a brain abscess](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-127-320.jpg)
![epidurals
general
- An injection of an anesthetic or analgesic into the epidural space
of the spinal cord resulting in regional anesthesia or analgesia
use
(i) Surgical anaesthesia and post-operative analgesia
- Thoracic / Abdo / Pelvic / Lower limb surgery
(ii) Obstetrics
(iii) Chronic pain
relevant
anatomy
insertion
- Consent
- Preparation + position
- Asepsis
- Level (middle of surgical incision)
- Local anaesthetic
- Loss of resistance
- Thread catheter
- Position catheter
- Secure
- Test dose
- Bolus / Infusion
drugs
(ii)Opioid
- Fentanyl
- Diamorphine
- Morphine
Supplemental analgesia
(i)Local anaesthetic
- Lignocaine
- Bupivicaine
- Ropivicaine
Neural Blockade [Motor, Sensory, Autonomic]
side
effects
local anaesthetic side effects
(i)Motor block
- Respiratory failure
(ii) Sensory block
- Thermal / Pressure injury
(iii) Proprioception loss
- Unsteadiness
(iv) Autonomic blockade
- CVS
- Hypotension (hypovolaemia)
- Bradycardia
(v) Visceral dysfunction
opioid side effects
Respiratory depression
Pruritus
Nausea / Vomiting
complications
potential
benefits
analgesic benefits
physiological benefits
System Effects of Epidural Result
CVS •Improved myocardial O2 supply:demand, reduced
SVR
•Reduced BP
•Reduced myocardial ischaemia
•Reduced blood loss
Coag Improved blood flow, reduced platelet stickiness, less
inhibition of fibrinolysis
Reduced venous
thromboembolism
Improved graft outcome
Resp Improved lung mechanics (increased compliance), less
diaphragmatic dysfunction
Improved oxygenation
Earlier extubation
Fewer pulmonary infections
GI Increased motility, improved blood flow Earlier return of bowel
function
Stress
response
Reduced/Abolishes neuroendocrine response to stress Prevents complications of this
System Effects of Epidural Result
CVS •Improved myocardial O2 supply:demand, reduced
SVR
•Reduced BP
•Reduced myocardial ischaemia
•Reduced blood loss
Coag Improved blood flow, reduced platelet stickiness, less
inhibition of fibrinolysis
Reduced venous
thromboembolism
Improved graft outcome
Resp Improved lung mechanics (increased compliance), less
diaphragmatic dysfunction
Improved oxygenation
Earlier extubation
Fewer pulmonary infections
GI Increased motility, improved blood flow Earlier return of bowel
function
Stress
response
Reduced/Abolishes neuroendocrine response to stress Prevents complications of this
troubleshooting
Failure of
analgesia
High block
Local
anaesthetic
toxicity
Anticoagulation
Post dural
puncture
headache
Neurological
complications
(i)Assess block
- Motor
- Sensory
- Autonomic
- Unilateral/Patchy/Too low /No block
(ii) Check site
(iii) Give top up
- Opioid or local anaesthetic
(iv) Withdraw catheter
(v) Consider subdural catheter*
(vi) Resite epidural
* Subdural block: Slow onset, inappropriately extensive, Horner's
syndrome, patchy, asymmetrical, motor sparing, risk of total spinal
(i) Stop / reduce rate
(ii) Do not lie patient flat
(iii) Treat side effects
- either due to a cumulative effect or direct intravascular injection
Presentation
(i) Peri-oral tingling, slurred speech, tinnitus
(ii) Altered consciousness, confusion, coma
(iii) Arrhythmias, CVS collapse, respiratory arrest
Treatment options include:
(i) Naloxone
(ii) Ondansetron?
(iii) Antihistamines
Treatment options for hypotension include:
(i) Check fluid status - ? Relative hypovolaemia
(ii) Raise legs
(iii) Fluid
(iv) Ephidrine
(v) Reduce infusion rate
- Features
(i)Onset 24-48h
(ii) Lasts 10-14 days
(iii) Postural
(iv) Fronto-occipital, radiates to neck
(v) Photophobia, diplopia
(vi) Nausea
Management
(i) ABC
(ii) Treat / Prevent convulsions
(iii) CPR for cardiac arrest
(iv) Intralipid 20%
Total Spinal occurs in 1:5000 - 50000. It is characterised by:
(i) Difficulty coughing / breathing
(ii) Weak arms
(iii) Difficulty talking / swallowing
(iv) Cardiorespiratory collapse
Management is supportive
- Management
(i) Reassurance
(ii) Analgesia
(iii) Blood patch
Key points are a high index of suspicion with:
(i) Abnormal neurology
(ii) Unexpectedly dense block
(iii) Anticoagulation
(iv) Difficult insertion
Management requires:
(i) Early imaging
(ii) Referral to a neurosurgeon](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-128-320.jpg)

![examination
of the
comatose
patient
[created
by Paul
Young
28/11/07]
eye
signs
in
coma
limb
movements
& postural
changes
in coma
respiratory
rate & pattern
in coma
body
temperature
in coma
distinguishing
structural &
metabolic
encephalopathy
- choreoathetotic or ballistic movements suggest a basal ganglion lesion
- myoclonic movements indicate a metabolic disorder usually of post
anoxic origin
- asterixis is usually seen with metabolic encephalopathies
decerebrate rigidity (extensor posturing)
- is characterised by stiff extension of limbs, internal rotation of the arms &
plantar flexion of the ankles. These movements may be unilateral, bilateral,
spontaneous or in response to a noxious stimulus
- while animal studies suggest that the lesion is usually in the midbrain, in
humans such posturing may be due to:
(i) midbrain lesions
(ii) metabolic disorders including hypoglycaemia, hepatic coma and drug
intoxication
- hypothermia is frequently observed with alcohol or barbiturate intoxication,
sepsis, drowning, hypoglycaemia, myxoedema coma & exposure to cold
- severe hyperthermia may be seen in pontine haemorrhage, intracranial
infections, heat stroke & anticholinergic drug toxicity
- as a general rule, at lighter levels of impaired consciousness tachypnoea
predominates while respiratory depression increases with depth of coma
- precise localising value of respiratory rate & patterns is uncertain
ophthalmoscopy findings:
(i) papilloedema suggests the presence of intracranial hypertension
but it is frequently absent when the lesion is acute
(ii) subhyaloid & vitreous haemorrhages are seen in patients with SAH
eye movements:
- horizontal eye movements to the contralateral side are initiated in the ipsilateral
frontal lobe & closely coordinated in the contralateral pons. To facilitate conjugate
eye movements, yoking of the 3rd, 4th & 6th cranial nerve nuclei is achieved by
the medial longitudinal fasciculus (ie to look left the movement originates in the
right frontal lobe & is coordinated by the left pons)
- vertical eye movements are under bilateral control of the cortex & upper midbrain
- full & conjugate eye movements in response to oculocephalic & oculovestibular
stimuli demonstrates the functional integrity of a large segment of the brainstem
- upward rolling of the eyes after corneal stimulation (Bell's phenomenon) implies
intact midbrain & pontine function)
- the presence of spontaneous roving eye movements excludes brainstem pathology
as a cause of coma
- ocular bobbing, an intermittent downward jerking of eye movement is seen in pontine
lesions due to loss of horizontal gaze and unopposed midbrain controlled vertical
gaze activity
- in a paralytic frontal lobe pathology the eye will deviate towards the side of the lesion
while in pontine pathologies, the eyes will deviate away from the lesion
- skew deviation (vertical separation of the ocular axes) occurs with pontine &
cerebellar disorders
pupils:
- the presence of normal pupils (2-5mm, equal in size & demonstrating both direct &
consensual light reflexes) confirms the integrity of the pupillary pathway (retina, optic nerve,
optic chiasma & tracts, midbrain & 3rd cranial nerve nuclei & nerves)
- the size of the pupil is a balance between the opposing influences of both sympathetic
& parasympathetic systems](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-130-320.jpg)
![failed
airway
techniques
[created by
Paul Young
02/10/07]
definition
a clinical situation in which a conventionally
trained anesthesiologist experiences
difficulty with mask ventilation, difficulty with
tracheal intubation, or both.
identification
of the difficult
airway
(b) external physical characteristics
1) a short, muscular neck
2) a receding mandible
3) a protruding tongue or upper incisors
4) mandibular instability
5) facial trauma
6) restricted head and neck movement
7) facial hair
8) obesity
9) short thyromental distance (less than
three finger breadths with neck extended
predicts difficult intubation)
(a) circumstances
1) failed intubation by ambulance personnel
(c) internal physical characteristics
1) adequate mouth opening
- ability to insert 3 finger breadths
- ability to visualise soft palate & uvula as
described by the Malampati classification
Class I Soft palate, fauces, uvula,
anterior and posterior tonsillar pillars
Class II Soft palate, fauces, uvula
Class III Soft palate, base of uvula
Class IV Soft palate not visible at all
Non-surgical
techniques for
difficult intubation
Awake Intubation
- Awake intubation should be the initial approach in a
patient in whom a difficult intubation is anticipated, but
who has adequate ventilation and is able to maintain oxygen
saturation at greater than 90%. In this situation, rapid ablation
of the patient’s own respiratory drive by paralytics or general
anesthesia may complicate airway management.
- Awake intubation offers several advantages:
1) spontaneous ventilation is maintained, allowing gas exchange;
2) airway reflexes are preserved, decreasing the risk of aspiration;
3) muscle tone, and thus airway anatomy, are preserved; and
4) the significant adverse effects of pharmacological agents used
in intubation are avoided.
The awake approach can be used with virtually any intubation
technique (surgical, direct laryngoscopy, blind nasal, fiberoptic,
or an alternative device) and it is facilitated with topical or local
anesthesia.
Difficult direct larngeal intubation:
- can be facilitated by optimising patient position & use
of BURP (backwards, upwards, rightwards pressure)
The failed airway:
- the airway is a failed airway when there have been
three failed attempts at direct intubation
- failed airway can be divided into patients who can
be ventilated & patients who cannot be ventilated
Options for the failed airway:
- bougie
- LMA
- fasttrack LMA
- combitube
- lighted stylet
- blind nasal
- bronchosope](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-131-320.jpg)



![Hepatic
Failure
Management
[created by
Paul Young
02/10/07]
Hepatic
encephalopathy
grading
- Hepatic encephalopathy involves a wide range of neuropsychiatric changes in patients
with significant liver dysfunction, ranging from subtle cognitive abnormalities to coma
types
(i) Type A is related to acute liver failure.
(ii) Type B occurs in the setting of normal liver
histology and the presence of a hepatic vascular bypass,
such as portocaval shunting.
(iii)Type C hepatic encephalopathy is due to cirrhosis,
- acute encephalopathy is usually precipitated by an identifiable trigger
- chronic encephalopathy usually involves a recurrent and fluctuating course.
diagnosis:
- Diagnosis is usually established based on a combination of laboratory
abnormalities suggesting severe hepatic dysfunction and neurologic deficits.
- Elevated blood ammonia levels can be present, they are
not required for making a diagnosis.
clinical
features:
- Early neurologic abnormalities include disturbance in sleep
patterns such as insomnia or hypersomnia.
- Neurologic abnormalities seen in more advanced presentations
include asterixis and hyperactive deep tendon reflexes.
- Focal neurologic signs may be detected in some patients during episodes
of hepatic encephalopathy, with hemiplegia being the most common deficit
treatment
- identify and treat precipitating factors such as:
(i) gastrointestinal bleeding,
(ii) infection,
(iii) alkalosis,
(iv) hypokalemia,
(v) sedatives/tranquilizers,
(vi)ingestion of dietary proteins,
(vii) azotemia, and
(viii) progressive hepatic dysfunction
- The mainstay of treatment for hepatic encephalopathy is
lactulose and alteration of gut flora.
- Lactulose, a nonabsorbable disaccharide, should be initiated and titrated to about four bowel movements a
day. Lactulose is metabolized by gut flora, lowering colonic pH and thereby favoring ammonia elimination.
- Enteric flora modification with antibiotics, such as metronidazole or neomycin,
is a second-line treatment, and can be used in combination with lactulose.
- Management also includes supportive measures such as restoring electrolyte
balance, fluid maintenance, aspiration precautions, and rapid sequence
intubation for airway protection in grades 3-4 hepatic encephalopathy.
- Flumazenil has been proposed as a possible therapeutic agent for hepatic
encephalopathy based on the theory that "endogenous benzodiazepines"
may be present in patients with hepatic encephalopathy. Meta-analyses
suggest that flumazenil was associated with a significant improvement
in encephalopathy compared with placebo; however, the benefit was short
term and may have been confined to patients who otherwise had a favorable
prognosis.
fulminant
hepatic
failure
- Fulminant hepatic failure is a clinical syndrome characterized by the rapid onset of hepatic
encephalopathy in conjunction with a marked decline in hepatic synthetic function.
investigation
treatment
criteria for
transplant
in acute
liver failure
complications
(i) urine and serum toxicology screens
(ii) hepatitis serologies.
(iii) ceruloplasmin,
(iv) antinuclear antibodies,
(v) smooth-muscle antibodies,
(vi) serum protein electrophoresis,
(vii) CMV and EBV serology
- Once a patient is diagnosed with fulminant hepatic failure, the patient
should be stabilized and transferred to a liver transplant center
Certain pathogeneses demand immediate specific treatment, including:
- N-acetylcysteine for paracetamol OD
- penicillin for Amanita mushroom poisoning;
-delivery of the infant in acute fatty liver of pregnancy;
- zinc and trientine therapy for Wilson's disease;
- transjugular intrahepatic portosystemic shunt, surgical decompression or
thrombolysis in patients with acute Budd-Chiari; and
- acyclovir in patients with acute liver failure related to herpes virus infection
supportive measures include:
(i) nutrition (amino acids, lipids, glucose, and essential elements),
(ii) electrolyte balance,
(iii) frequent glucose monitoring
(iv) aspiration precautions, and
(v) fluid maintenance.
(i) Hypokalemia, hyponatremia, and hypophosphatemia are common.
(ii) Hypoglycemia, seen in up to 45% of patients with fulminant hepatic failure,
requires aggressive glucose administration, often with 10% dextrose.
(iii) Infection in patients with fulminant hepatic failure is a major
source of mortality, as 44-80% of patients with fulminant hepatic
failure develop bacterial infections.
(iv) Fungal infections are also not uncommon in these patients,
with rates as high as 32% having been reported.
(v) Acute renal failure frequently develops in fulminant hepatic
failure. Renal failure is particularly high in the setting of paracetamol
ingestion, as it can directly damage the kidneys. Once renal failure is
established, it often is irreversible and carries a grave prognosis. Renal
replacement therapy is generally well tolerated and may provide a
bridge to transplant.
(vi) Severe coagulopathy often precedes the evolution of hepatic encephalopathy
to coma. The development of severe coagulopathy is due to the decreased synthesis
of clotting factors II, V, VII, and IX and is manifested by a prolonged prothrombin time.
However, current recommendations are to correct coagulopathy with FFP intravenously
only when overt bleeding occurs or when an invasive procedure is planned. Recombinant
factor VIIa has been shown to be safe and effective in reversing the coagulopathy
in patients with fulminant hepatic failure
(vii) - Cerebral edema is a common complication of fulminant hepatic failure, occurring
in up to 80% of patients with grade IV coma, but requires a high level of clinical suspicion.
Cerebral edema oftenleads to intracranial hypertension and subsequent herniation and death
- Direct intracranial pressure monitoring is recommended in patients suspected of cerebral
edema or intracranial hypertension, with a target intracranial pressure of <20 mm Hg.
Intracranial pressure monitoring is recommended to maintain an adequate cerebral
perfusion pressure of >60 mm Hg.
- Mannitol is first-line therapy for treating cerebral edema and intracranial
hypertension, administered at 0.3-0.4 g/kg body weight. In patients with
renal failure, mannitol may accumulate in astrocytes and cause increased rebound
swelling.
- Thiopental may be used in this setting (250 mg over 15 mins).
- propofol can be used.
- moderate hypothermia to 32-33°C, may be useful in decreasing intracranial pressure
as a bridge to liver transplantation or while transplantation is being performed
Liver transplantation offers the best long-term survival, with an overall
posttransplantation 1-yr survival of about 60%
- Short-term extracorporeal hepatic support for patients with fulminant hepatic
failure may ultimately serve to improve overall survival and provide support as a
bridge to liver transplantation, but it remains experimental (2 types are cell-based
and non-cell based)
Hepatorenal
syndrome
- Hepatorenal syndrome is the development of renal
failure in a patient with advanced liver disease.
- Hepatorenal syndrome is characterized by impaired renal function, abnormalities
in the arterial circulation, and activity of the endogenous vasoactive system
- Divided into two types (type 1 is rapidly progressive; type 2 is slowly progressive)
Epidemiology:
- The prevalence of hepatorenal syndrome in patients with end stage
cirrhosis ranges between 7% and 15%
Risk factors:
(i) Na and H2O retention (indicated by a urinary Na of <5 mEq/L and dilutional hyponatremia),
(ii) low mean arterial blood pressure,
(iii) poor nutrition,
(iv) reduced glomerular filtration rate,
(v) high plasma renin activity, and
(vi) esophageal varices.
Diagnostic criteria:
Treatment:
(i) dialysis
(ii) liver transplant
(iii) TIPS
(iv) iv clonidine has been shown to improve GFR by 25% (oral is ineffective)
(v) midodrine / octreatide / terlipressin
(vi) albumin administration](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-135-320.jpg)
![fungi
[created by
Paul Young
02/10/07]
risk factors
for invasive
Candidaemia
(i) such as recent abdominal surgery,
(ii) gastrointestinal tract perforation,
(iii) dialysis,
(iv) central venous catheterization,
(v) total parenteral nutrition,
(vi) broad-spectrum antibiotic therapy and
(vii) colonization with Candida species
arguments against
prophylaxis with
fluconazole
(i) may predispose to infection or colonization with azole resistant fungal species
(ii) drug interactions with fluconazole
(iii) hepatotoxicity of fluconazole
arguments for
prophylaxis with
fluconazole
- antifungal prophylaxis with fluconazole reduces invasive fungal infections and
total mortality across a broad range of clinical settings in non-neutropenic critically
ill patients in a systematic review.
- Certain Candida species, such as C. glabrata and C. krusei, and most filamentous
fungi, including Aspergillus species, are intrinsically or relatively fluconazole-resistant
- the incidence of candidaemia amongst unselected ICU patients is only 0.5–2%.
- Invasive fungal infections in such patients are associated with crude mortality rates of 30–40%,
Candida spp
- Candida albicans is asexual, dimorphic with hyphae, pseudohyphae & chlamydospores
- Other species with increased resistance patterns and varied morphology are
(i) C. topicalis
(ii) C. krusei
(iii) C. glabrata
(iv) C. lusitanae
(v) C. parapsilopsis
- Azole resistance is increasing with C. albicans and is well establised for C. krusei
& C. glabrata
- amphotericin resistance is a problem with C. lusitanae but it is sensitive to azoles
Cryptococcus
- C. neoformans and C. gattii are the most important
- an encapsulated organism
- cause of meningitis and pneumonia in the immunocompromised
- India ink staining and CSF and blood crytococcal antigen tests are useful
Mucormycosis
- caused by Zygomycetes fungi - Rhizopus, Rhizomucor, Absidia spp
- broad, non-septate hyphae that branch at 90 degrees
- risk factors are:
(i) chronic respiratory acidosis,
(ii) poorly controlled diabetes,
(iii) immunosuppression,
(iv) renal failure,
(v) chelation therapy with increased serum iron levels,
(vi) burns,
(vii) intravenous drug use
- invasive rhinocerebral, orbital or disseminated black lesions
- usually resistant to azoles (except posaconazole)
Aspergillus
fumigatus
- acute angle, branching, septated, non-pigmented hyphae
- associated diseases include:
(i) asthma (type 1 hypersensitivity to spores)
(ii) allergic bronchopulmonary aspergillosis (type 3 hypersensitivity
with recurrent pneumonia & bronchiectasis)
(iii) aspergilloma (mycetoma)
(iv) invasive aspergillosis
- serum galactogamman (an Aspergillus antigen) may aid diagnosis
- CT may show halo and crescent air signs with aspergilloma and
invasive disease
Pneumocystis
jiroveci
- previously known as P. carinii & renamed recently as well as reclassified
as a fungus on the basis of nucleic acid and biochemical features
- classically causes pneumonia in the immunosuppressed
- may respond to treatment with cotrimoxazole, dapsone or atovaquone
- concomitant corticosteroids should be used in patients with HIV infection
and significant hypoxaemia
- Invasive candidiasis is highly likely if:
(i) cultured from the blood (especially two at different times of collection)
(ii) cultured from a sterile site
- Invasive candidiasis is suggested by:
(i) culture from tissue or burn wound biopsies
(ii) culture from two non-contiguous sites
(iii) identified species is non commensal
treatment
of systemic
candidiasis
- For severe sepsis due to Candida species, initiate treatment with amphotericin
until the identity of the Candida species is confirmed.
- If the infection is related to an intravascular catheter, the catheter should be
removed to prevent relapse. Initially, use:
amphotericin B desoxycholate 0.5 to 1 mg/kg IV, daily.
- For proven Candida albicans and other susceptible strains, use:
fluconazole 400 mg (child: 10 mg/kg up to 400 mg) IV, daily.
- Following clinical improvement with either IV amphotericin or IV fluconazole, for
susceptible species, continue treatment with:
fluconazole 400 mg (child: 10 mg/kg up to 400 mg) orally, daily for a total of at least 14 days.
- Some Candida (eg C. krusei, C. glabrata) are resistant to fluconazole; voriconazole or
caspofungin may be suitable alternatives.
- Neutropenic patients with hepatosplenic candidiasis need prolonged therapy](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-136-320.jpg)



![Guillain
Barre
Syndrome
[created by
Paul Young
29/11/07]
general
- aka acute inflammatory demyelinating polyradiculoneuropathy
- typically a motor greater than sensory peripheral neuropathy
with subacute onset, monophasic course and nadir within 4 weeks
aetiology
- precise aetiology is unknown but GBS is immune mediated and
related to antibodies directed against peripheral nerve components
- numerous antecedents have been implicated but the more frequent are:
(i) upper respiratory tract infections
(ii) Campylobacter jejuni enteritis
(iii) CMV infection
(iv) EBV infection
(v) hepatitis A, B and C
(vi) HIV infection
- the association with antecedent infections suggests that certain agents may
elicit immune responses involving antibodies that cross react with peripheral
nerve gangliosides
- most patients suffer a demyelinating neuropathy but in about 5% of cases
the condition is a primary axonopathy
- GM1 antibodies are present in axonal forms of GBS and GQ1b antibodies
are present in the Miller Fisher variant of GBS
clinical
manifestations
- initial findings are usually subacute and progressive weakness that is most marked
in the legs associated with sensory complaints but without objective signs of sensory
dysfunction
- deep tendon reflexes are often significantly reduced or absent at presentation
investigation
CSF:
- typically reveals elevated protein content without pleocytosis
- the nucleated cell count is <10 cells/mm3
- a CSF lymphocytosis of 10-20 cells/mm3 may suggest the possibility of HIV
nerve conduction studies:
- may be normal initially but often reflect segmental nerve demyelination with:
(i) multifocal conduction blocks
(ii) temporally dispersed compound muscle action potentials
(iii) slowed conduction velocity
(iv) prolonged or absent F waves
treatment
general:
- components of treatment for patients with GBS are as follows:
(i) management of ventilatory failure
(ii) management of autonomic dysfunction
(iii) management of painful peripheral neuropathy
(iv) meticulous nursing care
(v) psychologic support
(vi) physical and occupational therapy
(vii) prevention of deep vein thrombosis
(viii) nutritional support
(ix) early planning for rehabilitation
(x) immunotherapy for underlying immune process
imaging:
(i) CT or MRI of c-spine should be considered to exclude a high cervical lesion
respiratory failure:
- patients with GBS and evolving respiratory failure should generally be intubated
when the vital capacity falls to about 15ml/kg or when difficulty with secretions
begins because the recovery is generally slow [suxamethonium should be avoided]
- many patients become too weak to trigger the ventilator requiring mandatory modes
- weaning patients with GBS must wait for adequate strength to return [an improvement in vital
capacity to >15ml/kg and in negative inspiratory force to greater than 25cmH2O usually suggests
that a patient has improved enough to begin weaning; a formula using a combination of ventilatory
and gas exchange variables has also been designed for this purpose]
- the majority of patients require support for less than 4 weeks but as many as 20%
require more than 2 months
autonomic dysfunction:
- treatment of autonomic dysfunction is difficult with marked lability in blood pressure responses
autonomic dysfunction:
- most typically presents as a hypersympathetic state and is often heralded by unexplained
sinue tachycardia; patients may rarely experience bradycardic episodes that require pacing
- blood pressure may fluctuate wildly
- autonomic surges during tracheal suction or due to distended viscus may be dramatic
nursing care:
- similar to care of other paralysed and ventilated patients but particular
care needs to be taken to remember that GBS patients are lucid
- in addition to carefully explaining procedures, arranging distractions
during the daytime and adequate sleep at night is very important
- in concert with physiotherapists, passive exercise should be performed frequently throughout the day
- eye patching may be helpful
- meticulous pressure care is required
DVT prophylaxis:
- a significant danger for patients with GBS requiring DVT prophylaxis
and a low threshold for investigation of potential DVT or PE
nutritional support:
- should begin as soon as the patient is admitted with appropriate concern for the risk of aspiration
- most patients can be nasogastrically fed without difficulty; however, autonomic
neuropathy sometimes complicates feeding
Immunotherapy
- overall, summary is that both plasma exchange and IVIG are effective and equivalent and no
additional benefit is conferred by combined treatment
- patients with heart disease, renal insufficiency, hyperviscosity or IgA deficiency may be more
susceptable to the complications of IVIG whereas labile BP, septicaemia and venous access
problems may preclude plasma exchange
(i) plasma exchange:
- the efficacy of plasma exchange has been reviewed in a Cochrane review of six class II
trials comparing plasma exchange alone with supportive care. Most of the trials employed
up to five plasma exchanges of 50ml/kg over 2 weeks. This metanalysis demonstrated a
more rapid recovery in ventilated patients treated with plasma exchange within 4 weeks of
onset of symptoms
- the optimal number of exchanges has been assessed in patients with mild, moderate and
severe GBS by the French cooperative group. On the basis of this trial, two exchanges are
better than none in mild GBS, four are better than two in moderate GBS and six are no better
than four in severe GBS
- albumin is the preferred replacement fluid
(ii) IVIG
- the efficacy of IVIG has also been examined by Cochrane review with three randomised
controlled trials demonstrating its equivalency with plasma exchange
steroids:
- corticosteroids are not effective in GBS and are therefore not recommended
eye complications:
- corneal ulcers may complicate poor lid closure
painful peripheral neuropathy:
- may be extremely difficult to treat
diagnostic
criteria
diagnostic criteria for typical Guillain Barre Syndrome
1. features required for diagnosis
(i) progressive weakness in both arms and both legs
(ii) areflexia
2. features strongly supportive of the diagnosis
(i) progression over days to 4 weeks
(ii) relative symmetry of symptoms
(iii) mild sensory symptoms or signs
(iv) cranial nerve involvement (particularly bilateral weakness of facial muscles)
(v) recovery beginning 2-4 weeks after progression ceases
(vi) autonomic dysfunction
(vii) absence of fever at onset
(viii) high CSF protein with fever than 10x6cells/L
(ix) typical electrodiagnostic features
3. features excluding diagnosis
(i) botulism, polio, myaesthenia or toxic neuropathy
(ii) abnormal porphyrin metabolism
(iii) recent diptheria
(iv) history or evidence of lead intoxication
(v) pure sensory syndrome without weakness
drugs associated with autonomic instability in GBS](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-140-320.jpg)

![primary critical
care emergencies
related to
haematological
malignancy
general
- With the rapid improvement in chemotherapy and supportive care of hematology
patients, almost all hematologic malignancies are potentially curable in children and
adults with chemotherapy, either alone or in combination with immunotherapy or
radiotherapy and bone marrow transplantation if indicated.
- If the malignancy is not curable, prolonged remission with excellent quality of life is
achievable for most patients.
- Delay in treatment of some aggressive malignancies can greatly jeopardize the chances
of recovery for some acutely ill patients.
clinical
situations
requiring
urgent
chemotherapy
cerebral
leukostasis
pulmonary
leukostasis
CNS
involvement
bulky mediastinal
involvement compressing
vascular structures
disseminated
intravascular
coagulation
severe
hemophagocytic syndrome
- should be suspected in the presence of any alteration of consciousness,
even a simple slowing down of cognitive functions, once an emergency
CT scan has ruled out an intracranial hemorrhage.
- generally observed in hyperleukocytotic leukemias, with circulating blast counts
greater than 30,000 to 50,000/mm3 for acute myeloid leukemia (AML) or
greater than 100,000/mm3 by definition for acute lymphoid leukemia (ALL).
- symptomatic leukostasis is very rare in ALL, even for greatly elevated blasts
counts, because of the smaller size and higher plasticity of these blasts.
leukaemic
infiltration
of the lungs
- Leukemic infiltration of the lungs, which is different from leukostasis,
can occur with low blast counts, and is often associated with AML5.
- Central nervous system (CNS) involvement suspected on the basis of clinical
signs, such as focal deficits, seizures, or any degree of alteration of consciousness
- Bulky mediastinal involvement with vascular compression (superior vena cava
syndrome) or tracheobronchial repercussion, especially as seen in T-cell ALL.
- Threatening disseminated intravascular coagulation (DIC)
with low fibrinogen levels and a prolonged prothrombin time.
- Severe hemophagocytic syndrome, with failure of one or more than one organ.
choice of
cytoreductive
regimen
- The choice of cytoreductive regimen depends on the type of malignancy
- For acute leukemias, efforts should be made to characterize the lineage (ALL or AML)
before treatment is initiated, but if lineage cannot be determined, a non-lineage-specific
cytotoxic regimen should be chosen.
- Intensivists can be confronted with five main situations, depending on whether the
lineage diagnosis has been established:
(i) ALL,
(ii) AML,
(iii) promyelocytic leukemia (AML3),
(iv) acute leukemia of unknown lineage,
(v) non-Hodgkin's lymphoma (NHL), and, very rarely, Hodgkin's disease (HD).
emergency
chemotherapy
in leukaemias
acute
lymphoblastic
leukaemia
acute
promyelocytic
leukemia
acute
myeloid
leukaemia
other than
promyelocytic
leukaemia
acute
leukaemia of
undetermined
lineage
leukaemic
pulmonary
infiltrates
the role of
leukapharesis
- In cases of compressive emergency or high tumor burden, progressive steroid therapy should be
prescribed first (beginning with 0.5 mg/kg prednisone for the first dose); patients with high tumor
burden should be carefully monitored, because they can rapidly develop a severe acute tumor lysis
syndrome (ATLS).
- For patients with increasing or stagnating WBC counts or without biologic indicators of tumor response
for lymphomas (especially increasing lactate dehydrogenase [LDH] levels) after two full doses of steroids,
emergency adjunction of vincristine with or without daunorubicin as early as day 2 is required.
- Classic induction therapy is based on a combination of prednisone, vincristine, and an
anthracycline (daunorubicin in most studies), with or without the addition of cyclophosphamide .
- The main complication of acute promyelocytic leukemia (APL) is DIC, with
early mortality essentially related to hemorrhages located in the CNS.
- Nevertheless, although leukostasis in APL is almost never a problem, because these patients are usually
pancytopenic, their leukemia should be considered (and treated) as hyperleukocytic APL as soon as the WBC
count is higher than 5000/mm3.
- Although APL is remarkably sensitive to anthracyclines, the emergency treatment of APL with
severe coagulation disorder now relies on early administration of all-trans-retinoic acid (ATRA).
- Initial worsening of the DIC is the rule, and patients should receive abundant transfusion
support to ensure a platelet count greater than 50,000/mm3, and at least 1.5 g/L of fibrinogen.
- In hyperleukocytic APL, immediate coadministration of ATRA with daunorubicin is required, starting with half the
usual dose (20 to 25 mg/m2/day) for at least 4 days, because transient exacerbation of DIC is almost universal.
- Urgent induction is derived from the classic reference treatment, a combination of 3 days of an anthracycline
(classically daunorubicin, but idarubicin is one of the many possible alternatives), with 7 days of cytarabine .
- The difference is that the scheme of administration is progressive
- In cases in which the lineage cannot be determined (e.g., no specialized cytologist on duty, poorly differentiated
leukemia requiring complementary immunohistochemical study) and the patient requires urgent chemotherapy, then
daunorubicin should be chosen, because of its activity on all types of blasts (AML or ALL).
- Acute respiratory failure revealing a leukemia is rare, but intensivists should be aware that respiratory
failure with bilateral consolidation can reveal nonhyperleukocytic monocytic leukemias (AML5).
- This condition should be recognized promptly, because it appears to be associated with
a high risk of rapid respiratory deterioration after initiation of chemotherapy.
- The induction treatment is based on low-dose daunorubicin alone (20 to 25 mg/m2/day)
for 2 to 3 days, followed by the introduction of cytarabine .
- Aggressive supportive care should be initiated in case of respiratory deterioration, because
50% of these patients can survive these difficult inductions.
- Therapeutic leukapheresis has been reported to be of benefit for patients with AML who have
high WBC counts, and it is routinely used in some centers for acute hyperleukocytic leukemia.
- However, controversial data have been published, and the results suggest that, despite a
potential reduction in early mortality, there is no overall improvement on long-term survival.
emergency
treatment of
lymphoma
non-Hodgkins
lymphoma
Burkitt's
lymphoma
Hodgins
lymphoma
- Emergency initiation of chemotherapy in non-Hodgkin's lymphomas (NHLs) can be
necessary in the following clinical situations:
1. Massive pleural or pulmonary involvement compromising hematosis
2. Bulky mediastinal tumor with compression of trachea or main bronchi
3. Poorly tolerated superior vena cava syndrome
4. CNS localization with alteration of consciousness
5. Spinal cord compression
6. Airway compromise in case of pharyngeal localization
7. Pericardial or cardiac involvement
8. Occlusive syndrome in massive abdominal tumors
9. NHL-related severe hemophagocytic syndrome
- In these cases, initiation of chemotherapy may be required before exhaustive assessment
of the disease has been completed, or even before definitive typing of the lymphoma has
been established, thus complicating the therapeutic choices.
- Nevertheless, most of these life-threatening complications occur in the setting of
aggressive, large cell lymphomas, and the important point is not to choose the optimal
protocol for a specific NHL but to be efficient in ensuring survival with limited toxicity
in these patients with compromised respiratory, cardiac, renal, or hepatic functions.
- All of these patients should receive adequate preventive treatment for ATLS, and they
should be closely monitored for the occurrence of this syndrome during the first 3 days.
- With the exception of confirmed or suspected Burkitt's lymphomas (which require
smaller doses of steroids on day 1), treatment of bulky NHLs should be started with
steroids at 1 mg/kg/day of methylprednisolone or equivalent on day 1 and completed as
early as day 2 with vincristine (1 mg/m2 once, maximum total dose 2 mg, in the absence
of severe preexisting peripheral neuropathy) and cyclophosphamide (500 to 700 mg/m2)
on day 2 in the absence of uncontrolled ATLS
- The risk of an overwhelming ATLS is so high in patients with Burkitt's lymphomas that
steroids alone should be administered first and in increasing doses.
- Most protocols recommend that known or suspected Burkitt's lymphomas with high
tumor burden be treated with a cytoreductive course of chemotherapy, before full-dose
chemotherapy is administered.
- Emergency chemotherapy is a rare necessity in HD, but life-threatening mediastinal
or cardiac involvement is possible, compromising oxygenation or hemodynamic stability.
- Nevertheless, one should remember that HD is a slow-responding tumor, so no spectacular
reduction of tumor burden should be expected within 24 or 48 hours after the initiation of
chemotherapy, and decisions regarding supportive care should take into account this
parameter.
CNS involvement:
- Patients with NHL of the CNS who display focal deficits, alterations of the level of
consciousness, or seizures should receive emergency steroid therapy with at least 2
mg/kg/day of methylprednisolone or equivalent.
- The optimal dosing is controversial in the literature, and doses ranging from 2 to 4
mg/kg/day can be considered as appropriate.
- Administration of high-dose methotrexate, a key drug in the treatment of CNS NHL, is
not necessary in an emergency situation
severe
hemophagocytic
syndrome
- Severe hemophagocytic syndrome is now well recognized as a common presenting feature in NHL and HD.
- In many cases, the organ failures are related to the intensity of the histiocytic activation and not to the
aggressivity of the lymphoma itself, which can have a very low tumor burden, making the etiologic diagnosis
all the more difficult.
- The clinical course of these patients is generally fulminant, especially once ICU admission is required.
The clinical presentation is confounding-it precisely mimics a septic shock, with fever, chills, vasoplegic
shock, acute respiratory distress syndrome, and oliguric renal failure-but severe pancytopenia, high blood
transfusion requirements, organomegaly, lymph node enlargement, and hepatic dysfunction days or weeks
before the occurrence of this pseudo-septic shock should suggest the diagnosis of severe hemophagocytic syndrome.
- The clinical course of these patients is generally fulminant, especially once ICU admission is required.
The clinical presentation is confounding-it precisely mimics a septic shock, with fever, chills, vasoplegic
shock, acute respiratory distress syndrome, and oliguric renal failure-but severe pancytopenia, high blood
transfusion requirements, organomegaly, lymph node enlargement, and hepatic dysfunction several days
or weeks before the occurrence of this pseudo-septic shock should suggest the diagnosis of severe
hemophagocytic syndrome.
management
of severe DIC
- Supportive care is essential in DIC and should include repeated platelet transfusions to reach a minimum
platelet count greater than 50,000/mm3 permanently; correction of the prothrombin time and of hypofibrinogenemia
with fresh-frozen plasma (2 to 4 units to start with) to ensure a prothrombin time less than 2.5 times normal; and a
fibrinogen level greater than 1 g/L before the start of the treatment.
- The use of low-dose unfractionated heparin (100 IU/kg/day) is controversial, requires platelet counts
permanently superior to 50,000/mm3, and cannot be recommended for patients with active bleeding.
- As soon as appropriate transfusion support is initiated, chemotherapy should be started,
always with progressive dosing, to reduce the leukemic load as quickly as possible.
- Transient worsening of the DIC is common and justifies the intensification of
transfusions as required by biologic and clinical manifestations.
- In uncontrolled and life-threatening bleeding in nonhematology patients, the adjunctive use of recombinant factor VIIa has
yielded some response, but this treatment has never been evaluated in the peculiar case of hematologic malignancies
hyperviscosity
syndromes
Hyperviscosity syndromes may be encountered in multiple myeloma and Waldenström's
macroglobulinemia, symptomatic forms being more common in the latter.
- Clinical manifestations are mainly neurologic (headaches, alteration or slowdown of cognitive function, stupor,
even coma, and rarely seizures), ocular (visual impairment, papillary edema with dilated retinal veins, retinal
hemorrhages), and excessive bleeding (mainly mucosal, cutaneous, and retinal).
- Emergency management is directed at rapidly decreasing blood viscosity through
plasmapheresis, which leads to rapid alleviation of the initial symptoms.
- Plasmapheresis is the only therapeutic option with immediate efficacy; it consists of the exchange of
1 to 1.5 plasma volumes (5 L maximum), with 100% replacement by 4% human albumin solution
- Long-term management, whether based on high-dose steroids or chemotherapy, is aimed at reducing the production
of the monoclonal immunoglobulin and can be postponed until a hematologist consultant has been reached
blastic
meningitis
- Although prophylactic intrathecal chemotherapy is required in all patients with ALL or hyperleukocytic AML,
very few patients require urgent intrathecal chemotherapy (coma, seizures, cauda equina syndromes).
- lumbar puncture, even for exploratory purposes, is contraindicated in patients with hyperleukocytosis, to prevent
any seeding of the cerebrospinal fluid with blasts during the procedure, and in those patients with marked DIC.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-142-320.jpg)

![haemodynamic
monitoring
[created by
Paul Young
16/10/07]
pulmonary
artery
catheter
Measured values:
cardiac output: 4-8L/min
cardiac index: 2.5-4L/min
CVP: 2-6mmHg
PAOP: 8-12mmHg
PAP: 25/10mmHg
SVO2: 0.65-0.70
Derived values
stroke volume: 50-100ml/beat
stroke volume index: 25-45ml/beat/m2
SVR 900-1300 dynes-sec/cm5
SVRI 1900-2400 dynes-sec/cm5
PVR 40-150 dynes-sec/cm5
PVRI 120-200 dynes-sec/cm5
Evidence
- Randomized studies have not shown a positive effect of PAC
- The timing of monitoring and intervention in the era of PAC may also explain the inconsistency
of the results. In the critically ill patient with multi-organ failure, intervention is not as efficacious
as in earlier stages of illness, probably because of more advanced pathophysiological processes.
Additional considerations:
- The use of PAC is also complicated by the invasiveness of the procedure and potential complications.
Oesophageal
Doppler
General:
- A Doppler probe in the mid-oesophagus, is used to measure the velocity of blood in the
descending aorta. This velocity can be transformed to a corresponding SV by a nomogram
derived from correlation studies with PAC measurements.
Measured values:
- blood velocity
Derived values:
- OD derived stroke volume and cardiac output
- systolic flow time, which may indicate systemic vascular resistance. The normal range of the
systolic flow time is 330-360 ms and, with lower values, hypovolaemia should be suspected
Evidence:
- early validation studies showed good agreement with thermodilution techniques; however,
it is now known that the agreement is poor when upper / lower body blood flow distributions are
altered or when estimates of aortic cross sectional area are inaccurate
Additional Considerations:
- OD does not require calibration
- relatively little training is needed to provide a reproducible result.
- The position of the probe, however, must be accurate and adjustments are required frequently.
Values for SV and CO must therefore be interpreted with attention to the probe position.
- requires a sedated patient
- contraindicated in oesophageal pathology, aortic balloon counterpulsation & severe coarctation
- unreliable in children due to large fluctuations in aortic cross-sectional area during systole
- assumptions that descending aorta is 70% of cardiac output can be incorrect
PICCO
General:
- The pulse contour cardiac output method (PiCCO) is the most validated system
in pulse contour analysis and correlates with PAC thermodilution measurements
Direct Measurements
- Pulse pressure
Derived Measurements
- Stroke volume
- Cardiac output
Evidence:
- comparisons with PA catether cardiac output measurement has shown good
agreement
Additional Considerations:
- results in patients with arrhythmia may be unreliable because of the irregular
arterial waveforms
- PiCCO is calibrated by transpulmonary thermodilution and is therefore invasive,
as, in addition to a central venous catheter, it requires a femoral or axillary artery
line.
- recalibration is advisable every few hours to allow for changes in SVR
(esp during haemodynamic instability or infusion of vasoactive drugs)
Lithium
Dilution
Cardiac
Output
General:
- LiDCO is a monitor that uses pulse power analysis.
- requires arterial and venous lines
Additional Considerations:
- It requires initial calibration, either by a small lithium
bolus or a value of CO attained with another monitor.
- The amount of lithium used to calibrate the system has not been associated with any reported
side-effects. However, there is interference with non-depolarizing neuromuscular blockers
so that calibration with lithium must take place before or 15-30 min after their administration
- LiDCO has been reported to be contraindicated in patients weighing less than 40 kg,
in the first trimester of pregnancy and in patients on lithium therapy.
- corrections for packed cell volume are necessary since lithium is only distributed in plasma
- blood is toxic after assay in the lithium sensitive electrode and must be disguarded
Measured Values:
Derived Values:
Evidence:
- Measurements with LiDCO suggest a comparable accuracy to PiCCO, and reports
propose comparable precision to CO determined by thermodilution.
- Reports on the clinical application of LiDCO are limited
Model
Flow
General:
- Model Flow estimates beat-to-beat SV and CO by an arterial line or a non-
invasive finger pressure using a non-linear three-component model of arterial impedance.
Additional Considerations:
- MF is easy to install and requires minimal technical skills.
- The cuff used to measure finger pressure is unreliable under circumstances
in which the patient develops peripheral vasoconstriction
Evidence:
- Changes in SV measured with MF have been validated against other
modalities but have not been validated in studies of outcome
Derived values:
- absolute values of SV and CO can be obtained in a clinical setting by calibrating
against a monitor that provides an absolute value for stroke volume.
Measured values:
- model flow stroke volume and cardiac output
central
venous
oxygen
sats
Evidence:
- The use of Scvo2 rather than Svo2 is argued by studies showing consistently higher values of
Scvo2 than Svo2 of approximately 5%, but with parallel changes in response to a volume load
- Svo2 value of more than 70% forms part of the strategy of'early goal-directed therapy' in sepsis
which has been shown to improve outcome
Mixed
venous
oxygen
sats
near-infrared
spectroscopy
- Near-infrared spectroscopy (NIRS) facilitates the estimation of oxygenation within tissue. By the use of
an optode placed on the skin, near-infrared light is sent through the tissue and the reflected light is used
to estimate oxygenation.
gastric
tonometry
General
- The gastric tonometer is used for the evaluation of perfusion to the splanchnic bed. Reduced perfusion
and resulting ischaemia are registered by changes in the pH of the gastric mucosa using a probe. A
decreased pH of the gastric mucosa is associated with a poorer outcome
- during splanchnic hypoperfusioni, intramuscosal PCO2 increases and intramuscosal pH is reduced.
echocardiography
General:
- echocardiography visualizes the real-time anatomy and physiology of the heart
Evidence:
- Fluid therapy guided by echocardiography has not been evaluated in an outcome study
Additional considerations:
- requires expert personnel and training
General:
- measured from superior vena cava via a central line
- ScvO2 is <SvO2 because it contains predominantly SVC blood which is lower than IVC blood
other data generated from monitoring device:
(i) CVP
situations where ScvO2 > SvO2
(i) anaesthesia - because of increase in CBF and depression of metabolism
(ii) patients with head injury where cerebral metabolism is depressed
(iii) shock - because of diversion of blood from splanchnic circulation, there
is increased oxygen extraction & therefore IVC saturation decreases
General:
- measured from a pulmonary artery catheter
- more invasive than ScvO2
- SvO2 is > ScvO2 as it contains blood from both SVC and IVC
Evidence:
- Gattinoni RCT showed no benefit from SvO2 monitoring
Other data generated from monitoring devices:
- see PAC
pros
& cons of
continuous
intraarterial
PaO2
monitoring
Direct measurements:
- SvO2 (a value of 0.5 corresponds to the theoretical critical
PvO2 of 26mmHg below which tissue dysoxia is highly likely; values exceeding 0.8 are highly
suggestive of high flow states such as sepsis, hyperthyroidism and severe liver disease)
Derived measurements:
- mixed venous oxygen content can be used to determine Qs/Qt (venous admixture),
VQI (simplified venous admixture) & VO2I (oxygen consumption index) [the latter of
these is CI x (CaO2-CvO2)x10]
Evidence:
(i) low intramuscosal pH (pHi) has been linked with bleeding from stress ulcers,
weaning failure, post-traumatic ARDS trauma, morbidity after liver transplant,
major complications after cardiac surgery, MODS & death
(ii) there is no convincing evidence that titrating therapy to pHi or CO2 gap improves outcome
Additional considerations:
(i) there is uncertainty about the true dysoxic threshold (current
recommendations are to maintain the CO2 gap <25mmHg)
(ii) regional PCO2 is insensitive to tissue dysoxia if blood flow is preserved](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-144-320.jpg)






![HIV
[created by
Paul Young
02/10/07]
general
PCP
Hep C
immune
reconstitution
syndromes
toxic
effects
of HAART
management
of prophylaxis
and HAART
in critically
ill patients
outcomes
CXR changes
associated
with HIV
- AIDS is a worldwide epidemic with greater than 20 million deaths
worldwide by the end of 2004, and three million deaths in 2004 alone
- In the last 10 yrs, our perception of HIV infection and AIDS has changed
from an almost uniformly fatal disease into a manageable chronic illness
with introduction of HAART
- A few studies indicate that in the era of HAART, ICU admissions for PCP
have declined, and overall outcomes seem to be improved. Respiratory
failure is still the commonest reason for admission to ICU
General:
- Pneumonia caused by Pneumocystis jiroveci (formerly classified Pneumocystis
carinii) has always been a major cause of illness and death in patients with HIV infection.
- Once thought to be a parasite, genomic analysis revealed that P. jiroveci is in fact a
fungus that infects only humans, whereas P. carinii is pathogenic only in immunodeficient rats.
Diagnosis:
- The diagnosis of PCP is established by identification of the organism in specimens obtained
from the respiratory tract, either in sputum induced by inhalation of hypertonic saline or by
bronchoscopy
Treatment:
- Trimethoprim-sulfamethoxazole is the preferred treatment for PCP
in patients who have not had an adverse reaction to this drug
- Patients with severe PCP who do not respond or who are intolerant of this medication are
usually given pentamidine, although this drug is associated with more adverse reactions
- Gas exchange typically deteriorates during the first few days of anti-Pneumocystis
therapy when corticosteroids are not given; corticosteroids may attenuate lung injury
caused by the inflammatory response to killed organisms, allowing the patient to survive
to receive more antimicrobial therapy
Prognosis:
- Before the availability of HAART, patients who survived
mechanical ventilatory support for PCP rarely lived for >1 yr.
- With the use of HAART, the prospects for long term survival are considerably
more hopeful, especially if the patient has not yet received antiretroviral therapy
- HIV infected persons tend to have more severe liver disease and liver-
associated mortality than HCV-infected persons without HIV disease.
- Death rates from HCV increased after the introduction of HAART, and the prevalence of
HCV-associated cirrhosis is four times higher in patients with HIV infection compared with
HIV seronegative persons
- It seems that impaired cellular immunity from HIV infection leads to accelerated HCV
reproduction, with an eight-fold increase in HCV replication in HIV-infected persons
compared with HIV-seronegative persons.
- HCV also accelerates the progression of HIV disease
- Management of co-infection with HIV and HCV should include agents active against both
viruses, but the timing and optimal combinations present problems related to
pharmacodynamics and toxicity.
General:
- When HAART inhibits viral replication, there is a corresponding increase in the population
of memory and naïve T cells, enhancement of lymphoproliferative responses, increased
interleukin-2 receptor expression, and reduced production of some plasma cytokines
- These proinflammatory effects underlie newly recognized syndromes associated with immunologic reconstitution
Diagnostic Criteria:
1. the diagnosis of AIDS,
2. treatment with anti-HIV medications, symptoms consistent with an infectious
or inflammatory condition that occurred while receiving antiretroviral therapy
3. symptoms that cannot be explained by a newly acquired infection or
by the expected clinical course of the disease or side effects of therapy.
Clinical features:
- In the lung, some patients develop a granulomatous disorder that resembles sarcoidosis, whereas
others with latent or active mycobacterial infection may develop fever, lymphadenopathy, and
opacities on the chest radiograph 2–8 wks after starting treatment with HAART
- IRIS has also been described after or during infection with Mycobacterium avium complex, cryptococcosis,
cytomegalovirus,herpes zoster, hepatitis B and C viruses, and the agent that causes progressive multifocal
leukoencephalopathy.
Treatment:
- discontinuation of HAART, reintroduction of corticosteroids, or both.
General:
- HAART may carry the risk of life-threatening toxicities that prompt admission to the ICU
Protease Inhibitors:
- can cause pancreatitis [very rare], which may be severe.
- Protease inhibitors also cause a syndrome of lipodystrophy, insulin resistance, and hyperlipidemia
Nucleoside reverse transcriptase inhibitors:
- may cause lactic acidosis by disrupting mitochondrial DNA replication by selective inhibition of DNA polymerase.
- Mild hyperlactemia occurs commonly; severe lactic acidosis occurs at a rate
of 1.3 cases per 1,000 person years of nucleoside exposure and may be life threatening
- If severe hyperlactemia or lactic acidosis is found, then the nucleoside analog reverse transcriptase
inhibitor should be stopped immediately, and standard supportive care should be given.
- Because patients may also develop severe lactic acidosis due to sepsis, empirical
antibiotics are administered pending the results of a bacteriologic evaluation.
Abacavir:
- is a nucleoside analog that is used in HAART regimens.
- associated with hypersensitivity reactions within a few weeks of treatment in around 3% of patients, and
rechallenge often leads to life-threatening anaphylaxis. The initial hypersensitivity reaction is characterized
by fever, chills, nausea, diarrhea, and rash. The rash is not always present, sometimes misleading
the clinician into diagnosing an infection
When to start prophylaxis:
- If an HIV-infected patient develops a critical illness, prophylaxis against opportunistic
pathogens like P. carinii should be started or continued unless it is otherwise indicated
When to start HAART:
- the decision to start HAART during critical illness or a severe infection
is problematic. Proponents of early institution of HAART, even in critically ill patients,
hold that prompt treatment of underlying HIV infection is the most important
determinant of long-term survival and that an improved immune system would facilitate
the resolution of an active infection.
- these drugs are often difficult to administer to critically ill patients. Only zidovudine
is available in an intravenous preparation
- All of the antiretrovirals may have significant interactions with other medications
that may be used to treat the critical illness, and drugs may impose new toxicities
in patients not well enough to withstand them.
- immune reconstitution after antiretroviral therapy may lead to a new life-threatening
accelerated inflammatory response to active or resolving infection, as in the cases of
respiratory failure after institution of HAART in patients recovering from PCP
- most clinicians defer starting HAART until the acute illness has resolved or improved significantly.
- Patients already receiving HAART should continue to receive these drugs whenever
possible, as discontinuing therapy is associated with viral replication and the emergence
of resistance.
- it seems that critically ill patients with HIV infection have similar short-
term outcomes as other patients with a comparable severity of illness
HIV
drugs
progression
of illness
mucocutaneous
infections in HIV](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-151-320.jpg)
![hormonal
reponse
to critical
illness
[created
by Paul
Young
03/12/07]
general
- Critical illness is characterized by a uniform dysregulation of all hypothalamic- anterior pituitary axes,
long known to contribute to the high risk for morbidity and mortality. It is now clear that the neuro-
endocrine responses to acute and prolonged critical illness are substantially different.
- In the acute phase of critical illness, the pituitary is secreting actively, but target organs become resistant
and concentrations of most peripheral effector hormones are low. These acute adaptations probably are
beneficial in the struggle for short-term survival,for which no need for intervention seems necessary.
- In contrast, prolonged, intensive care-dependent critical illness is hallmarked by a uniform
suppression of the neuroendocrine axes, predominantly of hypothalamic origin,which contributes to
the low serum levels of the respective target-organ hormones. These chronic alterations no longer
may be beneficial, as they participate in the general wasting syndrome of prolonged critical illness.
thyroid
axis
General
- Thyrotropin-releasing hormone (TRH), secreted by the hypothalamus, stimulates the pituitary thyrotropes to
produce thyrotropin, which in turn regulates the synthesis and secretion of thyroid hormones in the thyroid gland.
- Thyroid hormones are essential for the regulation of energy metabolism and have profound effects on
differentiation and growth. Although the thyroid gland predominantly produces thyroxine (T4), the biologic
activity of thyroid hormones is exerted largely by triiodothyronine (T3)
The acute phase of critical illness
- The early response of the thyroid axis after the onset of severe physical stress consists of a rapid decline in the
circulating levels of T3 and a rise in rT3 levels, predominantly because of altered peripheral conversion of T4.
- Thyrotropin and T4 levels are elevated briefly but subsequently normalize, although in those who are
more severely ill, T4 levels also may decrease.
- Although serum thyrotropin levels measured in a single daytime sample are normal in acute critical
illness, the thyrotropin profile already is affected, as the normal nocturnal thyrotropin surge is absent.
- The low T3 levels persist beyond thyrotropin normalization, a condition referred to as ''the low T3
syndrome.'' The decrease in circulating T3 during the first 24 hours after an insult reflects the severity
of illness. Furthermore, T3 levels correlate inversely with mortality.
The prolonged phase of critical illness
- Patients who need prolonged intensive care show, in addition to the absent nocturnal thyrotropin surge, a dramatically
reduced pulsatile thyrotropin secretion. Furthermore, serum levels of T4 and T3 are low, and in particular, the decline in
T3 correlates positively with the diminished pulsatile release of thyrotropin. The prognostic value of the disturbed thyroid
axis with regard to mortality is illustrated by lower thyrotropin, T4, and T3 and higher rT3 levels in patients who ultimately
die compared with those who survive prolonged critical illness.
- In the chronic phase of critical illness, the peripheral metabolism of thyroid hormone also is disturbed and contributes
to the low T3 syndrome. Regulation of thyroid hormone action at the level of the thyroid hormone receptor also seems
to be altered by critical illness, possibly causing an upregulated thyroid hormone sensitivity in response to low T3 levels.
gonadal
and
lactotropic
axis
somatotrophic
axis
general
- Gonadotropin-releasing hormone (GnRH), secreted in a pulsatile pattern by the
hypothalamus, stimulates the release of luteinizing hormone (LH) and follicle-stimulating
hormone (FSH) from the gonadotropes in the pituitary.
- In women, LH mediates androgen production by the ovary, whereas FSH stimulates the
aromatization of androgens to estrogens in the ovary.
- In men, LH stimulates androgen production by Leydig's cells in the testes, whereas the
combined action of FSH and testosterone on Sertoli's cells supports spermatogenesis.
- Prolactin (PRL) is a well-known stress hormone produced by the lactotropes in the
pituitary, which is physiologically secreted in a pulsatile and diurnal pattern, and is
presumed to have immune-enhancing properties. Physiologic control of PRL secretion
largely is under the control of dopamine, but several other PRL-inhibiting and -releasing
factors can modulate PRL secretion
The acute phase of critical illness
- Acute physical stress, such as surgery or myocardial infarction, brings along an
immediate fall in the serum levels of testosterone, even though LH levels are elevated.
This suggests an immediate suppression of androgen production Leydig's cells, which
may be viewed, at least in the short term, as an attempt to reduce energy consumption and
conserve substratesfor more vital functions. Involvement of cytokines again is possible,
as put forward by experimental studies.
- PRL levels rise in response to acute physical or psychologic stress. Factors possibly
involved are vasoactive intestinal peptide, oxytocin, and dopaminergic pathways, but
again cytokines or as yet uncharacterized factors also may play a role.
- The rise in PRL levels after acute stress is believed to contribute to the vital activation
of the immune system early in the disease process, but this remains speculative.
The prolonged phase of critical illness
- More dramatic changes develop within the male gonadal axis with prolongation of the
disease, and hypogonadotropism ensues. The circulating levels of testosterone become
extremely low and often even are undetectable, in the presence of suppressed mean LH
concentrations and pulsatile LH release.
- Total estradiol levels also are relatively low but the level of bioavailable estradiol
probably is maintained in view of the simultaneous decrease in sex-hormone-binding
globulin. Alternatively, a remarkable rise in estrogen levels is observed in other studies
- As testosterone is the most important endogenous anabolic steroid, the abnormalities in
the gonadal axis could be important with regard to the catabolic state of critical illness.
- The pulsatile fraction of PRL release becomes suppressed in patients in the prolonged
phase of critical illness. It is unclear whether or not the blunted PRL secretion contributes
to the immune suppression or increased susceptibility to infection associated with
prolonged critical illness
General
- Growth hormone (GH) is secreted by the somatotropes in the pituitary and is essential
for linear growth during childhood but serves many more important functions throughout life.
- The regulation of the physiologic pulsatile release of GH, consisting of peak serum GH
levels alternating with virtually undetectable troughs, is important for its metabolic effects
- Hypothalamic GH-releasing hormone (GHRH) stimulates, and somatostatin inhibits, the
secretion of GH.
- GH exerts direct and indirect effects, the latter mediated by insulin-like growth factor-I (IGF-I)
The acute phase of critical illness
- During the first hours to days after an acute insult, the GH profile changes dramatically.
The pulse frequency is increased, peak GH levels are elevated, and interpulse concentrations
are high.
- Concomitantly, a state of peripheral GH resistance develops, triggered in part by
cytokines, such as tumor necrosis factor a and interleukin 6.
- Despite the clearly enhanced GH secretion, serum concentrations of IGF-I decrease
- Theoretically, this may enhance the direct lipolytic and insulin- antagonizing effects of
GH, resulting in elevated fatty acid and glucose levels in the circulation, whereas indirect,
IGF-I-mediated somatotropic effects of GH are attenuated. As a result, costly anabolism,
largely mediated by IGF-I is decreased during the struggle for survival.
The prolonged phase of critical illness
- In prolonged critically ill patients, when recovery does not occur within a few days, a
different GH secretion pattern arises.
- The pulsatile release of GH becomes suppressed, whereas the nonpulsatile fraction of
GH release remains somewhat elevated. A strong positive correlation is found between
the pulsatile fraction of GH release and circulating IGF-I levels, which suggests that the
loss of pulsatile GH release contributes to the low levels of IGF-I in prolonged critical
illness.
- This chronic GH deficiency, resulting from lack of pulsatile GH secretion, could
contribute to the pathogenesis of the wasting syndrome that characterizes prolonged
critical illness.
adrenal
axis
General
- The hypothalamic corticotropin-releasing hormone (CRH) controls the pituitary corticotropes
for release of corticotropin, which stimulates the adrenal cortex to produce cortisol.
- In stress-free healthy humans, cortisol is secreted according to a diurnal pattern and exerts a negative feedback
control on both hormones. More than 90% of circulating cortisol is bound to binding proteins, predominantly
corticosteroid-binding globulin (CBG) but also albumin; however, only the free hormone is biologically active.
The acute phase of critical illness
- In the early phase of critical illness, cortisol levels usually rise in response to an increased
release of CRH and corticotropin, but the diurnal variation in cortisol secretion is lost.
- Cortisol production and glucocorticoid receptor number or affinity are modulated by cytokines in acute illness.
- Stress-induced hypercortisolism in critically ill patients fosters the acute provision of energy by shifting
carbohydrate, fat, and protein metabolism; protects against excessive inflammation by suppression of the
inflammatory response; and improves the hemodynamic status by induction of fluid retention and sensitization
of the vasopressor response to catecholamines.
The prolonged phase of critical illness
- Cortisol levels usually remain elevated in the chronic phase of critical illness, which seems to
be driven by non-corticotropin-mediated pathways, because corticotropin levels are decreased.
- Cortisol levels slowly decrease, only reaching normal levels in the recovery phase. CBG levels recover
in the chronic phase of illness. Whether or not the persisting elevation in cortisol is beneficial exclusively
in prolonged critical illness remains uncertain. Theoretically, it could contribute to the increased susceptibility
to infectious complications. Alternatively, the risk for ''relative adrenal failure'' may increase in the chronic phase
of critical illness and may predispose to adverse outcome
therapeutic
implications
- Administration of pharmacologic doses of GH, inspired by the assumption of sustained
GH resistance in the prolonged phase of critical illness, unexpectedly increases morbidity
and mortality.
- Initial trials studying administration of high doses of glucocorticoids clearly show that
this strategy is ineffective and perhaps even harmful. In contrast, studies using still
supraphysiologic low-dose glucocorticoid replacement therapy for relative adrenal
insufficiency report beneficial effects, at least in patients who have septic shock.
- It remains controversial whether or not administration of thyroid hormone to patients
who are critically ill is beneficial or harmful
- There is no conclusive clinical benefit demonstrated for androgen treatment in
prolonged critical illness
overview](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-152-320.jpg)



![hyperkalaemia
treatments
[created by
Paul Young
17/12/07]
protecting
the heart
Calcium chloride.
- Although there are no clinical studies assessing the efficacy of calcium
salts in the emergency management of hyperkalaemia, there remains little
doubt of their importance in emergency management even in patients with
normal serum calcium.
- Both calcium salts, calcium chloride and calcium gluconate, antagonise
the cardiac membrane excitability and have been widely recommended for
the treatment and prophylaxis of arrhythmias due to hyperkalaemia when life
threatening ECG changes (absent P waves, wide QRS, sine-wave pattern)
are present or when cardiac arrest occurs.
- The decision of which calcium salt should be used, chloride or gluconate,
is largely guided by practicalities such as availability and local practice.
Calcium chloride contains more calcium (6.8 mmol in 10 ml) than calcium
gluconate (2.2 mmol in 10 ml) and has greater bioavailability, but is more
likely to cause tissue injury if extravasation occurs.
Efficacy:
- calcium chloride and calcium gluconate do not lower serum potassium.
Cautions:
- known or suspected digoxin toxicity. Rate of administration should be slower
(over 30 min) in patients taking digoxin as calcium salts may contribute to toxicity.
Adverse effects:
- bradycardia, arrhythmias, tissue necrosis if extravasation occurs.
summary
of
medications
used
shifting of
potassium
into cells
(i) Insulin-glucose therapy.
- Several studies have evaluated the efficacy of insulin with
glucose for the treatment of hyperkalaemia. Insulin enhances
cellular uptake of potassium by stimulating the sodium-potassium
(Na-K) adenosine triphosphatase (ATP) pump. This effect is
independent of its effect on cellular glucose uptake.
- Administration of glucose without insulin is not recommended in
non-diabetics as endogenous insulin release may be insufficient
and paradoxically could increase serum potassium further.
- Efficacy: insulin reduces potassium by 0.65-1 mmol/l within 60
min of administration.
- Cautions: regular (soluble) insulin should be used.
- Adverse effects: hypoglycaemia. This may be delayed (30-60 min
post-infusion) if less than 30 g glucose is given.
(ii) Sodium bicarbonate.
- Sodium bicarbonate decreases the concentration of H+ in the
extracellular fluid compartment which increases intracellular Na+ via
the Na+/H+ exchanger and facilitates K+ shift into cells via the
Na-K-ATPase pump. However, bicarbonate does not lower serum
potassium in the absence of metabolic acidosis.
- Efficacy: no study has shown an independent potassium lowering
effect within 60 min but when used in combination with insulin-
glucose or salbutamol, it lowered potassium by 0.47±0.31 mmol/l at 30 min.
- Cautions: calcium salts and sodium bicarbonate should not be
administered simultaneously via the same route to avoid precipitation
of calcium carbonate.
- Adverse effects: hypernatraemia; pulmonary oedema due to large
sodium load; tetany in patients with coexistent hypocalcaemia.
(iii) Salbutamol.
- Beta agonists have been widely studied for the treatment of hyperkalaemia.
Salbutamol binds to beta-2 receptors stimulating adenylase cyclase which
converts ATP to cAMP. This results in stimulation of the Na-K ATP pump and
intracellular potassium uptake.
- Efficacy: salbutamol lowers serum potassium by 0.87-1.4 mmol/l after iv
administration and by 0.53-0.98 mmol/l after administration in the nebulised
form. The response is dependent on the dose administered as greater efficacy
was reported in patients receiving 20 mg versus 10 mg of nebulised salbutamol.
- It is important to note that beta-blockers may affect the response to treatment
and up to 40% of patients with ESRF do not respond to salbutamol.
- Cautions: beta-agonists may exacerbate tachycardia in patients with tachyarrhythmias.
- Adverse effects: tachycardia, tremor, anxiety and flushing.
removing
potassium
from the
body
(i) Exchange resins.
- Cation exchange resins are cross-linked polymers with negatively charged structural units which exchange calcium
(calcium resonium) or sodium (sodium polystyrene sulphonate; Kayexalate) for potassium across the intestinal wall.
- Efficacy: resins do not appear to increase faecal potassium excretion above the effect of induction of diarrhoea with
laxatives. Studies have reported no reduction in serum potassium at 4 h
- Cautions: slow acting, therefore unsuitable for urgent management of hyperkalaemia. Coadministration
of laxative is recommended.
Adverse effects: constipation, intestinal necrosis.
(ii) Diuretics.
- The theoretical basis for the use of diuretics in the treatment of hyperkalaemia is to enhance urinary potassium
excretion. However, there are no clinical trials to support their use in the treatment of hyperkalaemia.
(iii) Intravenous fluids.
- Although there is no clinical trial to support fluid replacement, it is advisable to administer 0.9% saline intravenously if there is
clinical evidence of volume depletion with the aim of improving renal perfusion and enhancing urinary potassium excretion.
(iv) Dialysis.
- Dialysis is the most immediate and reliable way of removing potassium from the body.The principle mechanism of action is the
diffusion of potassium across the transmembrane gradient. Haemodialysis can remove 25-40 mmol/h of potassium and is more
effective than peritoneal dialysis.
- The typical decline in serum potassium is 1 mmol/l in the first 60 min, followed by 1 mmol/l over next 2 h. The efficacy of
haemodialysis in lowering serum potassium can be improved by performing dialysis with a low potassium concentration in the
dialysate, a high blood flow rate or a high dialysate bicarbonate concentration.
medical
interventions in
hyperkalaemic
cardiac arrest
- When hyperkalaemia is suspected to be the primary precipitant of cardiac arrest, resuscitation should not be terminated
until serum potassium is controlled, by any means necessary, unless there are extenuating circumstances.
- Hyperkalaemia may also arise during the resuscitation attempt as a result of metabolic changes and hypoxia but does
not usually require specific intervention.
- During CPR, adrenaline (epinephrine) should be the first drug to be administered irrespective of the cause of cardiac
arrest. Adrenaline is a powerful sympathomimetic amine with both alpha- and beta adrenergic activity which helps to
drive potassium into cells, thereby lowering serum potassium.
- Next, calcium chloride should be administered to antagonise the toxic effects of hyperkalaemia.
- Sodium bicarbonate should be considered in the context of a metabolic acidosis.
- Insulin-glucose is thought to be ineffective during CPR, however it is unlikely to cause harm and should begin to have
effect within minutes of return of spontaneous circulation.
- There is no literature available on the use of intravenous salbutamol in this scenario.
- Optimising ventilation during CPR can avoid compounding acidosis and further extracellular shift of potassium.
haemodialysis during resuscitation
- There are several reports of patients treated successfully with dialysis during CPR for cardiac arrest
secondary to hyperkalaemia. In many of these reports, resuscitation combined with dialysis has been
successful even after prolonged CPR (in excess of 90 min) with no neurological sequelae. The dialysis
mode used was dependent on local availability and practice, but success has been reported with haemodialysis,
veno-venous haemofiltration or veno-venous haemodiafiltration, and also with peritoneal dialysis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-156-320.jpg)
![hyperkalaemia
[created by
Paul Young
17/12/07]
causes
ECG
changes
emergency
management
general
- Hyperkalaemia is the most common electrolyte disorder associated with potentially life-
threatening arrhythmias and cardiopulmonary arrest.
- It is defined as a serum potassium concentration above 5.0 mmol/l2 and may be classified
as mild (K 5.0-5.9 mmol/l), moderate (K 6.0-6.4 mmol/l) or severe (K=6.5 mmol/l).
- A potassium concentration above 10.0 mmol/l is usually fatal unless emergency treatment is
readily instituted, however survival with extreme hyperkalaemia (K 14 mmol/l) has been reported.
symptoms
- Patients may present with weakness progressing to flaccid paralysis, paraesthesia, depressed deep
tendon reflexes or respiratory difficulties. However, the absence of these symptoms should not lead
to a false sense of security if the clinical history suggests a high risk of an electrolyte disturbance.
arrhythmias
(i) Bradycardia.
- Bradycardia is an ominous complication of hyperkalaemia and these patients pose several dilemmas. Firstly, there is no widely
available guidance for the use of calcium salts for bradycardia induced by hyperkalaemia. As bradycardia is listed as a potential
adverse effect of calcium salts, there may be reluctance to use calcium salts even in the context of severe hyperkalaemia.
- the response to atropine is usually poor and temporary pacing may be considered although there is some evidence to suggest
a reduced efficacy of temporary pacing in this setting
- A universal recommendation is difficult in the face of little evidence, but haemodialysis usually resolves the bradycardia without
the need for cardiac intervention.
(ii) Asytole.
- The outcome of asystolic cardiac arrest due to hyperkalaemia is usually fatal unless the serum potassium can be returned to
normal. Despite this, there are several reports of successful resuscitation in patients presenting with or developing asystole as
a result of severe hyperkalaemia. Dialysis was necessary during the course of cardiopulmonary resuscitation (CPR) in most of
these cases to lower the serum potassium.
(iii) Ventricular tachycardia.
- Ventricular tachycardia (VT) is a recognised manifestation of hyperkalaemia but it is more commonly reported in association with
hypokalaemia. It has also been suggested that the presence of a broad complex tachycardia induced by hyperkalaemia may be
misinterpreted as VT instead of a sine-wave pattern.
(iv) Ventricular fibrillation.
- Ventricular fibrillation (VF) is often presented as the natural transition from a sine-wave pattern in the presence of extreme
hyperkalaemia (K > 8.0 mmol/l). Analogous to resuscitation for hypothermia, it is important to recognise that defibrillation is
frequently unsuccessful until the serum potassium is controlled and CPR should be prolonged.
(v) Pulseless electrical activity (PEA).
- Any electrolyte disorder may present as PEA, including hyperkalaemia. There are few reports in the literature of successful
resuscitation with PEA as the presenting rhythm of cardiac arrest. In each case, prolonged resuscitation was required.
pseudohyperkalaemia
- Pseudohyperkalaemia, also known as spurious hyperkalaemia, is defined as
a difference between serum and plasma potassium greater than 0.4 mmol/l.
- It should be suspected in patients with hyperviscosity syndromes such as polycythemia rubra
vera, in the absence of ECG changes despite severe hyperkalaemia and when sample storage
has been prolonged or inadequate.
- rarely pseudohyperkalaemia may occur due to malposition of the arterial cannula resulting in a
high shear rate and haemolysis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-157-320.jpg)
![hypernatraemia
[created by Paul
Young 15/12/07]
aetiology
treatment
general
- hypernatremia can be induced by several illnesses in the critical care setting.
- Hypernatremia is generally categorized according to the causal factors involved:
(i) hypervolemic,
(ii) hypodipsic, and
(iii) increased free water losses
Hypodipsic
hypernatremia
- Decreased water intake, or hypodipsia, probably represents the leading
cause of hyperosmolality encountered in intensive care settings.
- Outside of critical care settings this etiology is particularly prevalent among
the elderly or patients who have altered mental status who do not respond
appropriately to physiologic stimuli that signal increased thirst
Hypernatremia
from increased
water losses
- A variety of diseases can cause increased free water losses in the critical care setting, including
gastrointestinal water losses, intrinsic renal disease, hypercalcemia, hypokalemia, and solute
diuresis and glucosuria.
- Although these etiologies represent the most frequent causes of hypernatremia with critical
illnesses, they must be differentiated from diabetes insipidus, which represents the quintessential
clinical cause of hypernatremia.
- Generally, a urine osmolality less than 800 mOsm/kg H2O in the setting of elevated serum
osmolality is indicative of a renal concentrating defect. In the absence of glucosuria or other
causes of osmotic diuresis, this generally reflects the presence of diabetes insipidus.
Central diabetes insipidus
- Central diabetes insipidus is caused by a deficiency of AVP secretion from
the posterior pituitary but does not become fully manifest until more than
85% of the magnocellular AVP-secreting neurons are damaged.
- Central diabetes insipidus is rare, with a prevalence of 1:25,000. Most cases (40% to
50%) are secondary to a hypothalamic lesion, such as a tumor, or infiltrative
diseases such as sarcoidosis and histiocytosis.
- Approximately 20% to 30% of central diabetes insipidus is categorized as idiopathic, but
most of these patients most likely have underlying autoimmune disease.
- Sellar lesions and pituitary adenomas are not a common cause of diabetes insipidus, because,
over time, the secretion of AVP from magnocellular neurons can shift to regions higher in the
hypothalamus. Because these lesions are typically slow growing, if a sellar lesion is detected in
the setting of new-onset diabetes insipidus, this suggests the presence of a rapidly enlarging
sellar mass such as metastatic disease.
Nephrogenic diabetes insipidus
- Nephrogenic diabetes insipidus is caused by end-organ resistance of the kidney to the
antidiuretic effects of AVP. Whereas familial or hereditary nephrogenic diabetes insipidus is
secondary to mutations of the AVP V2 receptor or the AQP2 water channel, acquired nephrogenic
diabetes insipidus is caused by hypercalcemia, hypokalemia or medications such as lithium and
demeclocycline.
Distinguishing central and nephrogenic DI
- A plasma AVP level is useful to distinguish central diabetes insipidus from nephrogenic diabetes
insipidus; however, to differentiate definitively nephrogenic diabetes insipidus from central
diabetes insipidus and from normal individuals with primary polydipsia, performance of a water
deprivation test is often necessary.
- Treatment goals of hypernatremia include correcting the established
water deficit and reducing ongoing excessive urine water losses.
- The following formula is used to estimate the pre-existing water deficit:
- This formula assumes that total body water is 60% of body
weight and does not take ongoing water losses into account.
- The treatment of central diabetes insipidus with DDAVP is an effective means of improving polyuria
and hypernatremia. Initial doses in the acutesetting are 1 to 2 mcg (intravenous, intramuscular, or subcutaneous).
- If hypernatremia in the setting of central DI, free water should also be given in an effort to correct
serum sodium, with 5% dextrose in water as the preferred intravenous replacement fluid.
- Although some cases of nephrogenic diabetes insipidus respond to large doses of DDAVP,traditionally,
nephrogenic diabetes insipidus is treated with sodium restriction and thiazide diuretics (any drug in this class may be
used with equal potential for benefit), which block sodium absorption and act to decrease renal diluting capacity and
free water clearance.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-158-320.jpg)
![hyperphosphataemia
[created by Paul
Young 17/12/07]
causes
(i) renal failure
- most common cause
- causes hyperphosphataemia because the renal excretion by
the kidneys is impaired
- serum phosphate is usually normal until the creatinine clearance
is less than 30ml/min
(ii) increased renal resorption
- hypoparathyroidism
- thyrotoxicosis
(iii) cellular injury with release of phosphate
- tumour lysis syndrome
- rhabdomyolysis
- haemolysis
(iv) medication related
- abuse of phosphate containing laxatives
- excessive phosphate administration
- bisphosphonate therapy
manifestations
- most manifestations are due to associated hypocalcaemia which is produced by
(i) precipitation with calcium (leading to nepholithiasis)
(ii) interference with parathyroid hormone-mediated resorption of bone
(iii) decreased vitamin D levels
- manifestations of hypocalcaemia include muscle cramping, tetany,
hyperreflexia and seizures as well as cardiovascular manifestations
treatment
(i) limit phosphate intake
(ii) enhance urinary phosphate excretion
- in the absence of end stage renal disease, phosphate excretion
can be optimised with saline infusion and diuretics
- diuretics that work on the proximal tubule such as acetazolamide
are particularly effective for enhancing phosphate excretion
- any patient with life threatening hyperphosphataemia should receive dialysis
(iii) oral phosphate binders
- calcium and aluminium salts are widely used; however calcium salts may produce
metastatic calcification and aluminium salts are toxic.
- in dialysis patients, chronic management with calcium free phosphate binders such
as sevelamer hydrochloride may reduce long-term mortality by preventing long-term
cardiovascular complications associated with a high calcium phosphorus product
NB: in the acute management of patients with hyperphosphataemia accompanied
by hypocalcaemia, the likelihood and clinical significance of metastatic calcification
with acute calcium administration is unclear](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-159-320.jpg)
![hypertensive
emergencies
in pregnancy
[created by
Paul Young
09/10/07]
general
- Development of hypertensive disorders is the most common medical complication
during pregnancy, affecting 10% to 20% of all pregnancies worldwide.
- Causes include:
(i) pregnancy-induced hypertension
(ii) preeclampsia,
(iii) eclampsia, and
(iv) hemolysis, elevated liver enzyme levels, low platelet count (HELLP) syndrome.
preeclampsia
& eclampsia
Pathogenesis of preeclampsia
- Several factors seem to contribute to the development of preeclampsia, including
defective trophoblast invasion of the spiral arteries and abnormal trophoblast
differentiation.
risk factors:
(i) Preeclampsia during previous pregnancy
(ii) Advanced maternal age
(iii) Multiple pregnancies
(iv) High body-mass index
(v) Conception before age 20
(vi) Connective tissue disorders
(vii) Protein C and protein S deficiencies
(viii) Factor V Leiden mutation
(ix) Hyperhomocysteinemia
clinical features:
- Development of new-onset hypertension (systolic BP >140 mm Hg or
diastolic BP >90 mm Hg) during the third trimester or late second trimester
in a previously normotensive pregnant woman is the first sign of preeclampsia.
- Development of proteinuria (>300 mg/24 hours) usually follows.
- Preeclampsia may present with unusual clinical manifestations. Transient cortical
blindness, frequent headaches, and transient scotomata may occur
laboratory features:
- The serum creatinine measurement may be within normal laboratory range,
because the preeclampsia-induced decrease in filtration fraction is compensated by
the pregnancy-induced increase in glomerular filtration rate.
- Hyperuricemia and hypocalciuria also may accompany preeclampsia.
- Consumption of platelets in microcoagulation, resulting in thrombocytopenia
is a frequent feature of preeclampsia. The prothrombin time, partial thromboplastin,
time and fibrinogen concentration are unaffected by preeclampsia, unless complicated
by abruption placentae or severe hepatic involvement.
treatment:
- The definitive therapy for preeclampsia is delivery of the fetus.
- The use of antihypertensive agents to control mildly elevated systolic BP
in preeclampsia has not been shown to alter the course of maternal disease;
however, there is a general consensus, that systolic BP of at least
160mmHg and diastolic BP of at least 105 mm Hg should warrant initiation
of antihypertensive therapy.
- Prolonged antenatal therapy with methyldopa has stood the test of time.
Calcium-channel blockers also have been used as long-term therapy with
increasing confidence.
- Peripartum acute hypertensive episodes should be treated with intravenous
hydralazine or lobetalol. The goal is to lower systolic BP to approximately
140 to 150 mm Hg and diastolic BP to about 90 to 100 mm Hg
- Magnesium sulfate (MgSO4) is the preferred drug for preventing seizures.
- The safety and efficacy of MgSO4 have been demonstrated in the MAGPIE
trial, in which 10,000 pregnant women with BP of at least 140/90 mm Hg
and proteinuria of at least 1+ were treated with intramuscular MgSO4 or placebo.
Major findings include the following:
(1) a significantly reduced risk for convulsions in MgSO4 recipients,
regardless of the severity of preeclampsia, gestational age, or parity; and
(2) a trend toward decreased maternal mortality rates
HELLP
syndrome
general:
- characteristics of HELLP are:
(i) microangiopathic haemolytic anaemia
(ii) elevated liver function tests (AST, ALT, LDH)
(iii) low platelets
(iv) normal APTT, PT and fibrinogen
- HELLP syndrome should not be considered a variant of disseminated intravascular
coagulation (DIC), even though microangiopathic hemolytic anemia is
the hallmark of both conditions. Important differences exist between HELLP
syndrome and DIC. Prothrombin time, partial thromboplastin time, and
serum fibrinogen levels are normal in HELLP syndrome, whereas these parameters
are usually abnormal in DIC.
- Immunoflorescence studies usually reveal fibrin microthombi and fibrinogen
deposits in necrotic and normal hepatic sinusoids.
clinical manifestations:
- No clinical signs or symptoms are unique to HELLP syndrome.
- Epigastric pain and right upper quadrant pain are the most common symptoms.
Significant weight gain and generalized edema are the most prominent signs.
- Severe hypertension is not a universal finding.
- Occasionally, patients may present with polyuria caused by nephrogenous DI.
differential diagnosis:
(i) Acute fatty liver of pregnancy
(ii) Acute cholecystitis
(iii) Hemolytic uremic syndrome
(iv) Thrombotic thrombocytopenic purpura
(v) Perforating peptic ulcer
(vi) Acute pyelonephritis
(vii) Hepatic encephalopathy
(viii) Acute viral hepatitis
treatment:
- Diagnosis of HELLP syndrome should be considered a serious complication of
pregnancy. Patients should be admitted to monitored beds in the hospital.
- Administration of intravenous corticosteroids is associated with rapid
improvement of laboratory and clinical parameters in some patients after
delivery. Although the results are less dramatic, intravenous corticosteroid
use before delivery may be beneficial.
- Plasma exchange after delivery has been used in patients with persistent
HELLP syndrome and end-organ damage with variable response.
complications:
- HELLP syndrome is associated with several complications (eg, abruption
placentae [16%], acute renal failure [8%], subcapsular hematoma of liver [1%])
clinical features of severe preeclampsia
diagnostic criteria for pre-eclampsia
magnesium dosage in eclampsia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-160-320.jpg)

![hypoglycaemia
[created by
Paul Young
04/12/07]
general
- Hypoglycemia always constitutes an emergency because it signals an inability of the central nervous system (CNS)
to meet its energy needs. Resultant mental status impairment places the patient and others at risk for accidents
and traumatic injury. Left untreated, hypoglycemia can result in permanent neurologic damage and death.
- The definition proposed by Whipple in 1938 is still the most useful and defines pathologic hypoglycemia as a triad
of low plasma glucose, hypoglycemic symptoms, and resolution of symptoms with correction of the blood sugar
manifestations
- Symptoms caused by a sudden drop in blood glucose are associated with increased autonomic nervous
system outflow (adrenergic and cholinergic symptoms) and include anxiety, tremulousness, palpitation,
sweating, nausea, and hunger.
- Hypoglycemia is also commonly associated with symptoms of compromised CNS function because
of brain glucose deprivation (neuroglycopenic symptoms). Symptoms include weakness, fatigue, confusion,
seizures, focal neurologic deficit, and coma.
pathophysiology
- Conceptually, hypoglycemia results from an absolute or relative imbalance
between the rate of glucose appearance and disappearance from the circulation
- Excess glucose utilization by peripheral tissues favors disappearance and usually results from a
circulating insulin concentration inappropriate for the level of glycemia. In rare cases, however,
it may be caused by antibodies or incompletely processed insulin-like growth factors (IGFs) that
act on insulin receptors.
- Increased glucose metabolism by tissues as seen in intense exercise, weight loss, sepsis, or
pregnancy also favors disappearance of circulating glucose and can lead to hypoglycemia
if circulating glucose can not be replenished as quickly as it is used (eg, compromised endogenous
glucose production).
- The rate of glucose appearance is determined by oral intake of substrate and, in the fasting state,
by the rate of endogenous glucose production (eg, glycogenolysis, gluconeogenesis). In the fasting
adult, diseases associated predominantly with compromised endogenous glucose production include
malnutrition, liver failure, renal failure, endocrine deficiencies, and enzymatic defects in glycometabolic
pathways (eg, congenital [glucose-6- phosphatase deficiency] or acquired [ethanol, unripened ackee
fruit]).
predisposing
factors
- Although there are many conditions that can predispose to hypoglycemia, it is most often observed
in those treated for diabetes. Because of the high prevalence of diabetes in the population, hypoglycemia
is the most frequently encountered endocrine emergency in the ambulatory and inpatient care settings.
- In the Diabetes Control and Complications Trial (DCCT), an estimated 10% to 30% of type1 diabetes
patients experienced one hypoglycemic episode requiring third-party assistance for treatment per year.
Previous hypoglycemic episodes, lower glycosylated hemoglobin levels, and intensive therapy predicted
hypoglycemic events in this population.
- In the first 10 years of the United Kingdom Prospective Diabetes Study (UKPDS), hypoglycemic episodes
requiring third-party intervention occurred at an incidence of 1.2% for type 2 patients treated with insulin. More
recent studies suggest an incidence of severe hypoglycemia in type 2 diabetes approximating that of type 1
diabetes.
- In the nondiabetic hospitalized patient, the risk of developing hypoglycemia is associated with malnutrition,
malignancy, renal disease, congestive heart failure, and sepsis.
organ
failure
1. Liver disease
- The liver, through glycogenolysis and gluconeogenesis, supplies most of the glucose to the circulation in the fasting state. The normal
liver has a large functional reserve, and it is estimated that as little as 20% residual functionwould suffice to prevent hypoglycemia.
- This large reserve likely accounts for the fact that most patients with liver disease never develop hypoglycemia. Liver diseases most
commonly associated with hypoglycemia include hepatocellular carcinoma and fulminant hepatitis caused by hepatotoxic agents or viruses.
- Genetic defects in glycometabolic pathways can also lead to hypoglycemia as a consequence
of deficient hepatic glycogenolysis and gluconeogenesis, and most are diagnosed in childhood.
- Finally, liver dysfunction can contribute to hypoglycemia through compromised drug metabolism (eg, tolbutamide, glyburide, glipizide).
2. Renal disease
- The kidney is second only to the liver as a gluconeogenic organ. Factors associated with renal disease that predispose to hypoglycemia
include caloric deprivation from anorexia, vomiting, or protein restriction; depletion of gluconeogenic substrate from the latter or
hemodialysis treatment; use of glucose-free dialysate; and decreased clearance of renally excreted drugs or their metabolites (eg, insulin,
chlorpropamide, metabolite of glyburide).
autoimmune
causes
1. Anti-insulin receptor antibody
- Rarely, hypoglycemia is caused by autoantibodies that bind the insulin receptor and mimic the biologic action
of insulin. Most patients with this syndrome have an antecedent diagnosis of autoimmune disease.
- In some patients, an elevated erythrocyte sedimentation rate or positive anti-nuclear
antibody titer may be the only finding suggestive of an autoimmune cause.
2. Anti-insulin antibody
- Development of hypoglycemia has also been associated with autoantibodies directed against insulin itself. These antibodies
bind free circulating plasma insulin when its concentration is high and release insulin when the concentration of free plasma insulin
drops. Release of insulin at inappropriate times can cause hypoglycemia. Hypoglycemia in this setting
is typically observed in the postprandial period, but fasting hypoglycemia has been reported.
investigation
History
- The history frames the clinical context (eg, liver failure, sepsis, autoimmune disease, neoplasm,
no past health problems) and should be reviewed for a potential drug etiology (including ethanol).
- The history also may provide important clues to suggest dispensing error as a cause of
the hypoglycemia (eg, onset of hypoglycemia after a recent refill).
- Biochemical tests to assess for potential liver, renal, adrenal, and anterior pituitary dysfunction should be obtained.
(i) hormone levels
- Growth hormone and cortisol levels in the normal range at the time of hypoglycemia are not uncommon, especially if the problem
has been long-standing. Hormonal deficiency as a cause should be established in the usual manner (eg, cosyntropin or insulin tolerance test).
(ii) hypoglycaemic agents
- Blood and urine should be screened for the presence of hypoglycemic agents to rule out surreptitious use.
- If positive, the screen should be repeated to rule out the presence of interfering substances.
(iii) insulin antibodies
- The presence of insulin antibodies usually suggests that the patient has received insulin by injection but may represent autoantibodies
against insulin in rare cases. The current highly purified insulin preparations used for the treatment of diabetes are less immunogenic
than in the past. Thus, the absence of insulin antibodies does not reliably exclude surreptitious injection of insulin
(iv) plasma insulin & proinsulin
- If the initial evaluation fails to reveal a cause for the hypoglycemia, the possibility of insulinoma should next be
considered. Several different approaches to demonstrate the presence of an insulinoma exist, but the most
useful is the 48-hour supervised fast with measurement of plasma insulin and proinsulin.
- Demonstrating abnormal insulin suppression at the time the patient develops fasting hypoglycemia establishes the diagnosis
of insulinoma. This test is based on the premise that insulin secretion in normal b cells is suppressed, before the onset of
symptoms, when the plasma glucose level reaches 2mmol/L. In contrast, the threshold for insulin suppression in
insulinoma may be absent or shifted to a lower plasma glucose level and symptoms may arise before insulin suppression.
- Thus, a plasma insulin level that fails to suppress to less than 6 microIU/mL at the time of hypoglycemia strongly
suggests the presence of an insulin-secreting tumor, whereas a plasma insulin level that suppresses to less than
6 microIU/mL favors another etiology.
- The sensitivity of this test is not 100%; in rare cases, suppression of plasma insulin
levels to less than 5 microIU/mL is seen in patients with an insulin-secreting tumor.
(v) C-peptide levels
- Measurement of the plasma C-peptide level at the time of hypoglycemia is useful to diagnose patients injecting insulin
surreptitiously. The distinguishing biochemical features in these patients are low C-peptide levels accompanied by high
insulin levels. A similar pattern may be seen in patients with autoantibodies directed against the insulin receptor.
- In these patients, antibodies interfere with insulin binding to its receptor, thereby affecting its clearance from the
circulation. Because C-peptide clearance is unaffected, these patients can present with elevated insulin levels and
low C-peptide levels.
(vi) Insulin-like growth factor-II levels
- It has been suggested that at least 50% of non-islet-cell tumors that cause hypoglycemia produce incompletely
processed IGF-II (Big IGF-II) and that IGF-II is directly responsible for causing hypoglycemia.
- The correlation between circulating IGF-II levels and IGF-II hypoglycemic activity is complex. The interaction
between circulating IGF-II and specific binding proteins is believed to determine IGF-II hypoglycemic activity.
- Protein profiles that permit egress of IGF-II from the circulation and allow tissue entry are postulated to result in hypoglycemia.
Measurement of circulating IGF-II levels in isolation is thus not a useful routine diagnostic test.
therapy
- The first priority in treating hypoglycemia is to administer glucose replacement is necessary.
- The second priority is to address the underlying cause. Examples of interventions include removal or adjustment of the offending drug,
appropriate hormone replacement for patients with deficiency, or confrontation and psychiatry referral for patients with a factitious disorder.
- In the case of insulinoma, resection of the tumor is usually curative. For nonresectable
malignant insulinoma, diazoxide may provide some benefit.
- Hypoglycemia resulting from non-islet-cell tumors is usually treated by interventions aimed at reducing tumor
burden. If this cannot be achieved, glucose administration is the only therapy.
-The syndrome of autoantibodies against the insulin receptor can result in severe hypoglycemia, which is associated
with high mortality if left untreated. This disorder is usually a self-limited condition that resolves over months in most
cases. Therapy consisting of high-dose glucocorticoid (prednisone, 60 mg/d) prevents hypoglycemia by inhibiting the
insulinomimetic effect of the antireceptor antibody but does not hasten its disappearance from plasma.
neoplasm
1. Non-islet-cell tumors
- Mesenchymal tumors, hepatocellular carcinoma, adrenocortical tumors, carcinoid tumors, leukemia, and lymphomas are the tumors
most commonly associated with hypoglycemia. These tumors cause hypoglycemia by secreting a factor with insulin-like action that
is chemically distinct from insulin
- An incompletely processed IGF-II molecule, termed Big IGF-II, with decreased affinity
to IGF-binding proteins has been established as the cause of hypoglycemia in some tumors.
- Finally, ectopic insulin secretion from tumors is a rare phenomenon. Although sporadic case reports
exist in the literature, few reports have conclusively excluded the possibility of a concomitant insulinoma.
2. Insulinoma
- Pancreatic b-cell tumors are rare and can cause hypoglycemia by secreting insulin
autonomously. Most of these tumors are small, solitary, and benign (<10% are malignant)
- The central defect is an inability of insulinoma cells to suppress insulin secretion appropriately in response to a decreasing
circulating glucose concentration. This relative excess of insulin in relation to glucose leads to fasting hypoglycemia.
- Although development of hypoglycemia in the postprandial period does not rule out the presence of an insulinoma,
a negative supervised fast does, because virtually all patients with insulinomas develop hypoglycemia after a 48-hour
supervised fast. Thus, demonstrating fasting hypoglycemia is essential for the diagnosis of insulinoma
3. Islet hyperplasia
- In adults, a variety of histologic patterns in islets have been linked to hypoglycemia. This condition has been called
nesidioblastosis or diffuse islet hyperplasia or the syndrome of noninsulinoma pancreatogenous hyperinsulinism.
drug-
induced
hypoglycaemia
1. Insulin
- Insulin-induced hypoglycemia usually occurs in patients with diabetes treated with insulin.
- Factors to consider in assessing hypoglycemia in a patient with diabetes include:
(i) errors in the type, dose, or timing of insulin injection;
(ii) failure to account for changes in nutrition affecting the peripheral action (eg, weight
loss, exercise) or clearance of insulin (eg, renal failure); and
(iii) altered counterregulation as a result of underlying disease or drugs (eg, beta blockers).
- Some patients with psychiatric illness inject insulin surreptitiously, thereby inducing hypoglycemia. These patients have usually
acquired their familiarity with insulin through a relative with insulin-treated diabetes or through employment as a health care worker.
2. Sulfonylurea
- As with insulin, sulfonylurea-associated hypoglycemia can occur as a result of
volitional or inadvertent overdose, surreptitious use, or criminally intended administration.
- Risk factors associated with an inadvertent overdose in a patient taking sulfonylurea to treat diabetes include
(i) advanced age,
(ii) drug-drug interaction, and
(iii) decreased renal (eg, chlorpropamide) or hepatic clearance (eg, tolbutamide, glipizide, glyburide)
- Accidental overdoses can also occur in patients unknowingly taking sulfonylurea as a result of dispensing error.
3. Ethanol
- Ethanol inhibits gluconeogenesis. This phenomenon has been attributed to consumption
of a rate-limiting cofactor required for gluconeogenesis as a result of ethanol metabolism.
- Ethanol-induced hypoglycemia occurs after glycogen stores have been depleted (12-72
hours), when levels of circulating glucose reflect de novo synthesis from an alternate substrate.
- Ethanol levels in plasma may be normal or no longer detectable at the time of hypoglycemia.
- Hypoglycemia should be excluded before attributing impaired cognition to inebriation in the setting of ethanol ingestion.
4. Other drugs
- Many other drugs have been reported to cause hypoglycemia. High-dose salicylates, beta-blockers, and sulfa-based drugs
are commonly implicated. Pentamidine at doses used to treat Pneumocystis carinii pneumonia can also cause hypoglycemia.
Quinine and antiarrhythmics (eg, quinidine, disopyramide) have been associated with hypoglycemia. Quinolone antibiotics
(eg, gatifloxacin, levofloxacin) have received recent attention for their propensity to cause dysglycemia. Increased insulin
secretion is postulated as the underlying mechanism behind pentamidine, quinine derivatives (including quinolones),
and antiarrhythmic- induced hypoglycemia.
endocrinopathies
- Deficiencies in cortisol and growth hormone have been causally linked to hypoglycemia. Although these hormones do not play
a major role in the recovery from acute hypoglycemia, they play an important role in long-term support of counterregulation
by contributing to gluconeogenesis
- Pituitary disease that results in combined corticotropin and growth hormone
deficiency particularly predisposes to the development of hypoglycemia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-162-320.jpg)

![hyponatraemia
[created by
Paul Young
16/12/07]
hypoosmolar
hyponatraemia
evaluation
general
- Hyponatremia is a common electrolyte abnormality that varies greatly in its clinical presentation. It has
been estimated that approximately 1% of hospitalised patients have acute symptomatic hyponatremia.
- The incidence of hyponatremia (<134 mmol/L) in the intensive care unit was prospectively found to be approximately
30%. The in-hospital mortality ratefor critical care patients with hyponatremia approaches 40%, and hyponatremia
has been shown to be an independent predictor of mortality in the intensive care unit.
- Hyponatremia is generally categorized based on serum tonicity as isotonic, hypotonic, or hypertonic. Although most instances
of hyponatremia in critical illness are associated with hypotonicity, isotonic and hypertonic hyponatremia are also well documented
general
- Hypotonic hyponatremia can occur as a result of solute depletion, a primary decrease in total body solute (often with
secondary water retention), or solute dilution, a primary increase in total body water (often with secondary solute depletion)
- Hypotonic or hypoosmolar hyponatremia is generally subdivided according to the clinical ECF volume status. A recent
retrospective analysis found the relative distributions of the types of hypotonic hyponatremia in the intensive care setting to
be 24% hypervolemic, 26% hypovolemic, and 50% euvolemic.
Hypovolemic hypoosmolar hyponatremia
- Simultaneous water and sodium loss results in ECF volume depletion, with secondary AVP secretion and decreased free water excretion.
Retention of water from ingested or infused fluids can then lead to the development of hyponatremia. Primary solute depletion can occur
via renal or extrarenal sodium losses, each of which can have multiple etiologies.
- Virtually all disorders of solute depletion are accompanied by some degree of secondary retention of water by the kidneys in response to the
resulting intravascular hypovolemia. This mechanism can lead to hypoosmolality even when the solute depletion occurs via hypotonic or isotonic
body fluid losses. Disorders of water retention can cause hypoosmolality in the absence of any solute losses, but, often, some secondary solute
losses occur in response to the resulting intravascular hypervolemia, which can further aggravate the dilutional hypoosmolality.
1. Extrarenal solute losses
- Vomiting, diarrhea, hemorrhage, and excessive sweating all cause extrarenal losses of sodium and potassium, and the fluid loss that
accompanies the solute losses is a potent stimulus to AVP secretion.
- Hyponatremia in hypovolemic shock secondary to volume loss (from hemorrhage or gastrointestinal free water losses) or distributive
shock (secondary to sepsis in which there is a relative hypovolemia from vasodilatation) is characterized by a urine sodium concentration
(UNa) generally less than 10 mmol/L, reflecting appropriate nephron function to maximize sodium reabsorption and to conserve
body solute and ECF volume.
2. Renal solute losses
- Diuretics, mineralocorticoid deficiency, and nephropathies are all important etiologies of renal sodium loss that can lead to the
development of hypovolemic hyponatremia.
- In patients on diuretics, hypokalemia from kaliuresis can worsen hyponatremia by causing a net movement of sodium intracellularly.
- Thiazides are more commonly associated with severe hyponatremia than are loop diuretics such as furosemide.
- Renal solute loss is characterized by high urine sodium excretion, typically UNa >20 mmol/L, despite the existence
of degrees of volume depletion that would normally activate mechanisms causing renal sodium conservation.
Isotonic
hyponatremia
- Isotonic hyponatremia is usually synonymous with so-called ''pseudohyponatremia''
- Plasma osmolality can be measured directly in the laboratory by osmometry or osmolarity can be calculated based on the following formula:
Calculated osmolarity = (2 x [Na+]) + [glucose] + [urea]
- Normal serum is typically comprised of 93% water and 7% nonaqueous factors, including lipids and proteins. Although the
nonaqueous components do not affect serum tonicity, in states of marked hyperproteinemia or hyperlipidemia (typically, elevated
chylomicrons or triglycerides), the nonaqueous proportion of serum is relatively increased with respect to the aqueous portion,
artifactually decreasing the concentration of Na/L of serum although the concentration of Na/L of serum water is unchanged.
hypertonic
hyponatremia
- Hypertonic hyponatremia has also been termed translocational hyponatremia
because the presence of osmotically active particles in the plasma induces
an osmotic movement of water from the ICF to the ECF, decreasing serum
sodium even though serum osmolality remains elevated. Solutes such as
glucose, mannitol, sorbitol, or radiocontrast agents all exert this effect.
Corrected Na+ for glucose = [glucose 3] + apparent sodium
Euvolemic hypoosmolar hyponatremia
- Virtually any disease state causing hypoosmolality can present with what appears to be a normal hydration status based on the usual
methods of ECF volume assessment.
- Clinical evaluation of volume status is not sensitive, whereas laboratory measures such as normal or low urea and uric acid
concentrations and an elevated UNa are useful correlates of normal ECF volume.
- SIADH is the most common cause of euvolemic hyponatremia in critical illness.
Hypervolemic hypoosmolar hyponatremia
- In hypervolemic hyponatremia, there is an excess in total body water and total body sodium, resulting in clinically evident edema
or ascites; however, in many cases, the increase in total body water is out of proportion to that of total body sodium, causing hyponatremia.
- Congestive heart failure, cirrhosis, and nephrotic syndrome all share this common pathophysiology, although the specific
mechanisms vary among these different disease states.
treatment
General
- The symptom severity of hyponatremia depends in large part upon the
rapidity of the decrease in serum sodium. Most patients are not symptomatic
until the serum sodium decreases to less than 125 mmol/L.
- Symptoms are predominantly neurologic, including nausea, vomiting, headache,
fatigue, irritability, and disorientation. Severe hyponatremia can progress to seizures,
brainstem herniation, and death.
- The initial evaluation of patients in the critical care setting with hyponatremia includes a
thorough history and physical examination, with particularly careful evaluation of ECF
volume status.
- Initial laboratory evaluation should include serum electrolytes, glucose, an evaluation of
renal function with urea, creatinine, serum osmolality, and urine osmolality and sodium.
- Treatment of hyponatremia must strike a balance between the risks of the hyponatremia
and the risks of correction.
- The magnitude of these risks depends on the degree of brain volume regulation that has
transpired as a result of intracranial fluid and solute shifts
- The treatment of some hyponatremia-associated disease states involves treating the
underlying etiology, such as steroids for adrenal insufficiency and thyroid hormone for
hypothyroidism.
- In most cases, the appropriate treatment of hyponatremia relies on the identification of
the underlying ECF volume status, the acuity with which the hyponatremia developed,
and the severity of neurologic symptoms present.
Severe acute symptomatic hyponatremia
- Acute hyponatremia (defined as <48 hours duration) with very low sodium
values (<110-115 mmol/L) with seizures or coma is a medical emergency.
- The risk for neurologic complications is high, because cerebral edema can evolve
quickly as a result of osmotic movement of water into the brain.
- In patients with severe acute hyponatremia, NaCl should be infused at a rate to increase
serum [Na] approximately 1 to 2 mmol/L/h until a less hyponatremic serum [Na]
(ie, 125-130 mmol/L) has been achieved.
- In comatose or seizing patients, a faster rate of sodium correction of 3-5 mmol/L/h for a
short period of time (ie, 1-2 hours) may be warranted to avoid imminent brainstem herniation.
- In hypovolemic states, including the majority of patients with a UNa less than 30
mmol/L, fluid resuscitation with isotonic NaCl is appropriate with a goal serum sodium
increase of 0.5 mmol/L/h. Accumulated evidence in experimental animals and humans
confirms that a slower rate of serum serum correction minimizes the risk for central
pontine myelinolysis
- The serum sodium should be measured every 2 to 4 hours during acute corrections of
hyponatremia to ensure that the increase in serum is proceeding at the desired rate.
- Young premenopausal women appear to be at greater risk for neurologic sequelae from
hyponatremia, with 75% of cases of brain damage occurring in this subpopulation in
some studies.
- In SIADH, fluid restriction is the mainstay of serum sodium correction, with the goal
of maintaining fluid intake 500 mL/d below urine output; however, this degree of fluid
restriction is difficult to maintain in an intensive care setting where obligate fluid intakes
for various therapies often exceed this level.
- Other therapies for chronic hyponatremia include demeclocycline (600-1200 mg/d),
furosemide (20-40 mg/d), NaCl tablets (3-18 g/d), and urea (30 g/d). Current clinical
trials are underway investigating the use of AVP V2 receptor antagonists
sodium deficit = 0.6 x weight in kg x [Na desired - Na measured]](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-164-320.jpg)
![hypophosphataemia
[created by Paul
Young 17/12/07]
general
- the body of an average 70kg adult contains 712g of phosphorus (28000mol)
- 85% is stored in bone as hydroxyapaptite crystals; 14% is found in soft
tissues and 1% is found in the blood
- phosphate is the most abundant intracellular anion with an intracellular concentration
of 100mmol/L which is 100 fold greater than levels found in the plasma
homeostasis
- normal dietary intake of phosphorus is 800g-1000g
- the homeostasis of phosphate is under the control of parathyroid hormone,vitamin D
& calcitonin and depends in the intestine, kidneys and bone
- bone metabolism is linked to calcium homeostasis. In the setting of hypocalcaemia,
increased parathyroid hormone levels cause phosphate and calcium to be released from
bone
- intestinal absorption of phosphate occurs in the small bowel, mainly the jejunum. Vitamin
D which is produced by the kidneys in increased amounts when serum phosphate levels
are low increases the intestinal absorption of both calcium and phosphate
- phosphate is excreted from the kidneys, but most of the excreted phosphate load undergoes
resorption in the proximal tubule. Parathyroid hormone increase phosphate excretion by
inhibiting reabsorption of phosphate
physiological
functions of
phosphate
1. it is the source of high energy phosphate bonds in ATP
2. it is a component of nucleic acids, phospholipids and enzymatic cofactors
3. it is a component of cGMP and cAMP which are important intracellular messengers
4. it is a component of 2,3 DPG which is important in oxygen delivery to tissues
5. it is an essential regulator of enzymes of the glycolytic pathway
6. it acts as a buffer in maintenance of plasma pH
7. it has a role in the immune system and the coagulation system
definitions
- the normal plasma level of phosphate is 0.8-1.3mmol/L
- moderate hypophosphataemia is defined as 0.32mmol/L to 0.65mmol/L
- severe hypophosphataemia is defined as <0.32mmol/L
causes
1. inadequate intake or absorption
- malnutrition
- phosphate binding antacids
- vitamin D deficiency
- chronic diarrhoea
- malabsorption syndromes
2. redistribution into cells
- refeeding syndrome (chronic malnutrition leads to protein catabolism with total
body phosphate depletion despite normal serum phosphate. Introduction of
carbohydrates leads to an anabolic state which unmasks total body phosphate
depletion and leads to precipitous drop in serum phosphate)
- insulin administration in DKA leads to correction of acidosis and unmasking of
existing total body phosphate deficit due to urinary loss by osmotic diuresis
- alkalosis causes shift into cells
3. renal losses
- diuretic therapy (acetazolamide produces greatest loss of phosphate while
frusemide has minimal effect; mannitol produces minimal phosphate loss but
interferes with the assay of serum phosphate producing falsely low levels
- osmotic diuresis
- hyperparathyroidism
- proximal renal tubular dysfunction (Fanconi's syndrome)
effects
treatment
4. extreme catabolic states
- burns, trauma and sepsis
respiratory effects
- acute respiratory failure
- ventilator dependence
- decreases 2,3 DPG causing leftward shift of the oxygen dissociation curve
musculoskeletal effects
- muscle weakness
- rhabdomyolysis
- bone demineralisation
haematological effects
- haemolysis
- disorders of leukocyte phagocytosis or chemotaxis
neurological
- altered mental state
- gait disturbance
- paraesthesias
cardiovascular
- reversible dilated cardiomyopathy
- decreased inotropy
general
- high dose iv phosphate therapy is not without complications and
hyperphosphataemia, hypocalcaemia, hypotension, tetany and
ECG abnormalities may all occur
- iv phosphate therapy should be administered with extreme caution
in patients with renal failure; iv phosphate therapy should also be
avoided in patients with hypercalcaemia as it may cause metastatic
calcification
- it is important to be aware of the potassium content of intravenous
phosphate preparations
- phosphorus depletion describes a situation of total body depletion. This may exist with
normal plasma phosphate levels such as in malnutrition and DKA
specific approaches:
- KH2PO4 contains 10mmol phosphate
and 10mmol K per 10ml ampoule
- NaKH2PO4 contains 13.4mmol phosphate,
21.4mmol Na, 2.6mmol K in a 20ml ampoule
- if phosphate 0.65 to 0.89 oral phosphate is
most appropriate
- if phosphate is 0.4-0.65 then 3 ampoules
in 100ml normal saline over 3 hours
- if phosphate <0.4 then 4 ampoules in
100ml normal saline over 4 hours](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-165-320.jpg)
![hypopituitarism
[created by
Paul Young
10/07/12]
physiology
aetiology
investigation
treatment
general
epidemiology
- Incidence and prevalence of hypopituitarism are estimated to
be 4.2 per 100 000 per year and 45.5 per 100 000, respectively.
Hypopituitarism is the inability of the pituitary gland to provide sufficient hormones adapted
to the needs of the organism. It might be caused by either an inability of the gland itself to
produce hormones or an insufficient supply of hypothalamic-releasing hormones.
hormone tests
clinical
features
- Tumoral masses in the sellar region with suprasellar extension can become manifest with visual impairment that is slowly progressive in most
cases. Visual-field defects can present not only as classic bitemporal hemianopsia but also unilaterally in many cases. Usually, such defects
remain unrecognised by patients until diagnosed by a doctor.
- Headaches can be an unspecific symptom of tumour masses. In case of lateral extension, rarely, signs of oculomotor nerve impairment
and, even less common, additional damage to other cranial nerves within the cavernous sinus might arise.
- Hypopituitarism can be subclinical, indicated only by measurement of hormones, or its clinical onset might be acute and severe, necessitating
admission and intensive care management. Shortages of adreno corticotropic hormone (ACTH), thyroid-stimulating hormone (TSH), and
antidiuretic hormone (ADH) are potentially life-threatening
- Gonadotropin and growth-hormone deficiencies, on the other hand, cause chronic morbidity. Raised prolactin concentrations sometimes
accompany hypopituitarism because of disruption of inhibitory signals by the hypothalamus. This alteration can cause lactation, tenderness
of the breast, and suppression of gonadotropins, leading to symptoms of hypogonadism.
Imaging
- Cranial MRI should be done to exclude tumours and other lesions of the sellar and parasellar region after hypopituitarism
has been confirmed. Of sellar tumours, the pituitary adenoma is the most frequent. However, hypopituitarism is not
excluded by normal MRI of the sellar and parasellar region.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-166-320.jpg)



![ICU-acquired
weakness
[created by
Paul Young
02/10/07]
clinical
presentation
common scenarios include:
(i) difficulty weaning
(ii) generalised weakness
- When a reliable motor examination is possible, affected
patients will exhibit generally symmetrical motor deficits
in all limbs, ranging from paresis to true quadriplegia.
- Reflexes are usually diminished or absent, but
normal reflexes do not rule out the diagnosis.
- Sensory examination is often curtailed by patient
sensorium, interaction with the examiner, and edema.
differential
diagnosis
- Once a weakness syndrome is entertained, the
clinician must clearly establish the absence of a
neuromuscular condition that began before admission
to the ICU
such conditions include:
- acute spinal cord injury,
- motor neuron disease,
- Guillain-Barre syndrome,
- myasthenia gravis,
- Lambert-Eaton syndrome, and
- muscular dystrophy
general
ICU-acquired weakness encompasses:
(i) critical illness polyneuropathy (CIP), and
(ii) critical illness myopathy (CIM)
CIP vs CIM
- In CIP, electrophysiologic testing usually shows sensorimotor
axonopathy with decreased compound muscle action potential
(CMAP) and sensory nerve action potential yet normal nerve
conduction velocities
- CIM is an acute primary myopathy (not secondary to muscle
denervation) and is diagnosed by abnormalities of the electro-
myographic tracing during a voluntary contraction (requiring
patient cooperation). The definitive diagnosis of muscle
involvement requires examination of muscle tissue by biopsy with
selective loss of myosin being practically pathognomonic.
- aka acute quadriplegic myopathy
approach
investigation
arguments for specific investigation:
(i) CIM and CIP are potentially reversible entities, therefore should be
carefully identified to avoid unreasonably pessimistic prognoses
(ii) accurate predictions are paramount in decisions regarding goals of
care in the patient with protracted critical illness.
(iii) may identify an alternative diagnosis
arguments against specific investigation:
(i) Technical difficulties in investigation of ICU patients including oedema,
artifacts related to the presence of multiple electrical devices, and invasive
catheters are common sources
(ii) Neurophysiologic testing does not predict duration of mechanical
ventilation nor ICU stay
(iii) The presence of CIP and/or CIM does not ensure reversibility
(iv) establishing a highly specific diagnosis does not translate to a specific therapy.
prognosis
short-term:
- ICU acquired weakness has been demonstrated to lead to longer ventilation, ICU stay and
mortality yet no conclusive evidence exists to refute the possibility that poor outcomes and
weakness may simply reflect the type and/or severity of the patient’s underlying condition.
long-term:
- Metaanalysis of 36 studies provided information on the outcomes of 263 patients.
Mean duration of follow-up was 3 to 6 months (range, 2 days to 8 years).
- Complete functional recovery with patients regaining the ability to breathe
spontaneously and to walk independently was reported in 68% (180 of 263 patients).
- Severe disability with quadriparesis, quadriplegia, or paraplegia
was reported in 28% (74 of 263 patients).
- Persisting milder disabilities were common even in patients with complete functional
recovery, and included reduced or absent deep tendon reflexes, stocking and glove
sensory loss, muscle atrophy, painful hyperesthesia, and foot drop
epidemiology
- De Jonghe et al found clinically significant ICU-AW in 25% of
patients who received mechanical ventilation for at least 7 days.
- Studies using cohorts restricted to sepsis and multiorgan failure have found
even higher incidences of neuromuscular disease, ranging from 50 to 100%.
risk
factors
1. systemic inflammation
2. glycaemic control:
- tight glycaemic control appears to decrease
prevalence of ICU-acquired weakness
3. medications
- steroids and neuromuscular blocking agents
4. immobility
risk factor
modification
5. malnutrition](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-170-320.jpg)
![ICU
management
of abdominal
trauma
[Created by
Paul Young
28/10/07]
general
- admission to ICU necessitates reevaluation of the patient
by repeating the primary & secondary surveys
- repeat primary survey is required because:
(i) transport may have dislodged equipment
(ii) significant time may have elapsed since the initial primary survey
- secondary survey is required because:
(i) it may have been interrupted due to the need for urgent operation
(ii) patient may have been transferred to ICU due to a decline in clinical status
(iii) 10% of trauma patients have injuries that are missed during the initial evaluation
(iv) 25% of abdominal injuries are undetected at the time of presentation
admission
after
damage
control
laparotomy
General:
- 'damage control' refers to urgent abdominal exploration with the
basic goal of controlling massive bleeding & preventing ongoing
peritoneal contamination
- after 'damage control' patients often arrive in the ICU hypothermic,
acidotic & coagulopathic. ICU goal is to correct these abnormalities
to allow return to theatre for definitive operation as required
- failure to correct acidosis of coagulopathy suggests ongoing bleeding
which may require return to theatre
Rewarming:
- warm blankets & a warm room are essential & should be prepared
before the patient arrives
- all intravenous fluids should be warmed
- rarely invasive techniques for active rewarming may be required
Correction of acidosis:
- acidosis is generally the result of global hypoperfusion & should
correct with restoration of circulatory volume and haemoglobin
Correction of coagulopathy:
- clotting factors function best at normal temperature and normal pH
- standard coagulation tests may be normal in the lab at 37 degrees
despite significant coagulopathy in the hypothermic patient
- coagulopathy may also be a result of dilution in massive transfusion or
disseminated intravascular coagulation
- calcium is bound by citrate, a preservative in packed red cells and needs
to be aggressively replaced as it acts in the clotting cascade and is required
for normal contractive function of the heart and circulatory system
delayed
complications
- delayed complications from either known or unsuspected intra-
abdominal injuries generally manifest as sepsis
- the possibility of missed hollow viscous injury is a major concern
during the nonoperative management of patients
- when solid organ injuries are identified the risk of hollow viscus injury
increases so that 6% of patients with one solid organ injury have a
viscus injury, 22% with two solid organ injuries have a viscus injury
& 33% of patients with three solid organ injuries have a viscus injury
admission
for non-
operative
management
of solid organ
injury
- non-operative management consists of:
(i) serial physical examination
(ii) serial measurement of laboratory parameters
(iii) strict bed rest
(iv) optimisation of coagulation status
- changes in physical examination findings, haemodynamic
status (including tachycardia) or transfusion should be promptly
communicated to the trauma surgeon as any clinical deterioration
may necessitate immediate angiography or operation](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-171-320.jpg)
![ileus
[created
by Paul
Young
04/10/07]
general
normal
gastrointestinal
motility
treatment
- ileus is defined as the absence of physiological motility of the
bowel leading to a disturbance in the progression of bowel contents
through the gastrointestinal tract; it must be distinguished from
mechanical obstruction
neostigmine:
- dramatic effect for treatment of colonic pseudoobstruction has
been demonstrated with 2mg iv of neostigmine (N Engl J Med
1999; 341: 137-41)
- when a food bolus is introduced into the intestine, organised
migrating motor complexes that exist at rest disappear and
digested food is propelled through the GI tract by spikes of
contraction of smooth muscle in the the wall of the gut
- PSNS increases GI motility while SNS decreases it
- nitric oxide produces smooth muscle relaxation and decreases
gastrointestinal motility
- some endocrine substances increase GI motility including:
(i) motilin
(ii) gastrin
(iii) cholecystokinin
- some endocrine substances decrease GI motility including:
(i) somatostatin
(ii) glucagon
clinical
consequences
- ileus results in inability to tolerate enteral feeding,
nausea, vomiting & constipation
- accumulation of fluid and air in the bowel results
in abdominal distention
- serious consequences of ileus include intestinal ischaemia,
intestinal perforation and abdominal compartment syndrome
- intolerance of enteral feeding compromises the ability to
provide adequate nutrition to critically ill patients
diagnosis
- ileus is suggested by the presence of the following signs and symptoms:
(i) abdominal distention
(ii) nausea
(iii) vomiting
(iv) high NG output
(v) high gastric residual volumes during enteral feeding
(vi) abdominal pain
(vii) absent bowel sounds
(viii) constipation
- radiological findings suggestive of ileus are increase air in the
small intestine, bowel distention & the presence of air-fluid levels
pathogenesis
- three types of clinical ileus are observed:
(i) adynamic ileus
(ii) spastic ileus (observed rarely in diseases
such as porphyria or lead poisoning)
(iii) ischaemic ileus (identified in haemodynamically
stable patients with low flow states)
general measures:
- adequate resuscitation is important if at all possible to ensure that
organ blood flow is optimised; exogenous catecholamines promote
the development of ileus and should be limited where possible
- avoid excessive iv hydration as bowel oedema worsens ileus
- avoid narcotics where able
- correct electrolyte disturbances (hypokalaemia in particular inhibits
normal muscle contraction)
feeding:
- avoid prolonged starvation as prolonged starvation is associated
with mucosal atrophy; early use of GI tract is associated with achieving
caloric goals earlier, earlier bowel movements and shorter length of
hospital stay (10-20ml/hr is all that is required for this)
- do not assume that a patient with ileus should not be fed enterally;
passage of flatus and bowel sounds are not reliable indicators of
normal gastrointestinal motility and virtually all haemodynamically
stable patients should be enterally fed
- TPN is not a substitute for enteral nutrition and there are no data to
support indiscriminate use of TPN in patients with ileus
metoclopramide:
- widely used but has not been shown to be beneficial
NSAIDS:
- systemic ketorolac is associated with early bowel movements
and increased tolerance to oral diet; it also causes GI bleeding
and renal impairment which limits its utility in critical care
erythromycin:
- used because of its molecular similarity to motilin
- no standardised definition exists
newer agents:
- agents being investigated include narcotic antagonists, nitric oxide
synthase inhibitors and protein tyrosine kinase inhibitors](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-172-320.jpg)

![indications
for adult
cardiac
surgery
[created by
Paul Young
14/10/07]
coronary
artery
disease
general:
- the aim of surgery is to eliminate symptoms & prolong life so
the indications should be based on:
(i) symptoms
(ii) left ventricular function
(iii) area of ischaemia
(iv) anatomic localisation of coronary artery stenosis
specific anatomical coronary lesions:
(i) left main stenosis of >50% or a left main equivalent (>70%
stenosis in the proximal LAD & proximal Cx arteries)
(ii) triple vessel disease with >70% lesions in all 3 coronary territories
(iii) significant proximal LAD stenosis with 2 vessel disease
NB: long term survival benefit is even greater when LV function is
depressed before surgery
trials:
- in the early 1990s, three large multicentre randomised trials were undertaken
in Europe & the United States: the Veterans Administration Cooperative Study,
the European Coronary Surgery Study and the Coronary Artery Surgery Study
which all demonstrated a significant benefit for CABG over medical treatment
- since these trials several important factors have changed:
(i) patients are older (patients >65 were excluded)
(ii) surgical techniques have improved with use of arterial grafts
(iii) new medical therapies such as statins have been shown to prolong life after CABG
predicted surgical risk:
- risk factors that increase perioperative mortality include:
(i) increased age
(ii) diabetes mellitus
(iii) COPD
(iv) renal failure
(v) previous surgery
(vi) left ventricular dysfunction
(vii) pulmonary hypertension
(viii) emergency operation
- risk can be predicted with the Euroscore (www.euroscore.org)
aortic
valve
surgery
aortic stenosis:
(i) symptomatic aortic stenosis (unless comorbidities preclude it)
- surgery is the only effective therapy for symptomatic AS
(ii) mild to moderate aortic stenosis undergoing CABG
- aortic stenosis is graded based on echocardiography criteria
mild (effective valve area of >1.5cm2)
moderate (effective valve area of >1-1.5cm2)
severe (effective valve are of <1cm2)
aortic regurgitation:
(i) NYHA class III or IV symptoms due to AR
(ii) LVEF <25% or end systolic dimension >60mm or both
(iii) LVEF 25-49% may be an indication (controversial)
(iv) AR associated with aortic root dilatation of >50mm
mitral
valve
surgery
mitral stenosis:
(i) moderate or severe mitral stenosis (mitral valve area <1.5cm2)
in symptomatic patients (NYHA III or IV)
mitral regurgitation:
(i) symptomatic mitral regurgitation
(ii) assymptomatic patients with mild or moderate LV dysfunction
(iii) acute onset of atrial fibrillation due to MR
- ischaemic MR may improve with revascularisation](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-174-320.jpg)



![intraabdominal
infections
[created by
Paul Young
02/10/07]
empirical
antimicrobial
therapy
Hospital-acquired intra-abdominal infections:
- Postoperative (nosocomial) infections are caused by more-resistant flora, which may include:
(i ) Pseudomonas aeruginosa,
(ii) Enterobacter species,
(iii) Proteus species,
(iv) methicillin-resistant Staphylococcus aureus,
(v) enterococci, and
(vi) Candida species.
- For these infections, complex multidrug regimens are recommended, because adequate empirical
therapy appears to be important in reducing mortality. Local nosocomial resistance patterns should
dictate empirical treatment, and treatment should be altered on the basis of the results of a thorough
microbiologic workup of infected fluid.
which patients
require antimicrobials?
- Bowel injuries due to penetrating, blunt, or iatrogenic trauma
that are repaired within 12 h and intraoperative contamination
of the operative field by enteric contents under other circumstances
should be treated with antibiotics for no more than 24 h
- acute appendicitis without evidence of gangrene, perforation, abscess,
or peritonitis requires only prophylactic administration of inexpensive
regimens active against facultative and obligate anaerobes
- Acute cholecystitis is often an inflammatory but noninfectious disease.
If infection is suspected on the basis of clinical and radiographic findings,
urgent intervention may be indicated, and antimicrobial therapy should
provide coverage against Enterobacteriaceae. Activity against enterococci
is not required, because their pathogenicity in biliary tract Infections has not
been demonstrated. Coverage against anaerobes is warranted in treatment
of patients with previous bile duct–bowel anastomosis
- Infections occurring during the course of acute necrotizing
pancreatitis are due to microbial flora similar to that found in
infections resulting from colonic perforations
Community-acquired intra-abdominal infections
- Antibiotics used for empirical treatment of community acquired intra-abdominal infections should be active
against enteric gram-negative aerobic and facultative bacilli and b-lactam–susceptible gram-positive
cocci. Coverage against obligate anaerobic bacilli should be provided for distal small-bowel and colon-derived
infections and for moreproximal gastrointestinal perforations when obstruction is present
indications for
antifungal therapy
- Candida albicans or other fungi are isolated from ~20% of patients with acute perforations
of the gastrointestinal tract. Even when fungi are recovered, antifungal agents are unnecessary,
unless the patient has recently received immunosuppressive therapy for neoplasm, transplantation,
or inflammatory disease or has post-operative or recurrent intraabdominal infection.
- Anti-infective therapy for Candida should be withheld until the infecting species is
identified. If C. albicans is found, fluconazole is an appropriate choice. For fluconazole
resistant Candida species, therapy with amphotericin B, caspofungin, or voriconazole is
appropriate. The latter 2 agents cause substantially less toxicity than does amphotericin B
and are specifically indicated for patients with renal dysfunction
indications for
anti-enterococcal
therapy
- Numerous prospective, blinded, and randomized trials have compared regimens active against
strains of Enterococcus routinely isolated from patients with community-acquired infections.
None have demonstrated benefit from covering enterococcus in this setting
- Antimicrobial therapy for enterococci should be given when enterococci
are recovered from patients with health care–associated infections
duration
of therapy
- Antimicrobial therapy for established infections should be continued until resolution of clinical signs of
infection occurs, including normalization of temperature and WBC count and return of gastrointestinal function.
- The risk of subsequent treatment failure appears to be quite low for patients who have no clinical evidence
of infection at the time of cessation of antimicrobial therapy.
- For patients who have persistent or recurrent clinical evidence of intra-abdominal infection after 5–7 days of
therapy, appropriate diagnostic investigation should be undertaken. This should include CT or ultrasonographic
imaging, and antimicrobialtherapy effective against the organisms initially identified should be continued
pyogenic
liver
abscess
- A pyogenic liver abscess usually develops by spread of infection from an
intra-abdominal source, such as diverticulitis or the biliary tract.
- Causative organisms are often a mixture of aerobic and anaerobic bowel flora, but occasionally
an organism of the Streptococcus anginosus/milleri group may be found alone.
- Klebsiella pneumoniae is an increasingly identified cause of liver abscess,
particularly in patients from Asia. It is usually the sole infecting organism and has
a higher incidence of metastatic infections than non-Klebsiella infections.
- The antibiotic regimen for acute peritonitis due to perforated viscus is generally appropriate initial therapy.
In children, in whom Staphylococcus aureus is a common cause, consider use of an antistaphylococcal drug.
- When culture results are available, modify therapy accordingly and continue for at least 4 to 6 weeks.
- Some form of drainage procedure is usually necessary.
- Where the aetiology is not clearly pyogenic, undertake serological testing for Entamoeba
histolytica and Echinococcus granulosus (see hydatid disease), and consider testing for
Fasciola hepatica. If radiological imaging suggests hydatid disease, needle aspiration should
be delayed pending these results to avoid intraperitoneal spillage of hydatid contents.
Likely
pathogens
by site
- Infections derived from the stomach, duodenum, biliary system,
and proximal small bowel can be caused by gram-positive
and gram-negative aerobic and facultative organisms.
- Infections derived from distal small-bowel perforations can be caused by
gram-negative facultative and aerobic organisms with variable density.
- Perforations of this type often evolve into localized abscesses, with
peritonitis developing only after rupture of the abscess.
- Anaerobes, such as B. fragilis, are commonly present.
- Colon-derived intra-abdominal infections can be
caused by facultative and obligate anaerobic organisms.
- Streptococci and enterococci are also commonly present.
- By far the most common gram-negative facultative organism is E. coli.
peritonitis
due to
perforated
viscus
- Peritonitis due to perforated viscus is usually a polymicrobial infection with aerobic and
anaerobic bowel flora. It may not be necessary to cover all organisms present.
- Use:
amoxy/ampicillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
PLUS
gentamicin 4 to 6 mg/kg (child <10 years: 7.5 mg/kg; >10 years: 6 mg/kg) IV, daily
(adjust dose for renal function)
PLUS
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 12-hourly.
- Alternatively, if gentamicin is contraindicated as a single preparation, use:
piperacillin+tazobactam 4+0.5 g (child: 100+12.5 mg/kg up to 4+0.5 g) IV, 8-hourly
OR
ticarcillin+clavulanate 3+0.1 g (child: 50+1.7 mg/kg up to 3+0.1 g) IV, 6-hourly.
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity), use:
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 12-hourly
PLUS EITHER
Ceftriaxone 1 g (child: 25 mg/kg up to 1 g) IV, daily
OR
cefotaxime 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly.
- For patients with immediate hypersensitivity to penicillin, substitute vancomycin for
amoxy/ampicillin in the first-listed regimen:
vancomycin 25 mg/kg up to 1 g (child <12 years: 30 mg/kg up to 1 g) IV, 12-hourly
(monitor blood levels and adjust dose accordingly)
acute
pancreatitis
Severe non-necrotising pancreatitis
- There is no evidence that antibiotic therapy is useful for non-necrotising severe pancreatitis.
Severe necrotising pancreatitis
- Patients with infected pancreatic necrosis or abscess require surgical referral, usually for treatment
with drainage and/or debridement, in addition to antibiotic therapy. The role of prophylactic antibiotics
in improving the clinical outcome associated with severe pancreatitis appears to be limited to those
patients with necrotising pancreatitis, and even in these patients their role is controversial.
- If sepsis is suspected or proven, antibiotics should be used:
meropenem 500 mg IV, 8-hourly for 7 days
OR
imipenem 500 mg IV, 6-hourly for 7 days
OR
piperacillin+tazobactam 4+0.5 g IV, 8-hourly for 7 days.
- For patients with immediate penicillin hypersensitivity, seek advice from an infectious
diseases physician or clinical microbiologist.
ascending
cholangitis
- Ascending cholangitis is usually associated with Gram-negative sepsis and prompt antibiotic
treatment is essential. If biliary obstruction is present, appropriate drainage should be undertaken.
- For initial antibiotic treatment, use:
amoxy/ampicillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
PLUS
gentamicin 4 to 6 mg/kg (child <10 years: 7.5 mg/kg; ?10 years: 6 mg/kg) IV, daily
for up to 3 days (adjust dose for renal function)
NB: Unrelieved biliary obstruction may potentiate aminoglycoside toxicity for courses longer than 72
hours. This effect occurs almost exclusively in patients with initial bilirubin levels above 85 micromol/L.
However, empirical gentamicin is preferred to broad-spectrum beta lactams because it has a broader
Gram-negative spectrum and is more rapidly bactericidal.
- If ongoing IV therapy is required after 3 days, a different regimen should be used
- In patients with a history of previous biliary tract surgery or known biliary obstruction, add:
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 12-hourly.
- Alternatively, for patients hypersensitive to penicillin (excluding immediate hypersensitivity)
or when gentamicin is contraindicated, as a single drug, use:
ceftriaxone 1 g (child: 25 mg/kg up to 1 g) IV, daily
OR
cefotaxime 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly.
- In patients unresponsive to initial therapy or requiring IV therapy beyond 3 days, blood culture
results may provide a guide to appropriate therapy. In the absence of this information, use:
piperacillin+tazobactam 4+0.5 g (child: 100+12.5 mg/kg up to 4+0.5 g) IV, 8-hourly
OR
ticarcillin+clavulanate 3+0.1 g (child: 50+1.7 mg/kg up to 3+0.1 g) IV, 6-hourly.
- Response to effective biliary drainage and antibiotics is usually rapid. When afebrile, change to:
amoxycillin+clavulanate 875+125 mg (child: 22.5+3.2 mg/kg up to 875+125 mg) orally, 12-hourly
for a total treatment duration of 7 days.
acute
cholecystitis
- Causative organisms of acute cholecystitis are usually aerobic bowel flora (eg Escherichia coli,
Klebsiella species and, less commonly, Enterococcus faecalis). Anaerobes are found infrequently,
unless obstruction is present.
- When there is evidence of sepsis, use:
amoxy/ampicillin 1 g (child: 25 mg/kg up to 1 g) IV, 6-hourly
PLUS
gentamicin 4 to 6 mg/kg (child <10 years: 7.5 mg/kg; >10 years: 6 mg/kg) IV, daily (adjust dose for renal function)
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity,
or when gentamicin is contraindicated, as a single drug, use:
ceftriaxone 1 g (child: 25 mg/kg up to 1 g) IV, daily
OR
cefotaxime 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly.
- Note that cephalosporins are not active against enterococci. If biliary obstruction
is present, add metronidazole (400 mg orally 12-hourly) to treat anaerobes.
- When afebrile and if ongoing oral therapy is required, change to:
amoxycillin+clavulanate 875+125 mg (child: 22.5+3.2 mg/kg up to 875+125 mg) orally, 12-hourly.
Stop antibiotics when patient has been afebrile for 48 hours and has a normal neutrophil count.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-178-320.jpg)


![intracerebral
haemorrhage
[created by
Paul Young
04/11/07]
general
pathophysiology
aetiology
clinical
features
diagnostic
studies
airway
management
haemodynamics
prevention of
haemorrhage
extension
hydrocephalus
intracranial
hypertension
surgical
evacuation
thrombolytic-
induced
haemorrhage
outcome
- spontaneous intracerebral haemorrhage accounts for approximately 10% of all strokes in North
America and 20-30% in East Asia
- is associated with greater mortality and more severe neurological deficits than any other stroke
type with nearly half of all patients dying in the 1st 30 days & survivors often having significant
residual disability
primary injury
- primary injury is due to local tissue destruction as rupture of a cerebral blood
vessel introduces a stream of blood into the brain parenchyma
- in more than 1/3rd of patients, continued bleeding or rebleeding leads to haematoma
enlargement & further mechanical damage over the 1st few hours
secondary injury
- secondary injury is thought to occur due to ischaemia and cerebral oedema
hypertensive haemorrhage:
- occurs predominantly deep in the cerebral hemispheres most often in the putamen; other
frequent sites include the thalamus, cerebellum & pons (all of these sites are supplied by
small penetrating arteries that branch directly off large vessels & thus are exposed to high sheer)
aneurysms and vascular malformations:
- up to 1/4 of intracerebral haemorrhage is attributable to intracranial
aneurysms or vascular malformation
- although aneurysmal rupture is most commonly associated with haemorrhage into the
subarachnoid space, the blood may also be directed into the substance
of the brain if the aneurysm is adherent to the brain parenchyma
- approximately 1/2 of intracranial AVMs in adults present with haemorrhage.
The majority of AVMs become symptomatic by the age of 40. Multiple calcified
channels may be seen within the haematoma on CT suggesting the presence
of an AVM
other causes:
(i) cerebral amyloid angiopathy
- is an important cause of haemorrhage in the elderly
(ii) haematological causes
- coagulopathy related ICH is most often due to warfarin therapy but may also be
seen with other antithrombotic and thrombolytic agents
(iii) malignancy
- haemorrhage from underlying malignancy is rare; however, it occasionally occurs
with glioblastoma multiforme and lymphoma and with melanoma, choriocarcinoma,
renal cell carcinoma and bronchogenic carcinoma
- benign tumours are almost never a cause of intracerebral bleeding
(iv) infection
- bleeding may occur in association with fungal infection eroding a vessel wall or
necrotising haemorrhagic encephalitis with herpes simplex virus
(v) venous sinus occlusion
(vi) sympathomimetics (eg cocaine, amphetamines)
(vii) following reperfusion (after endartectomy or thrombolysis)
(viii) haemorrhagic transformation after acute ischaemic stroke
- the clinical presentation of ICH is often indistinguishable from ischaemic stroke; however, more commonly
includes altered level of consciousness, headache and vomiting (due to elevated intracranial pressure)
- blood pressure elevation is common
- 15-25% of patients develop seizures in the 1st 48 hours
- symptoms are maximal at onset or develop over minutes to hours
CT
- non-contrast CT scanning remains the gold standard for diagnosis of acute intracerebral haemorrhage
with typical appearance of acute haematoma consistning of a well defined area of increased density
surrounded by a rim of decreased density
MRI:
- MRI is less reliable for detection of acute haemorrhage than CT;
however, it is better at determining the age of a haemorrhage
angiography:
- can be useful in evaluating the cause of intracerebral haemorrhage where an underlying
aneursym or vascular malformation is suspected or demonstrated on CT or MRI
- airway compromise may occur for two reasons in intracerebral haemorrhage:
(i) diminished consciousness may result in relaxation of the pharyngeal
musculature and tongue and suppression of the cough and gag reflexes
(ii) ICH involving the posterior fossa may lead to complete loss of pharyngeal
tone and absent cough, swallow and gag reflexes
- intubation of patients with ICH requires adequate sedation and relaxation
as well as prevention of ICP elevation
- ICP elevation may be caused by several factors during intubation including
hypoxaemia, hypercarbia and direct tracheal stimulation
- arterial blood pressure is elevated in the majority of patients presenting
with ICH even in the absence of a history of hypertension
- there is substantial controversy over whether and when to lower blood
pressure after acute ICH and how aggressive any intervention should be
- arguments for acute lowering of blood pressure are as follows:
(i) high blood pressure may predispose to haematoma enlargement
and may contribute to worsening of oedema
(ii) hypertension during the acute phase of ICH has been shown to correlate with poor outcome
(iii) to limit the potential for end-organ damage including myocardial
infarction, CCF, and acute renal failure
- arguments against lowering blood pressure:
(i) lowering blood pressure might exacerbate ischaemic damage in
tissue surrounding haemotoma by impairing CBF
(ii) chronic hypertension shifts the cerebral autoregulation curve to the right such that a higher CPP is
required to maintain normal CBF; lowering blood pressure to "normal" levels may lead to impaired CBF
- in summary, unless there are signs of systemic complications, there appears
to be no compelling need to treat hypertension aggressively in the acute phase
- modest blood pressure reductions of 15-20% in very hypertensive patients
(MAP>130mmHg) appear to be safe
- in theory vasodilators such as GTN and nitroprusside can increase ICP; therefore,
beta blockers, ACE inhibitors and calcium channel blockers are preferred agents
- because haemorrhage extension may occur in the 1st few hours
aggressive correction of coagulopathy is warranted
- even patients without coagulopathy may benefit from factor VIIa to
promote haemostasis and prevent haemorrhage extension
- in approximately 40% of patients with ICH, blood extends into the ventricular system where
it may block cerebrospinal fluid pathways with resultant hydrocephalus and increased ICP
- hydrocephalus may also develop due a direct mass effect on a ventricle
- EVD is frequently used to treat hydrocephalus; however, efficacy has never been
established and catheters frequently become blocked if there is intraventricular blood
- intraventricul ar urokinase has been used intraventricularly to facilitate clearance of blood from the ventricles.
In a preliminary trial, it showed no increase in complications and a trend towards decreased mortality
- the incidence, impact and appropriate management of intracranial
hypertension in ICH is not well understood
- invasive monitoring is not routinely performed
- the rationale for surgical evacuation of haematoma is that reducing mass effect and removing the neurotoxic
clot consitituents should minimise injury to adjacent brain tissue and hence improve outcome
- unfortunately, several randomised trials for supratentorial ICH all failed to show a benefit and metaanalysis
of these trials reported that patients undergoing surgical evacuation had a higher rate of death than those
managed medically. Criticisms of these trials include outdated surgical technique, inadequate patient selection
and delay in performance of surgery
- The STITCH trial randomized 1,033 patients in 27 countries to early surgery or conservative treatment. Eligible
patients had computed tomographic evidence of intracerebral hemorrhage within 72 hours, with a minimum
hematoma diameter of at least 2 cm and a Glasgow Coma Scale (GCS) score of at least 5
- Overall, a favorable outcome at six months was reported in 26 percent of surgical patients and 24 percent of
conservative treatment patients. Mortality rates did not differ significantly between the groups
- Some limited data support the use of minimally invasive surgical techniques (endoscopic
aspiration or stereotactic haematoma evacuation) compared to medical therapy
- surgical intervention is generally recommended in cerebellar haematoma if there is diminished level of
consciousness, a large haemoatoma (>3cm3), a midline location, compression of basal cisterns or brainstem
or hydrocephalus
- symptomatic ICH is a feared complication of thrombolytic therapy and is associated with considerable
morbidity and mortality
- it is more common after thrombolytic treatment of stroke than of thrombolytic treatment of extracerebral thrombosis
- in the setting of thrombolytic therapy, any new deficit should be assumed to be due to haemorrhage and
infusion should be stopped while urgent CTB is obtained. Preparations should be made to administer
blood products if needed
- mortality following ICH is 25-50% with hald deaths occurring in the 1st 48 hours
- although patients with small haemorrhages and minor deficits may recover
completely, the majority of survivors have significant residual disability
- withdrawal of support biases predictive models in ICH as withdrawal of care is a frequent mechanism of death
- early herniation leading to brain death is another common mechanism of death
- medical complications of pulmonary embolism, pneumonia and sepsis accout for most of the other deaths](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-181-320.jpg)
![acute
ischaemic
stroke
[created by
Paul Young
03/11/07]
general
pathophysiology
emergent
stroke
evaluation
tPA
other
thrombolytics
tpa in
specific
subgroups
intra-arterial
thrombolysis
combination
therapy
mechanical
devices
surgical
options
- the rationale for acute ischaemic stroke treatment is that when arterial occlusion occurs there is an
area of infarcted brain the is surrounded by a region of that has reduced blood flow impairing function but
not sufficiently severe to result in irreversible infarction
- this is the 'ischaemic pendumbra' and if adequate blood flow can be restored within a critical time frame
this area may return to normal function
- ischaemic strokes are generally classified as:
(i) large vessel thrombotic
(ii) small vessel thrombotic
(iii) embolic
- large vessel thrombotic strokes are often preceded TIAs
- clinical deficits typically correspond to the territory of a
major cerebral artery or their border zones
- in embolic strokes, the onset is usually sudden
- the presence of AF, rheumatic heart disease or a recent
myocardial infarction increase the probability of embolism
- several clinical syndromes are attributable to small vessel or lacunar strokes including
pure motor stroke, pure sensory stroke, ataxic hemiparesis and dysarthria/clumsy hand
syndrome
- clinical determination is unreliable and imaging is required
general assessment:
- emergent assessment of the stroke patient begins prehospital and mechanisms are required for
early notification if aggressive early therapies are feasible
- initial assessment should be performed rapidly and targetted towards assuring adequate airway
and ventilation [particularly in obtunded or comatose patients]
- hypoxaemia should be corrected [aspiration is a major cause of morbidity in these patients]
- arrhythmias are common in stroke patients [particularly AF] and bradycardia
may signal increased intracranial pressure
- hypotension should be corrected
- seizures should be controlled with anticonvulsants
- hypoglycaemic may mimic stroke and should be treated
blood pressure management:
- hypertension commonly accompanies stroke & in most cases treatment is not recommended due
to the risk of causing further impairment of perfusion to ischaemic penumbra
- when thrombolytic therapy is considered, SBP should be controlled to less
than 185mmHg or diastolic less than 110mmHg
triage & laboratory studies:
- immediate concern for the emergency department after initial stabilisation is confirming the diagnosis of
stroke, excluding stroke mimics & established whether acute intervention is warranted
- establishing time of onset is crucial and if rapid intervention is needed then CT should be performed rapidly
- additional blood tests include coagulation studies, full blood count & electrolytes
glucose:
- evidence from animal models of stroke suggests that hyperglycaemia increases the severity of ischaemic
injury & initial blood glucose in acute stroke is correlated with outcome independent of initial stroke severity
- although studies have not been performed to demonstrate a beneficial effect on outcome of controlling
blood glucose, it seems reasonable to control glucose to reasonable levels
temperature control:
- fever is clearly associated with worse outcomes after stroke
- hypothermia reduces stroke severity in animal models of stroke but no randomised
trials have been completed in humans
- despite the uncertainty or benefit, maintenance of normothermia is advised after stroke
stroke team:
- a stroke team consists of individuals from multiple disciplines with specialised knowledge and interest in acute
ischaemic stroke. The stroke team is usually responsible for evaluating the CT scan, establishing the diagnosis
and making the decision about treatment
general:
- further analysis of the NINDS study did not identify any specific subgroups with a greater or lesser likelihood
of responding to tPA; however, clinical experience has raised questions about treatment of several subgroups
age and risk of thrombolytics:
- elderly patients have a higher incidence of cerebral amyloid angiopathy which might predispose to haemorrhage after tPA
- in the NINDS study, older patients were less likely to have a favourable outcome but fared better with tPA than without it
- in ECASS II, older patients had a greater risk of haemorrhagic transformation
- advanced age is not a contraindication to thrombolysis but requires consideration
of a lower probability of good outcome and higher risk of haemorrhage
CT findings on baseline scan:
- before RCT tPA trials, several studies suggested that the presence of early
changes on CT predicted a greater risk of haemorrhagic transformation
- in ECASS II early hypodensity was an independent risk factor for intracranial haemorrhage
- in the NINDS study the odds ratio of symptomatic haemorrhage was increased (2.9 vs 1.5) with hypodensity of
>1/3rd the MCA territory; however, few patientshad this finding on baseline scan and the increased risk of
haemorrhage did not reach statistical significance
- analysis of the Australian Streptokinase study failed to show any significant relationship between ischaemic
changes on baseline CT (within 4 hours of symptom onset) and intracerebral haemorrhage
aspirin pretreatment:
- may individuals at risk of stroke are treated with aspirin or other antiplatelet agents
- whether aspirin increases the risk of thrombolytic therapy is unclear
- in MAST-I, patients treated with aspirin and streptokinase had a higher incidence of death from intracerebral haemorrhage
- aspirin pretreatment was not associated with intracerebral haemorrhage in the NINDS trial
- aspirin therapy is not a usually regarded as a contraindication to thrombolytics
severe stroke:
- in most studies of thrombolysis, prognosis and risk of haemorrhage are strongly related to the severity of stroke
- despite poorer outcomes and increased risk of haemorrhage, more patients had good outcomes with tPA than without in the NINDS trial
- severe stroke is not a contraindication to thrombolytics
general:
- an alternative approach to intravenous thrombolytics is direct delivery of thrombolytic agents by a microcatheter embedded in the clot
- the advantage is direct visualisation of the occluded artery and knowledge of the recanalisation status as thrombolysis proceeds; while
the disadvantage is the additional time required
trials:
- the PROACT II trial showed that intra-arterial thrombolysis with urokinase at up to 6 hours from the onset of symptoms
in patients with M1 or M2 segment occlusions led to improved functional outcome at 90 days; however, symptomatic
haemorrhage occurred in 10% of patients compared with 2% of controls (control group received direct arterial injection of saline)
- evidence for thrombolytics in basilar artery thrombosis comes only from case series; good outcomes have been
reported with intra-arterial thrombolysis of basilar thrombosis well beyond the usual 6 hour time limit
- 3 large double blinded placebo controlled trials of streptokinase in stroke (multicentre acute
stroke trial - Europe MAST-E ; Australian Streptokinase Trial (ASK) & the multicentre acute
stroke trial - Italy (MAST-I ))
- all three demonstrate a significant increase is risk of haemorrhage NNH to cause death or disability = 5
- involves intravenous tPA followed by angiography and intraarterial tPA if persistent thrombus is present
- in a small study, this approach lead to greater recanalisation in the combined group than the intra-arterial alone
group (81 vs 50%); however, it was associated with a slight risk of increased bleeding and the study was not
powered to lookfor differences in functional outcome
- mechanical devices have been shown to increase recanalisation rates (MERCI trial); however, clinical data are lacking at present
neuroprotectives- multiple neuroprotective agents have been trialled; however, results have been universally disappointing
- cerebral herniation is the most common cause of death from stroke in the 1st few days
- surgical decompression of large hemispheric infarcts causing oedema and can prevent
herniation and death; randomised trials have not been performed
- cerebellar infarction is a special case where surgical intervention may be clearly indicated. In these patients compression of the brainstem
and 4th ventricle leads to hydrocephalus or severe pontomedullary compromise which may be reversed by rapid surgical decompression
of the posterrior fossa leading to survival with minimal residual deficit
anticoagulation
- RCTs to date include trials of low molecular weight heparin & heparin
- overall, the studies do not show a reduced recurrence of ischaemic stroke from anticoagulation
commenced 24-48 hours after stroke & haemorrhage rates varied from 1-2.5%; even in patients
with atrial fibrillation the role of early anticoagulation is uncertain
antiplatelet
therapy
- Chinese Aspirin Stroke Trial and IST trial combined include more than 40000 patients and demonstrated
a small but significant reduction in recurrent stroke (7 per 1000) or death/dependency (12/1000) at 28 days
imaging
- evaluation of patients with acute stroke depends heavily on imaging
CT:
- CT excludes haemorrhage as the aetiology in recent stroke
- subtle abnormalities may indicate the presence of acute ischaemic stroke including subtle
hypodensity, loss of insular ribbon and hyperacute artery signs
- CT angiography also allows evaluation of vessels and may have potential to determine which patients will
benefit fromintervention (based on the burden and distribution of thrombus)although studies are currently lacking
- xenon CT can be used to determine cerebral perfusion and may identify the size of the
ischaemic penumbra; its use to guide therapy has yet to be elucidated
MRI:
- the major drawbacks of MRI are difficulty with performance on an emergent basis and the
problems with identification of hyperacute haemorrhage
- diffusion weighted imaging shows early ischaemia and in combination
with perfusion imaging may identify reversibly ischaemic tissue
- European cooperative acute stroke study (ECASS) trial was one of the first large RCTs to test rtPA administered within 6 hours of stroke onset.
Patients with clinically severe hemispheric strokes were excluded & CT was allowed to show no or early signs of ischaemia only. No difference in
outcome and increased risk of bleeding. Subgroup analysis of target population showed statistically significant benefit in favour of rtPA for good
outcome.
- ECASS-II designed with strict exclusion of patients with greater than 1/3rd MCA infarct on CTB. Also failed to demonstrate benefit - NNH to cause
haemorrhage was 18.
- NINDs was designed to assess very early rtPA (<3 hours). Total of 624 patients in 2 parts. Demonstrates NNT to have minimal or no disability at
3 months is 8. NNH to cause symptomatic ICH is 14. No significant difference in mortality (24 vs 28% respectively). No difference in outcomes
at 24 hours.
- Canadian Altepase for stroke effectiveness study which is a cohort study of all patients receiving rt-PA in Canada over a 2 and half year period
shows similar benefit to NINDs with a lower risk of ICH (only 4.6%). This study includes at total of 1135 patients An earlier metanalysis of 15
publications from post NINDs era using NINDs criteria show a stroke deficit reduction (37% achieved a very favourable outcome) similar to NINDs
but a lower risk of bleeding (5.2%). This study includes 2639 patients and results were achieved despite protocol deviations in 19.8% of patients.
- ATLANTIS part A was another North American study of rtPA which enrolled patients up to 6 hours was stopped early because of safety concerns.
Study showed increased risk of haemorrhage and no favourable outcome.
- ATLANTIS part B aimed to assess efficacy within 5 hours - results indicated no significant benefit. Subgroup
in ALTANTIS treated within 3 hours of onset had trend towards better outcome but this only constituted 62 patients.
- Metanalysis of all of the above studies (and others) with total of 5216 patient shows significant improvement in good outcome at 3 months and
significant increase in ICH](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-182-320.jpg)

![ketoacidosis
[created by
Paul Young
15/12/07]
general
- Ketoacidosis is a high anion gap metabolic acidosis due to an excessive blood
concentration of ketone bodies (keto-anions).
- Ketone bodies (acetoacetate, beta-hydroxybutyrate, acetone) are released into the blood
from the liver when hepatic lipid metabolism has changed to a state of increased ketogenesis.
- A relative or absolute insulin deficiency is present in all cases.
relationship
between
lactic
acidosis
and
ketoacidosis
- A mixed acid-base disorder may be present (eg lactic acidosis from peripheral
circulatory failure, or metabolic alkalosis from vomiting). An associated lactic acidosis
may mask the presence of the ketoacidosis. This occurs because the lactic acidosis
decreases the acetoacetate : beta-hydroxybutyrate ratio (ie more beta-hydroxybutyrate
produced ) because NAD+ is produced in the production of lactate.
- The major ketone bodies are acetoacetate and beta-hydroxybutyrate and the ratio
between these two acid anions depends on the prevailing redox state (eg as assessed by
the NADH/NAD+ ratio).
- The common test used to detect ketones (eg 'Acetest') depends on the reaction of
acetoacetate (and to a lesser extent acetone) with the nitroprusside reagent. A decreased
acetoacetate level may lead to a weak or absent test reaction despite high total levels of
total ketoanions (acetoacetate and beta-hydroxybutyrate combined) because the beta-
hydroxybutyrate is not detected.
causes
The three major types of ketosis are:
(i) Starvation ketosis
(ii) Alcoholic ketoacidosis
(iii) Diabetic ketoacidosis
starvation
ketosis
- When hepatic glycogen stores are exhausted (eg after 12-24 hours of total fasting), the
liver produces ketones to provide an energy substrate for peripheral tissues.
- Ketoacidosis can appear after an overnight fast but it typically requires 3 to 14 days of
starvation to reach maximal severity.
- Typical ketoanion levels are only 1 to 2 mmol/l and this will usually not alter the anion gap.
- The acidosis even with quite prolonged fasting is only ever of mild to moderate severity
with ketoanion levels up to a maximum of 3 to 5 mmol/l and plasma pH down to 7.3.
This is probably due to the insulin level, which though lower, is still enough to keep the
FFA levels less than 1mM. This limits substrate delivery to the liver restraining hepatic
ketogenesis. Ketone bodies also stimulate some insulin release from the islets.
alcoholic
ketoacidosis
Typical Presentation
- This typical situation leading to alcoholic ketoacidosis is a chronic alcoholic who has a
binge, then stops drinking and has little or no oral food intake. The two key factors are
the combination of ethanol and fasting.
- Presentation is typically a couple of days after the drinking binge has ceased.
Pathophysiology
- The poor oral intake results in decreased glycogen stores, a decrease in insulin levels
and an increase in glucagon levels. Hepatic metabolism of ethanol to acetaldehyde and
then to acetate both involve NAD+ as a cofactor. The NADH/NAD+ ratio rises and this:
(i) inhibits gluconeogenesis
(ii) favours the production of beta-hydroxybutyrate over acetoacetate
- The insulin deficiency results in increased mobilisation of free fatty acids from adipose
tissue. The decreased insulin/glucagon ration results in a switch in hepatic metabolism
favouring increased beta-oxidation of fatty acids. This results in an increased production
of acetylCoA which forms acetoacetate (a keto-acid).
Other features
- Volume depletion is common and this can result in increased levels of counter-
regulatory hormones (eg glucagon)
- Levels of FFA can be high (eg up to 3.5mM) providing plenty of substrate for the
altered hepatic lipid metabolism to produce plenty of ketoanions
- GIT symptoms are common (eg nausea, vomiting, abdominal pain, haematemesis, melaena)
- Acidaemia may be severe (eg pH down to 7.0)
- Plasma glucose may be depressed or normal or even elevated
- Magnesium deficiency is not uncommon
- Patients are usually not diabetic
Management
- This syndrome is rapidly reversed by administration of glucose and insulin.
- A mixed acid-base disorder may be present: high anion gap due to ketoacidosis,
metabolic alkalosis due to vomiting and a respiratory alkalosis.
diabetic
ketoacidosis
General:
- involves an absolute or relative lack of insulin leads to diabetic metabolic
decompensation with hyperglycaemia and ketoacidosis.
- A precipitating factor (eg infection, stress) which causes an excess of stress hormones
(which antagonise the actions of insulin) may be present.
- The most common situations in patients presenting with DKA are:
(i) Infection as precipitant (30% of cases)
(ii) Treatment non-compliance (20%)
(iii) New diagnosis of diabetes (25%)
(iv) No known precipitating event (25%)
Pathophysiology
- The pathogenesis requires two events:
(i) Increased mobilisation of free fatty acids (FFA) from adipose tissue to the liver
- FFA mobilisation is initiated by the effect of absolute or relative insulin deficiency on
fat cells. FFA levels can be quite high (eg 2.5 to 3.5 mM). This provides the liver with
plenty of substrate. These FFA levels are much less then ketone levels and contribute
only a small amount to the metabolic acidosis.
(ii) A switch of hepatic lipid metabolism to ketogenesis
- The major switch in hepatic lipid metabolism occurs in response not just to insulin
deficiency but additionally to the concomitant rise in levels of the stress hormones
(glucagon, corticosteroids, catecholamines, growth hormone). The role of glucagon is the
most clearly established. The hepatic effects of a fall in the insulin:glucagon ratio are
increased glycogenolysis, increased gluconeogenesis, increased ketogenesis
- The inhibition of the enzyme acetyl CoA carboxylase is probably the key step. This
enzyme is inhibited by increased FFA levels, decreased insulin levels and particularly by
the rise in glucagon.
- The effect is to decrease the production and level of malonyl CoA. This compound has
a central role in the regulation of hepatic fatty acid metabolism as is mediates the
reciprocal relationship between fatty acid synthesis and oxidation. It is the first
committed intermediate in fatty acid metabolism. Malonyl CoA inhibits fatty acid
oxidation by inhibiting carnitine acyltransferase I.
- A fall in malonyl CoA levels removes this inhibition resulting in excessive fatty acid
oxidation with excessive production of acetyl CoA and excess acetoacetate.
- The problem however is not just of hepatic over-production of glucose and ketones but
also of peripheral underutilisation of both glucose and ketones.
Development of high anion gap acidosis in DKA
- Acetoacetic acid (pKa 3.58) and beta-hydroxybutyric acid (pKa 4.70) dissociate
producing H+ which is buffered by HCO3- in the blood. For each anion produced there is
a loss of one bicarbonate. The increase in the anion gap (representing the increase in the
unmeasured acid anions) should approximately equal the decrease in the [HCO3-]. A
'pure' high anion gap metabolic acidosis results.
Development of hyperchloraemic acidosis
- In some cases, a hyperchloraemic metabolic acidosis develops: this is most common
during the treatment phase. This occurs because acetoacetate and beta-hydroxybutyrate
are moderately strong acids and even at the lowest urinary pH are significantly ionised.
They are excreted with a cation (usually Na+ or K+) to maintain electroneutrality. The net
effect is the loss of 'potential bicarbonate' equal to the level of urinary ketone body loss.
Mixed acidosis
- At presentation, both types of acidosis may be present and the elevation in the anion gap
will be less than expected for the degree of depression in the bicarbonate level (resulting
in Delta ratio < 0.8).
- A predominant hyperchloraemic acidosis (defined as a DKA patient with a delta ratio <
0.4) is present in about 10% of patients on arrival at hospital and in about 70% after 8
hours of treatment.
- Patients who are more severely dehydrated retain more keto-anions and have a lower
incidence of hyperchloraemic acidosis. Patients who have been able to maintain fluid
intake during development of their illness are more likely to have a hyperchloraemic
acidosis component present on admission
- Administration of large volumes of normal saline in resuscitation of patients with acute
DKA promotes continued diuresis (and continued loss of ketone bodies with Na+ as the
cation) and provides plenty of chloride to replace the lost ketoanions.
Other acid base disorders in DKA
- Possible complicating acid-base disorders are:
(i) Lactic acidosis due to hypoperfusion and anaerobic muscle metabolism
(ii) Metabolic alkalosis secondary to excessive vomiting
(iii) Respiratory acidosis due to pneumonia or mental obtundation
(iv) Respiratory alkalosis with sepsis
(v) Renal tubular acidosis (type 4) is present in some diabetic patients and the associated
urinary acidification defect can cause a hyperchloraemic normal anion gap acidosis. This
syndrome (known as hyporeninemic hypoaldosteronism) occurs in some elderly diabetics
who have pre-existing moderate renal insufficiency but is not a common problem in acute DKA](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-184-320.jpg)
![Klebsiella
[created by
Paul Young
02/10/07]
general
- Klebsiella species belong to the family Enterobacteriaceae that includes
Enterobacter spp., Escherichia coli, Proteus spp. and Serratia spp.
- They are non-motile, rod-shaped, usually encapsulated organisms that
are ubiquitous in nature, found both in the general environment and on
mucosal surfaces of mammals.
- Species differentiation is based on various biochemical reactions.
- Medically important species are Klebsiella pneumoniae and to a
lesser degree Klebsiella oxytoca
colonisation
& infection
- The vast majority of Klebsiella infections are nosocomial
and are typically opportunistic.
- As enteric organisms, Klebsiella spp. are involved in urinary tract infections,
peritonitis, cholangitis and intra-abdominal infections. However, because of
their ability to colonise the upper respiratory tract and the skin of critically ill
patients, they also cause pneumonia and catheter-related bacteraemia.
- The risk of colonisation and subsequent infection by Klebsiella spp. is related
to previous exposure to antimicrobials, length of hospital stay and the presence
of invasive lines, factors common to most nosocomial pathogens.
resistance
- Klebsiella spp. display a particular proclivity for acquiring plasmids.
- As a result, they are the likeliest of all the Enterobacteriaceae to
possess extended-spectrum betalactamases, which are overwhelmingly
plasmid-borne.
- Extended-spectrum beta-lactamases are able to hydrolyse third
generation cephalosporins (e.g. cefotaxime, ceftazidime, ceftriaxone)
and aztreonam.
- Extended-spectrum beta-lactamases-producing Klebsiella spp. were first
identified in the 1980s and their prevalence is increasing, most likely due
to the indiscriminate use of third generation cephalosporins.
- the presence of resistance to ceftazidime that is reversed by the addition
of clavulanic acid is suggestive of an extended-spectrum beta-lactamase.
- Plasmids carrying extended-spectrum beta-lactamases display relatively
high stability and persistence of colonisation. Extended-spectrum
beta-lactamase-producing strains can be observed years after exposure to
ceftazidime and other cephalosporins. In addition, these plasmids frequently
contain genes encoding resistance to aminoglycosides and co-trimoxazole.
- Although imipenem-resistant Klebsiellae have been documented, such strains
are fortunately still rare
therapy
- Non-extended-spectrumbeta-lactamase-producing Klebsiellae are likely to
be sensitive to awide range of agents active against Gram-negative organisms.
- These include fluoroquinolones, aminoglycosides, the antipseudomonal betalactams
(piperacillin-tazobactam, ticarcillin-clavulanic acid, cefepime, cefpirome and
ceftazidime) and often other second and third generation cephalosporins and
broadspectrum penicillins.
- The drugs of choice for extended-spectrum beta-lactamase-
producing strains are the carbapenems, imipenem and meropenem.
- Although in vitro testing may indicate susceptibility to one or more
third generation cephalosporins, the clinical outcome is poor when they
are used even in the presence of apparent susceptibility. The use of a
beta-lactam / beta-lactamase inhibitor combination such as piperacillin-tazobactam
is also not recommended for extended-spectrum beta-lactamase-producing strains
except possibly for urinary tract infections. Clinical evidence to support their
use for treatment of bloodstream infections is lacking.
- Extended-spectrum beta-lactamase-producing Klebsiellae are often resistant
to fluoroquinolones, and their prevalence is increasing. The exact mechanism for
the association is still unclear, but is thought to arise through prior exposure
to both cephalosporins and quinolones
influence of ESBL on resistance](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-185-320.jpg)
![lactic
acidosis
[created
by Paul
Young
15/12/07]
physiology
of lactate
Daily Production of Lactate
- Each day the body has an excess production of about 1500 mmols of lactate (about 20
mmols/kg/day) which enters the blood stream and is subsequently metabolised mostly in
the liver. This internal cycling with production by the tissues and transport to and
metabolism by the liver and kidney is known as the Cori cycle. This normal process does
not represent any net fixed acid production which requires excretion from the body.
- All tissues can produce lactate under anaerobic conditions but tissues with active
glycolysis produce excess lactate from glucose under normal conditions and this lactate
tends to spill over into the blood.
Relationship of lactate to pyruvate
- Lactate is produced from pyruvate in a reaction catalysed by lactate dehydrogenase:
Pyruvate + NADH + H+ <=> Lactate + NAD+
- This reaction is so rapid that pyruvate and lactate can be considered to be always in an
equilibrium situation. Normally the ratio of lactate to pyruvate in the cell is 10 to 1. The
ratio [NADH]/[NAD+] by the Law of Mass Action determines the balance between
lactate and pyruvate. This ratio is also used to denote the redox state within the
cytoplasm. Lactic acid has a pK value of about 4 so it is fully dissociated into lactate and
H+ at body pH. In the extracellular fluid, the H+ titrates bicarbonate on a one for one basis.
Tissues Producing Excess Lactate
- At rest, the tissues which normally produce excess lactate are:
(i) skin - 25% of production
(ii) red cells - 20%
(iii) brain - 20%
(iv) muscle - 25%
(v) gut - 10%
- During heavy exercise, the skeletal muscles contribute most of the much
increased circulating lactate.
- During pregnancy, the placenta is an important producer of lactate which
passes into both the maternal and the foetal circulations.
Lactate metabolism
- Lactate is metabolised predominantly in the liver (60%) and kidney (30%).
- Half is converted to glucose (gluconeogenesis) and half is further metabolised to CO2
and water in the citric acid cycle. The result is no net production of H+ (or of the lactate
anion) for excretion from the body.
- Other tissues can use lactate as a substrate and oxidise it to CO2 and water but it is only
the liver and kidney that have the enzymes that can convert lactate to glucose.
- The balance between release into the bloodstream and hepatorenal uptake maintains
plasma lactate at about one mmol/l.
- The renal threshold for lactate is about 5 to 6 mmols/l so at normal plasma levels, no
lactate is excreted into the urine. The small amount of lactate that is filtered
(180mmol/day) is fully reabsorbed.
pathophysiology
of lactic acidosis
- Lactic acidosis can occur due to:
(i) excessive tissue lactate production
(ii) impaired hepatic metabolism of lactate
- In most clinical cases it is probable that both processes are contributing to the
development of the acidosis. The liver has a large capacity to metabolise lactate so
increased peripheral production alone is unlikely to lead to other than transient acidosis.
- In situations where lactic acidosis is clearly due to excessive production alone (such as
severe exercise or convulsions), the acidosis usually resolves (due to hepatic metabolism)
within about an hour once the precipitating disorder is no longer present. In severe
exercise, lactate levels can rise to very high levels eg up to 30 mmol/l.
- A continuing lactic acidosis means that there is continuing production of lactate that
exceeds the liver's capacity to metabolise it. This may be due to clearly very excessive
production (eg convulsions) with a normal liver at one extreme, or to increased
production in associated with greatly impaired hepatic capacity to metabolise it (eg due to
cirrhosis, sepsis, hypoperfusion due hypovolaemia or hypotension, hypothermia, or some
combinations of adverse factors) at the other extreme.
definitions
& significance
- Definitions differ concerning the blood level at which a lactic acidosis is regarded as
significant' but as a guide:
Hyperlactaemia: a level from 2 mmols/l to 5 mmol/l.
Severe Lactic Acidosis: when levels are greater than 5 mmols/l
- As levels rise above 5mmols/l, the associated mortality rate can become very high.
- The brief and often very high lactate levels that occur with severe exercise or
generalised convulsions (eg up to 30 mmol/l) are associated with an extremely low
mortality rate so the absolute lactate level (alone) is not a good predictor of outcome
unless the cause of the high level is also considered.
causes
(Cohen
& Woods
classification)
Type A Lactic Acidosis : Clinical Evidence of Inadequate Tissue Oxygen Delivery
(i)Anaerobic muscular activity (eg sprinting, generalised convulsions)
(ii)Tissue hypoperfusion (eg shock -septic, cardiogenic or hypovolaemic; hypotension; cardiac
arrest; acute heart failure; regional hypoperfusion esp mesenteric ischaemia)
(iii) Reduced tissue oxygen delivery or utilisation (eg hypoxaemia, CO poisoning, severe anaemia)
- If hypoxaemia is the only factor present, it needs to be severe (eg paO2 < 35mmHg) to
precipitate lactic acidosis because of the protection afforded by the body's compensatory
mechanisms which increase tissue blood flow. Similarly anaemia needs to be severe (eg
[Hb] <5g/dl) if present alone because tissue blood flow is increased in compensation.
Type B Lactic Acidosis: No Clinical Evidence of Inadequate Tissue Oxygen Delivery
- refers to situations in which there is no clinical evidence of reduction in tissue oxygen
delivery. Carbohydrate metabolism is disordered for some reason and excess lactic acid is
formed. Research using more sophisticated methods to assess tissue perfusion have now
shown that occult tissue hypoperfusion is present in many cases of Type B acidosis.
(i) type B1 : Associated with underlying diseases
- LUKE leukaemia, lymphoma
- TIPS thiamine deficiency, infection, pancreatitis, short bowel syndrome
- FAILURES hepatic, renal , diabetic failures
(ii) type B2: Assoc with drugs & toxins (eg phenformin, cyanide, beta-agonists, methanol, adrenaline,
salicylates, nitroprusside infusion, ethanol intoxication in chronic alcoholics, anti-retroviral drugs,
paracetamol, salbutamol, biguanides, fructose, sorbitol, xylitol, isoniazid)
(iii) type B3: Assoc with inborn errors of metabolism (eg congenital forms of lactic acidosis with
various enzyme defects eg pyruvate dehydrogenase deficiency)
diagnosis
- The condition is often suspected on the history and examination (eg shock, heart failure)
and is easily confirmed and quantified by measuring the blood lactate level.
- It may be associated with other causes of a high anion gap acidosis (eg ketoacidosis,
uraemic acidosis)
- Coexistent lactic acidosis and metabolic alkalosis may result in minimally altered
plasma bicarbonate level. A high anion gap may be a clue in this later situation but the
anion gap is not invariably elevated out of the reference range
management
- The principles of management of patients with lactic acidosis are:
(i) Diagnose and correct the underlying condition (if possible)
(ii) Restore adequate tissue oxygen delivery (esp restore adequate perfusion)
(iii) Ensure appropriate compensatory hyperventilation where possible
- lactic acidosis in sepsis has been attributed to:
(i) impaired regional microvascular blood flow & autoregulation
(ii) mitochondrial dysfunction with impaired pyruvate oxidation
(iii) excess catecholamines may impair hepatic lactate extraction
(by reducing regional hepatic blood flow)
(iv) lactate clearance is decreased because pyruvate dehydrogenase activity
is reduced in both skeletal muscle and liver.
NB:
- tissue hypoxia may not be a major mechanism & NMR spectroscopy
suggests that hyperlactaemia may occur without tissue hypoxia
- net lactate production from the hepatosplanchnic bed is uncommon in sepsis
Use of bicarbonate:
- two randomised controlled studies of bicarbonate in lactic acidosis and shock
found no beneficial effects on cardiac function or any other effects of pH correction
- potential adverse effects include:
(i) acute hypercapnia
(ii) ionised hypocalcaemia
(iii) intracellular acidosis due to CO2 crossing cell membranes rapidly
(iv) acute intravascular overload
(v) bicarbonate increases lactate production by increasing the activity of the rate limiting
enzyme phosphofructokinase, shifts Hb-O2 dissociation curve, increased oxygen affinity
of haemoglobin and thereby decreases oxygen delivery to tissues
- potential indications:
(i) patients with pulmonary hypertension in whom pulmonary vasoconstriction may be
worsened by acidosis
(ii) patients with significant ischaemic heart disease in whom severe acidosis lowers the
threshold for arrhythmia
Carbicarb:
- carbicarb is an equimolar combination of sodium bicarbonate & sodium carbonate which
generates less CO2 than HCO3 & may have less adverse effects. It is not in clinical usage
Dichloroacetate:
- DCA stimulates the activity of phosphate dehydrogenase complex, the rate limiting enzyme
that regulates entry of pyruvate into the TCA cycle. It increases intracellular pH and decreases
lactate concentrations; however, a large multicentred study found no haemodynamic benefit
or improvement in patient outcome in treatment of patients with lactic acidosis
- it is not commercially available
Tris / THAM
- Tris-hydroxymethyl aminomethane is a weak alkali which is rarely used
because of concerns about side effects. Namely,
(i) hyperkalaemia
(ii) hypoglycaemia
(iii) extravasation necrosis
(iv) neonatal hepatic necrosis
Dialysis / haemofiltration:
- peritoneal dialysis is not useful in removing lactate when using bicarbonate
buffered haemofiltration; it remains a useful marker of clinical disease progression
in patients on bicarbonate buffered haemofiltration](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-186-320.jpg)
![lacunar
syndromes
[created by
Paul Young
02/10/07]
definition
aetiology
investigation
treatment
- lacunar syndromes are stroke syndromes associated with chronic
hypertension involving infarction in territories of deep penetrating arteries
- the five classical lacunar syndromes are:
1. Pure motor stroke/hemiparesis (33-50%)
2. Ataxic hemiparesis (2nd most common)
3. Dysarthria/clumsy hand
4. Pure sensory stroke
5. Mixed sensorimotor stroke
- The cause of lacunar infarction is occlusion of a single small penetrating artery. This
occlusion may be due to microatheroma and lipohyalinosis, which are associated with
hypertension, smoking, and diabetes, or to microembolism from the heart or carotid arteries1. pure motor stroke
- the lacune is usually in the posterior limb
of the internal capsule or the basis pontis
Consider TPA
- contraindications include
1) Beyond 3 h of stroke onset (or when last well)
2) CT scan evidence of recent major infarction
3) Concomitant anticoagulation (with prolonged
aPTT or PT greater than 15 s or INR greater than 1.7)
4) Platelet count <100,000/mm3
5) Documented hypersensitivity;
6) another stroke or major head injury in last 3 mo;
7) major surgery in last 14 d;
8) pretreatment systolic BP >185 mm Hg or diastolic BP >110 mm Hg
9) rapidly improving signs
10) mild deficit
11) prior intracerebral hemorrhage
12) seizure at onset of stroke
13) gastrointestinal or urinary bleeding in last 21 d
14) recent myocardial infarction
symptoms
- lacunar syndromes are characterised by an absence of
cortical signs such as neglect, visual field deficits or aphasia
Symptoms may occur suddenly or may evolve in either a fluctuating
(eg, the capsular warning syndrome) or a progressive manner.
1. Pure motor stroke
- consists of hemiparesis or hemiplegia that typically affects the face, arm, and leg
equally; however, the face or leg can be involved to a lesser extent than other regions,
and occasionally only arm or leg weakness is noted.
- transient sensory symptoms (but not signs) may be present.
- dysarthria and dysphagia also may be present.
2. Ataxic hemiparesis
- weakness and clumsiness on one side of the body
- usually affects the leg more than the arm
- the onset of symptoms is often over hours or days.
2. Ataxic hemiparesis & 3. dysarthria / clumsy hand
- The most frequent sites of infarction are the posterior limb
of the internal capsule, basis pontis, and corona radiata.
CT scan is appropriate initial investigation; may require MRI
3. dysarthria/ clumsy hand
- main symptoms are dysarthria and clumsiness of hand which
is most prominent when patient is writing
4. pure sensory stroke
- main symptoms are tingling, numbness or occasionally pain on one side of the body
4. pure sensory stroke
- lesion is usually in the thalamus
5. mixed sensorimotor stroke
- hemiparesis of hemiplegia with sensory abnormality on the same side
5. mixed sensorimotor stroke
- The infarct is usually in the thalamus and adjacent posterior internal
capsule (seemingly, in both the carotid and vertebrobasilar territories).
signs
2. Ataxic hemiparesis:
A combination of pyramidal signs (eg, hemiparesis, hyperreflexia,
Babinski sign) and cerebellar ataxia on the same side of the body
often involves the leg more severely than other parts of the body.
Nystagmus may be present.
1. Pure motor stroke/hemiparesis:
Hemiparesis or hemiplegia is noted with hyperreflexia and Babinski sign,
but no involvement of any other system is observed
3. Dysarthria-clumsy hand
- Unilateral lower facial weakness with dysarthric speech is noted.
On protrusion, the tongue may deviate to the side of facial weakness.
A mild ipsilateral hemiparesis usually is noted, but the arm is ataxic.
Ipsilateral hyperreflexia and Babinski sign may be observed.
4. Pure sensory stroke
- Unilateral sensory loss is observed. Although the patient may
complain of weakness, no weakness is found on examination.
5. sensorimotor stroke
- A combination of pyramidal signs (eg, hemiparesis, hyperreflexia,
Babinski sign) and sensory signs without cortical signs
other investigations include:
- immediated blood glucose to rule out hypoglycaemia
- coags & FBC
commence on aspirin & statin
treat risk factors](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-187-320.jpg)
![laryngeal
& tracheal
injury
[created
by Paul
Young
11/12/07]
general
- direct trauma to the airway is rare accounting for less
than 1% of traumatic injury seen in most major centres
- the bony protection afforded to the airway by the sternum and mandible and
death from asphyxia at the accident scene account for the rarity of the injury
mechanism
of injury
blunt injury:
- common causes include motor vehicle accidents where the extended neck impacts
with the steering wheel or dashboard
- the 'clothes line injury' occurs when a cyclist or horserider collides with a cable or
wire causing direct injury to the upper airway; assaults and strangulation account for
the remainder of injuries
- direct blows are more likely to injure the cartilages of the larynx while flexion/extension
injuries are most commonly associated with tracheal tears and laryngotracheal transection
- larynx above the cricoid is injured in 35% manifesting as oedema, contusions, haematomas,
lacerations, avulsion and fracture dislocation, most commonly of the thyroid and arytenoid
cartilages
- the cricoid cartilage itself is injured in 15% which may cause recurrent laryngeal nerve
dysfunction
- the cervical cartilage itself is injured in 45% with tracheal transection occurring most often
at the junction of the cricoid and the trachea. Oedema fluid and air dissecting within submucosal
layers of the larynx and trachea may cause airway obstruction. Air in the soft tissues can cause
epiglottic emphysema and narrowing of the supraglottic airway in which case straining, talking
& coughing may worsen the oedema
penetrating injury
- usually results from stab and gunshot wounds
- the anterior triangle of the neck is the most common involved in stab wounds
- the larynx is injured in 1/3rd of those with upper airway injuries
associated injuries:
- common associations with blunt laryngotracheal injury include:
(i) cervical spine
(ii) head injury
(iii) multisystem trauma
- of those with penetrating neck trauma, major vascular injuries (carotid, jugular, subclavian,
& vertebral arteries) occurs in 25-50%, pharnygeal and or oesophageal injuries occur in 30%,
neural injury (spinal cord, brachial plexus) in 12% and apical thoracic injury in 10%
assessment
general:
- definitive investigation and management depend on
the airway status and presence of associated injury
- the degree of injury is not readily assessable on the basis of any
one clinical symptom or sign and delayed diagnosis is common
clinical features:
(i) symptoms
- respiratory distress
- hoarseness
- dysphonia
- cough
- stridor, noisy breathing
- dysphagia
(ii) signs
- abnormal laryngeal contour
- subcutaneous emphysema
- cervical ecchymosis
- haemoptysis
investigation
plain radiography may demonstrate
(i) air in soft tissues
(ii) pneumomediastinum
(iii) pneumothorax
(iv) cervical spine fracture
- CT scanning demonstrates
(i) fractures of the cartilages
(ii) haematomas
- it is used in stable patients with laryngeal tenderness,
endolaryngeal oedema & small haematomas
fibre optic laryngotracheostomy
- can demonstrate vocal cord dysfunction, integrity
of the cartilagenous framework & larygneal mucosa
rigid laryngoscopy
- can be used when adequate visualisation is not achieved with fibreoptics
others:
- pharyngo-oesophagoscopy, contrast studies, open exploration & angiography
may be required to exclude aerodigestive tract & major vascular injuries
airway
management
- Airway management in patients with neck trauma is based upon a high
index of clinical suspicion for cricoid or cervical tracheal injuries. Attempts at
endotracheal intubation in patients with unsuspected cricoid injuries can be
disasterous. Cricoid pressure or the attempted passage of an endotracheal
tube may dislocate a fractured cricoid cartilage and/or entirely disrupt a partial
tracheal transection, producing complete airway obstruction.
- The equipment and personnel required to perform an immediate tracheostomy
must be present prior tomanipulation of an injured airway.
- Positive pressure ventilation can exacerbate air leaks and rapidly worsen
symptoms from pneumothorax, pneumomediastinum, and air dissecting
around airway structures. Whenever possible, the patient should be permitted
to breathe spontaneously.
- Rapid induction of anesthesia and neuromuscular blockade can rapidly produce
loss of the airway and the inability to provide positive pressure ventilation.
- Attempts at direct laryngoscopy or intubation over a flexible bronchoscope
may be futile because of bleeding within the airway or distortion of anatomic
structures. The danger also exists that flexible bronchoscopy may occlude the
airway or precipitate airway obstruction in patients with critical airway stenosis.
- Under ideal circumstances, pre-oxygenation followed by awake flexible bronchoscopy
may permit evaluation of airway injuries and safe endotracheal intubation.
- Prior induction of general anesthesia, using a potent inhalation anesthetic
such as sevoflurane, while maintaining spontaneous ventilation, may be appropriate
in some patients. This approach can permit rigid laryngoscopy and rigid bronchoscopy
while maintaining spontaneous ventilation. These techniques may be preferable when
bleeding or debris obscure the airway, making fibreoptic examination impossible. If
endotracheal intubation appears unwise and the patient is unstable or the airway is lost,
immediate tracheostomy is the only appropriate choice.
- When the trachea itself is injured, it is preferable to conserve normal trachea by placing the
tracheostomy through the damaged area. This will facilitate subsequent surgical repair of the
trachea](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-188-320.jpg)
![Laryngeal
mask airway
[created by
Paul Young
22/12/07]
features
- made of medical-grade latex-free silicone rubber
- has three main components:
1) an airway tube which has a 15mm standard male adapter
2) a mask with a specially shaped cuff
3) a mask inflation line with a inflation indicator balloon & valve
- the mask is designed to conform to the contours of the hypopharynx
with its lumen facing the laryngeal opening
general
an airway control device that was introduced in the
UK in 1988 & became available in the USA in 1992
when inserted correctly the LMA occupies the entire
hypopharynx and rests against the upper oesophageal
sphincter behind the cricoid cartilage at the level of C6.
The sides of the device face into the piriform fossae and
the upper border rests against the base of the tongue
indications
1. lack of expertise for endotracheal intubation
2. failed intubation
success at placement of LMA is unaffected by
Mallampati score or presence of a hard collar
sizes
size 1 - neonates up to 5kg
size 1 1/2 - infants 5-10 kg
size 2 - infants / children 10-20 kg
size 2 1/2 - children 20-30kg
size 3 - children heavier than 30kg and small adults
size 4 - normal and large adults (cuff volume 30ml)
size 5 - large adults (cuff volume 40ml)
contraindications1. prolonged positive pressure ventilation
LMA proseal
Features:
(i) Drain tube allows easy clinical confirmation of correct mask position
(ii) Drain tube provides direct access to stomach contents and prevents
gastric insufflation providing an escape for unexpected regurgitation
(iii) High seal pressure - up to 30 cm H20 - Providing a tighter seal against
the glottic opening with no increase in mucosal pressure
(iv) Provides more airway security than regular LMA
insertion
soft palate teeth
tongue
larynx
esophagus
trachea
soft palate teeth
tongue
larynx
esophagus
trachea
(i) Prepare LMA (deflate – more stable, rigid, less risk of kinking)
(ii) Stabilize head and place Index finger between tube and cuff
(iii) Push down until soft resistance (tip in upper oerophageal sphincter
(iv) Inflate cuff (LMA normally comes back 1 cm)](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-189-320.jpg)

![Legionella
[created by
Paul Young
02/10/07]
definition
aetiology
symptoms
signs
investigations
treatment
Legionella pneumophila is a common cause of
community acquired pneumonia & accounts for 2-15%
of all community acquired pneumonia; it is also a cause
of nosocomial pneumonia
risk factors are:
1. smoking
2. chronic lung disease
3. immunosuppression (esp with corticosteroids)
4. surgery is the major risk factor for nosocomial infection
with transplant recipients at the highest risk
transmitted for inhalation of aerosols containing Legionella
or microaspiration of water contaminated with Legionella
may be contracted from handling contaminated
soil or from contaminated air conditioners
a disease caused by Legionella pneumophila which
causes clinical illness rangeing from mild cough and
low-grade fever to stupor, respiratory failure and MOF
early symptoms include:
- fever
- malaise
- myalgias
- anorexia
- headache
temperature often exceeds 40
cough is only slightly productive; may be haemoptysis
chest pain may be prodominant and can be pleuritic
GI symptoms are prominent with
watery diarrhoea occuring in 40%
clinical signs of pneumonia - often bilateral
Bloods:
- hyponatraemia is more common than other forms of pneumonia
- CK is often elevated
- LFTs may be mildly deranged
extrapulmonary Legionella causing myocarditis, pericarditis,
prosthetic endocarditis, sinusitis, cellulitis, pancreatitis,
peritonitis & pyelonephritis have all been described
CXR
- symptoms may precede CXR infiltrate
- 1/3rd of patients have pleural effusion
- immunosuppressed patients (esp those on steroids)
develop distinctive nodular opacities which expand & cavitate
Special tests:
1. urinary Legionella Ag
- only detects serogroup 1
- sensitivity is 70% & specificity approaches 100%
2. Legionella serology
- requires acute and convalescent specimen
3. PCR on BAL
4. direct staining
Sputum specimen
- diagnosis is suggested by leucocytes with an
absence of organisms seen on gram stain
1. antibiotic therapy
- erythromycin is historically drug of choice but
newer macrolides (esp azithromycin) have superior
in vitro activity and tissue penetration. Azithromycin,
clarithromycin & roxithromycin have all been used
- quinolones are effective and given interaction of
macrolides with immunosuppressives, they are first
choide in transplant patients
- therapy can be changed to oral when patient is afebrile
for 48hrs. Total therapy should be 10-14 days. 21 days
is recommended for severe disease and in immunosuppressed
patients](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-191-320.jpg)


![life threatening
cutaneous drug
reactions
[created by
Paul Young;
03/10/07]
general
- Adverse cutaneous reactions to drugs are frequent, affecting 2% to 3%
of all hospitalized patients. Fortunately, only about 2% of adverse
cutaneous reactions are severe and very few are fatal
classification
- The clinical pattern of the individual skin lesion is classified into 4 types:
1. Typical targets:
- individual lesions less than 3 cm in diameter with a regular round shape,
well-defined border, and at least 3 different zones, that is, 2 concentric rings
around a central disk. One ring consists of palpable edema, paler than the center
disk.
2. Raised atypical targets:
- round, edematous, palpable lesions, similar to EM but with only 2 zones and/or
a poorly defined border.
3. Flat atypical targets:
- round lesions characteristic of EM but with only 2 zones and/or a poorly defined
border and nonpalpable with the exception of a potential central blister.
4. Macules with or without blisters:
- nonpalpable, erythematous, or purpuric macules with an irregular shape and size
and often confluent. Blisters often occur on all or part of the macule.
1. Bullous erythema multiforme:
- detachment less than 10% of BSA, localized typical targets or raised atypical targets.
2. Stevens Johnson Syndrome:
- detachment less than 10% of BSA, widespread
erythematous or purpuric macules of flat atypical targets
3. Overlap Stevens Johnson Syndrome / toxic epidermal necrolysis:
- detachment between 10% and 30% of BSA, widespread purpuric macules or flat atypical targets.
4. toxic epidermal necrolysis with spots:
- detachment greater than 30% of BSA, widespread purpuric macules or flat atypical targets.
5. toxic epidermal necrolysis without spots:
- detachment greater than 10% of BSA, large epidermal sheets and no purpuric macules.
- The involved BSA should measure the extent of detached and detachable epidermis (which
is often much less than the area of erythema) at the worst stage of the disease
clinical
manifestations
- The initial symptoms of TEN, that is, before the appearance of frank
mucocutaneous sloughing, include:
(i) fever (all cases)
(ii) conjunctivitis (32% of cases),
(iii) pharyngitis (25% of cases), and
(iv) pruritus (28% of cases).
- The cutaneous lesions begin with a burning and painful eruption.
- This eruption extends symmetrically from the face and upper part of the
body to the entire body, predominantly on the trunk and proximal limbs.
- The initial lesions are poorly defined macules with darker centers.
- Maximal extension of lesions usually occurs in 2 or 3 days, but can be
manifested in a few hours. There is a sheet like loss of epidermis and the
appearance of flaccid blisters that spread with pressure in TEN.
- Nikolsky's sign is positive over large areas involved by confluent erythema.
- Mucous membranes (in increasing order of frequency: oropharynx,
eyes, genitalia, anus) are commonly affected 1 to 3 days before the
skin lesions appear.
- Widespread painful mucosal erosions result in impaired alimentation,
photophobia, and painful micturition.
- Gastrointestinal or tracheobronchial epithelium can be involved via a process
of necrosis resulting in profuse diarrhea or respiratory distress, respectively,
and causing high morbidity.
- Blood abnormalities are also almost always present. Anemia and lymphopenia are
found in virtually all patients, neutropenia in 30% of patients (indicating a poor
prognosis), and thrombopenia in 15% of patients.
- Fluid losses are massive and accompanied by with electrolyte imbalance.
- During the first days, skin lesions are usually colonized by Staphylococcus
aureus; they are later invaded by gram negative rods.
- Thermoregulation is impaired and energy expenditure is increased.
- Re-epidermization begins after a few days, and most of the skin surface is
re-epithelialized in 3 weeks.
causative
drugs
- More than 100 drugs have been associated with the development of SJS/TEN
- Sulfonamides are the most strongly associated with TEN
followed by antibiotic drugs (in descending order of frequency:
cephalosporins, quinolones, aminopenicillins, tetracyclines, macrolides),
imidazole antifungals, anticonvulsants (phenobarbital, phenytoin, valproic
acid, carbamazepine, and lamotrigine), then nonsteriodal anti-inflammatory
drugs (especially oxicam), allopurinol, and others.
- the risk for developing TEN is largely confined to the start of
antiepileptic therapy, that is, within the first 8 weeks, after which it
was not associated with an increased risk. The incubation time for all
other drugs varies from a few days to 2 to 3 weeks, but may be up
to 1 month.
treatment
- More than 100 drugs have been associated with the development of SJS/TEN
- Sulfonamides are the most strongly associated with TEN
followed by antibiotic drugs (in descending order of frequency:
cephalosporins, quinolones, aminopenicillins, tetracyclines, macrolides),
imidazole antifungals, anticonvulsants (phenobarbital, phenytoin, valproic
acid, carbamazepine, and lamotrigine), then nonsteriodal anti-inflammatory
drugs (especially oxicam), allopurinol, and others.
- the risk for developing TEN is largely confined to the start of
antiepileptic therapy, that is, within the first 8 weeks, after which it
was not associated with an increased risk. The incubation time for all
other drugs varies from a few days to 2 to 3 weeks, but may be up
to 1 month.
- Both SJS and TEN are life-threatening diseases,
and so the management of patients must be prompt.
- Early diagnosis with the early recognition and withdrawal of all
potential causative drugs is essential to a favorable outcome.
- Morbidity and mortality decrease if the culprit drug is withdrawn
no later than the day when blisters of erosions first occurred.
- The patient must be transferred to an intensive care unit or a burn center. Prompt
referral reduces risk of infection, mortality rate, and length of hospitalization.
- The main types of symptomatic treatment are the same as for burns, and the
experience of burn units is helpful for the treatment of TEN: environmental temperature
control, careful and aseptic handling, sterile field creation, avoidance of any adhesive
material, and maintenance of venous peripheral access distant from affected areas.
- The early fluid requirement of TEN patients are two thirds to three
fourths of those of patients with burns covering the same area.
- Intubation and mechanical ventilation are nearly always
necessary if the trachea and bronchi are involved.
- Patients require ophthalmology review early and frequently
- There is no consensus about topical care. Topical antiseptics (0.5% silver nitrate or
0.05% chlorhexidine) are usually used to paint, bathe, or dress the patients. Silver
sulfadiazine, which is very popular in burn units, should be avoided because sulfonamides
are frequently implicated in the etiology of TEN
- Dressings may be gauzes with petrolatum, silver nitrate, polyvidone iodine,
hydrogels, Hydrone, Vigilon (semipermeable dressings), SoftSorb, and others
that can also be impregnated with silver nitrate.
- Corticosteroids have for years been the mainstay therapy for TEN and SJS
There are no randomized clinical trials on the use of corticosteroids in the treatment
of these life-threatening diseases.
- IVIG has been used](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-194-320.jpg)




![Ludwig's
angina &
other deep
tissue
infections
of the neck
[created by
Paul Young
02/10/07]
defn
- Ludwig's angina describes inflammation of the submandibular space which usually begins in the
submaxillary space & spreads to the sublingual space via the fascial planes not the lymphatics
- other deep neck infections include those of the:
1. pharyngeal space
2. retropharyngeal space
3. prevertebral space
4. danger space
5. masticator space
6. carotid space
7. pretracheal space
8. peritonsillar space
9. parotid space
10. temporal space
symptoms
symptoms related to deep space neck infection are:
1. pain
2. respiratory difficulties
3. dysphagia
signs
- physical examination should focus on determining the location of the infection,
the deep spaces involved and any potential functional compromise or complications
- most consistent signs of a deep neck space infection are:
1. fever
2. elevated WCC
3. tenderness
- other signs depend on location and include:
1. asymmetry of neck & associated neck masses or lymphadenopathy
2. medial displacement of lateral pharyngeal wall &
tonsil caused by parapharyngeal space involvement
3. trismus caused by inflammation or the pterygoid muscles
4. torticollis and decreased range of motion of the
neck caused by inflammation or paraspinal muscles
5. fluctuance (may not be palpable because of deep neck location & extensive
overlying soft tissues)
6. possible neural deficits (particularly of cranial nerves) - eg hoarseness from
vocal cord paralysis with carotid sheath & vagal involvement & Horner's syndrome
from involvement of the cervical sympathetic chain
7. regular spiking fevers (may suggest internal jugular vein thrombophlebitis & septic
embolisation - Lemieres syndrome)
8. tachypnoea & shortness of breath (may suggest pulmonary complications
& warn impending airway obstruction)
aetiology
- tonsillar & pharyngeal infections
- dental infections or abscesses
- oral surgical procedures
- salivary gland infection or obstruction
- trauma to the oral cavity & pharynx
- foreign body aspiration
- cervical lymphadenitis
- brachial cleft abnormalities
- thyroglossal duct cysts
- thyroiditis
- IV drug use
- mastoiditis & Bezold abscess
investigation
1. Bloods:
- Blood chemistries
- FBC
- clotting profile
2. microbiology
- blood cultures in septic patients
- abscess cultures with gram stain
3. imaging:
- lateral soft tissue X-rays of the neck
- mandible series (with particular attention to
the 2nd and 3rd mandibular molars because
the apices of these teeth extend below the mylohyoid
giving them access to the submandibular space)
- CXR: to evaluate mediastinum, check for subcut air
or pneumomediastinum or concurrent pneumonia
suggesting aspiration or Lemieres syndrome
- CT scanning
treatment
1. airway is first priority
2. obtain cultures whereever possible
3. volume resuscitation
4. choose parenteral antibiotics most likely to cover causative organisms
(depending on local sensitivities)
5. incision & drainage if indicated
common organisms are:
- S. pyogenes
- S. viridans
- S. pneumoniae
- S. aureus
- Fusobacterium nucleastum
- Bacteroides oralis
- Spirochaeta
- Peptostreptococcs
- Neisseria spp
- Pseudomonas, E.coli & H. influenzae](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-199-320.jpg)


![magnesium
disorders
[created by
Paul Young
16/12/07]
causes
of
hypomagnesaemia
manifestations
of severe
deficiency
general
- Magnesium (Mg) is involved in more than 300 enzymatic reactions and is essential for life.
- Magnesium deficiency has been reported in 20% to 65% of patients in an intensive care unit (ICU) setting
- Patients who develop Mg deficiency in the ICU have mortality rates 2 to 3 times higher and prolonged
hospitalization compared with those who are not Mg deficient.
- Mg deficiency has been proposed to cause hypertension, neuromuscular
hyperexcitability, bronchial airway constriction, coronary vasospasm, and seizures.
therapeutic
uses of
magnesium
(i) Acute Myocardial Infarction
- Three major trials define our understanding to date regarding Mg therapy in AMI: the
Second Leicester Intravenous Magnesium Intervention Trial (LIMIT- 2), the Fourth
International Study of Infarct Survival (ISIS-4) and the Magnesium in Coronaries
(MAGIC) Trial.
- The overall evidence from clinical trials does not support the routine application of
adjunctive Mg therapy in patients with AMI. Prior studies may have shown benefit, but
they were smaller and possibly more prone to type I statistical errors of chance. Both the
ISIS-4 and MAGIC Trials were large in number, and both found no benefit of adjunctive
Mg therapy.
magnesium
homeostasis
- Magnesium is the second most abundant intracellular cation, potassium being the first.
- The normal adult total body Mg content is approximately 25 g (2000 mEq or 1 mol)
- About 53% of total Mg stores are in bone, 27% in muscle, 19% in soft tissues, 0.5% in
erythrocytes, and 0.3% in the serum
- serum Mg concentration is the most common form of assessing Mg status. However,
because serum only contains 0.3% of the total body Mg, it is a poor reflection of total
body Mg content.
- Magnesium homeostasis involves the kidney, small bowel, and bone. Absorption occurs
along the entire intestinal tract but primarily occurs along the jejunum and ileum..
- From 30% to 50% of dietary Mg is absorbed under normal dietary conditions.
- The kidney is the primary site of Mg homeostasis.
Importance
of Magnesium
- Magnesium may be required for substrate formation, as an allosteric activator of
enzyme activity, and for membrane stabilization.
- Adenylate cyclase and the sodium-potassium-adenosine triphosphatase (Na, K,
ATPase) are enzymes that are critically dependent on Mg.
- Magnesium is hypothesized to play a role in sepsis and shock
- By regulating smooth muscle tone, Mg may play a role in critical illnesses such as acute
myocardial infarction (AMI), acute cerebral ischemia, and asthma exacerbation. Smooth
muscle tone is determined by calcium-dependent phosphorylation of myosin light chain.
(ii) Acute Cerebral Ischemia
- In theory, Mg antagonizes many of the processes known to lead to the death of the
penumbra, the low blood flow area surrounding a region of acute ischemia.
- Human studies on Mg therapy and acute cerebral ischemia have been few in number
and small in size. A systematic review of 4 trials suggested a reduction in the end point of
death or dependence, but the small numbers failed to reach statistical significance
(odds ratio: 0.67, 95% confidence interval: 0.35-1.26).
- A large trial, the Intravenous Magnesium Efficacy in Stroke (IMAGES) Trial, enrolled
several thousand participants and randomized them to receive Mg or placebo within
12 hours of stroke with limb weakness. This trial showed no benefit from magnesium
in acute ischaemic stroke and thus it cannot be recommended
(iii) Asthma
- The use of Mg as adjunctive therapy in asthma was originally proposed in 1936;
however, the use of intravenous Mg therapy for acute asthma exacerbations has
shown conflicting results in clinical trials.
- The results of a large trial with varying degrees of illness severity did not show any
benefit of Mg therapy. However, several studies focusing on the most severe cases of
asthma exacerbation found benefit. More clinical studies specifically examining the ICU
patient are needed.
(iv) Preeclampsia
- The MAGPIE Trial was the largest trial to date examining hypertensive disease in
preeclamptic women. More than 10,000 women with preeclampsia were randomized to
receive Mg therapy or placebo. The Mg therapy group experienced eclampsia
significantly less than the placebo group (0.8% vs 1.9%; relative risk: 0.42, 95%
confidence interval: 0.29-0.60). Moreover, the relative risk for death in the Mg therapy
group was lower (relative risk: 0.55, 95% confidence interval: 0.26-1.14).
- Magnesium therapy is clearly indicated for women with preeclampsia. It has been
shown to decrease the incidence of eclampsia and likely decreases overall mortality.
- The MAGPIE Trial administered 16 mmol initially, followed by 4 mmol per hour in
women with preeclampsia
(v) torsade de pointes
- For torsade de pointes, the ACLS Guidelines recommend a loading
dose of 8mmol of Mg over 15 minutes followed by 4mmol an hour
hypermagnesaemia
- Caution should be taken with Mg therapy in patients with any degree of renal failure. If
a decrease in glomerular filtration rate exits, the dose of Mg should be halved, and the
serum Mg concentration must be monitored daily.
- Signs of Mg intoxication occur at Mg levels greater than 1.5-2.0mmol/L and include
hypotension, flushing, nausea, lethargy, and decreased deep tendon reflexes.
- Marked muscle weakness, decreased respiration, and cardiac arrest may occur at very
high serum Mg concentrations, greater than 4 to 5 mmol/L.
- Intravenous calcium (100-200 mg over 5-10 minutes) antagonizes the severe effect of
Mg intoxication. In mild cases, discontinuation of Mg therapy will suffice.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-202-320.jpg)


![intracranial
hypertension
management
[created by
Paul Young
26/11/07]
general
management
- The principles guiding management are:
(i) optimize perfusion, oxygenation, and venous drainage;
(ii) minimize brain metabolic demands; and
(iii) avoid interventions that may exacerbate the ionic or osmolar gradient.
head
& neck
positioning
- Head position should be neutral, and any form of compression of the jugular veins should be avoided. Adhesive tapes used to secure
the endotracheal tube in place should not be tightly attached to the sides of the neck. Subclavian venous access may be preferred
over jugular sites. If it is necessary to turn the head during a procedure, this must be done with caution and for the shortest time possible.
- The practice of head elevation to reduce brain edema is widespread but only supported by inconsistent data.
- ICP tends to be lower when the head of the bed is raised to 30 degrees compared with the horizontal position. However, the effect of head elevation on
cerebral perfusion pressure is less predictable. In various studies, cerebral perfusion pressure was found to be slightly increased, unaltered, or reduced
after head elevation.
sedation
& analgesia
general
- Pain, anxiety, and agitation increase brain metabolic demands, cerebral blood flow, and at times also ICP. Therefore, a rational
regimen of analgesia and sedation is appropriate in most patients with cerebral edema who present these symptoms.
- However, along with sedation, it is important to identify and effectively treat potential underlying causes of agitation, such as
pain, bladder distension, bronchial secretions, or inappropriate ventilation.
- Opiates, benzodiazepines, and propofol are the most commonly used agents to achieve sedation
(iii) propofol
- Propofol is a very useful agent because it provides effective sedation that can be easily controlled and quickly reversed.
Duration of action becomes longer as fat deposits get saturated with continuous use, but rapid reversibility may be maintained
if the infusion rate is titrated down accordingly.
- propofol has anticonvulsant activity and decreases cerebral metabolic rate
(ii) benzodiazepines
- Benzodiazepines are less expensive than propofol and have the advantage of inducing amnesia, as well as sedation. Midazolam has very short
action when a few doses are administered intermittently, but sedative effects persist much longer as long-acting metabolites begin to accumulate.
- benzodiazepines have both anticonvulsant properties and decrease cerebral metabolic rate
(i) opioids
- Fentanyl and sulfentanyl must be used with caution because they have been associated with increases in ICP in patients with severe
brain trauma, although this may be avoidable with careful dose titration.
- On the positive side, morphine sulfate is extremely effective in controlling symptoms of excessive autonomic arousal ("autonomic storms").
intubation
& ventilation
- Hypoxia and hypercapnia are potent cerebral vasodilators; thus, they may lead to augmented cerebral blood volume and
consequent elevation of intracranial hypertension, particularly in patients with abnormal capillary permeability.
- Intubation and mechanical ventilation are indicated if ventilation or oxygenation is insufficient in patients with brain edema.
- Special caution must be exercised during endotracheal intubation to avoid an additional rise in ICP due to worsening hypoxia
and hypercapnia and reflex responses triggered bydirect tracheal stimulation. Adequate preoxygenation and use of rapid-sequence protocols
may minimize compromise of gas exchange. Intravenous lidocaine (1 mg/kg), etomidate(0.1- 0.5 mg/kg), or thiopental (1-5 mg/kg) may be
used to avert detrimental reflex responses
- Once the patient is intubated, ventilator settings should be adjusted to maintain normal PO2 and PCO2.
- Concerns about detrimental effects of positive-end expiratory pressure (PEEP) on ICP are theoretically sound, but negative
consequences are almost never seen in practice. Thus, PEEP should be used as needed to improve hypoxia.
- Intensive bronchial toileting is important to prevent complications from atelectasis and pneumonia. However, it should be performed cautiously to avert the
occurrence of marked rises in ICP that may occur during suctioning. Administering a bolus of intravenous lidocaine prior to introducing the suctioning catheter
is an effective preventive strategy. Brief periods of hyperventilation with 100% oxygen in anticipation of tracheal manipulation are also helpful in blocking ICP
elevations.
prevention
of seizures,
hyperthermia
& hyperglycaemia
- These various factors may be considered together because they all cause deleterious
effects in the injured brain and should be prevented or aggressively treated when present.
- The benefit of prophylactic use of anticonvulsants remains unproven in patients with most conditions leading to brain edema. However, this preventive
use is quite common in practice and may be defensible in patients with very limited intracranial compliance. Also, there is some evidence that subclinical
epileptic activity may be associated with progression of midline shift and worse outcome at least in critically ill patients with intracerebral hemorrhage.
- Fever and hyperglycemia worsen ischemic brain damage and may markedly exacerbate cerebral edema.
osmotic
therapy
-Mannitol and hypertonic saline are the 2 osmotic agents most extensively studied and most
frequently used in practice to ameliorate brain edema and intracranial hypertension.
- Both are effective regardless of the pathophysiology and distribution of edema.
(i) Mannitol
- Despite its widespread use for over 40 years, the precise mechanisms of action of mannitol remain incompletely defined.
- The osmotic effect is based on the fact that mannitol does not cross the cellular membrane or the intact blood-brain barrier. Hence, mannitol increases intravascular
tonicity, thereby establishing a concentration gradient across the blood-brain barrier that forces movement of water from the edematous brain tissue to the intravascular
space. This is followed by rapid renal excretion of mannitol and water.
- It has also been experimentally shown that the decline in ICP precedes the fall in brain water content that occurs after a bolus
of mannitol, arguing in favor of a mechanism other than dehydration being responsible for the early effects of the agent.
- The incomplete understanding of the mechanisms underlying the effects of mannitol on ICP and the lack of systematic studies of
mannitol treatment in humans explain the lack of agreement on what is the optimal way of administering the agent.
- A standardized dosing regimen (eg, 1 to 1.5 g/kg of 20% mannitol in a bolus followed by 0.25 to 0.5 g/kg every 4 to 6 hours) may be complicated by volume depletion.
There is also concern about possible leakage of mannitol into damaged brain tissue potentially leading to "rebound" rises in ICP. In fact, accumulation of mannitol in
white matter has been reported after multiple doses, but not after a single dose, of the medication.
- A serum osmolality of 320 mOsm/L is generally quoted as the maximal allowable serum osmolality when the patient is receiving mannitol. However, it
is important to understand that this cutoff number is a limitation designed to prevent renal tubular damage based on very limited evidence.
(ii) Hypertonic Saline
- As is the case with mannitol, various and possibly interacting mechanisms may be responsible for the reduction in brain edema
and ICP achieved with hypertonic saline. They include:
1. osmotic dehydration of the brain,
2. decreased blood viscosity,
3. increased regional brain perfusion from endothelial cell dehydration and possible pial artery vasodilatation,
4. enhanced cardiac output and, to a lesser degree, mean arterial pressure,
5. attenuation of inflammatory responses at the microcirculatory level, and reduction of
extravascular lung volume, facilitating improvement in gas exchange and oxygenation.
- Animal models of focal brain injury have demonstrated significant decreases in cerebral water content and ICP with the use of hypertonic solutions.
In these studies, hypertonic saline has resembled mannitol in that water content is preferentially reduced in the noninjured hemisphere.
Mannitol vs hypertonic saline
- Experimental designs comparing hypertonic saline with mannitol have offered conflicting results. Brain water content was reduced more effectively
by hypertonic saline in studies of focal hemorrhage and ischemia but not in others models. The duration of ICP reduction may be
longer with hypertonic saline, but this difference may be restricted to the first bolus and disappear with repeated doses.
- Clinical data on hypertonic saline is promising but far from definitive. Initial enthusiasm for this treatment was fueled by experimental data and
small clinical trials using hypertonic saline for volume resuscitation in hemorrhagic shock that showed an improvement in survival attributed to
reduction in ICP. However, in a larger recent trial,hypertonic saline was compared with conventional fluid management (lactate Ringer) for the
prehospital resuscitation of patients with severe brain trauma and hypotension, and it failed to improve neurologic outcome. Preferential benefit
in patients with trauma or postoperative edema (against no detectable benefit on lateral displacement in patients with nontraumatic intracranial
hemorrhage or infarction) was reported in one study, but hypertonic saline has also been effective in reducing ICP in patients with severe SAH
- Several small randomized trials comparing hypertonic saline with mannitol in head injury have shown better results with hypertonic saline.
However, no definite conclusions can be drawn at present because the studies involved a wide range of saline concentrations, and equiosmolar
solutions were not consistently used. Further carefully designed studies comparing the 2 agents are needed before superiority of one of them can
be firmly postulated.
- Concentrations of hypertonic saline ranging from 3% to 23.4% have been used in clinical studies. Combinations with dextran, hydroxyethyl
starch, and acetate have been tested. Continuous infusion and intermittent boluses have been evaluated. However, comparisons of all these
various options are not available, and therefore there is no clear information on what may be the ideal form of administration of hypertonic saline.
steroids
(i) brain tumours
- Glucocorticoids are very effective in ameliorating the vasogenic edema that accompanies tumors, inflammatory conditions,
and other disorders associated with increased permeability of the blood-brain barrier, including surgical manipulation.
- Dexamethasone is the preferred agent due to its very low mineralocorticoid activity. The usual initial dose is 10 mg
intravenously or by mouth, followed by 4 mg every 6 hours. This is equivalent to 20 times the normal physiologic
production of cortisol. Responses are often prompt and remarkable, sometimes dramatic, but some tumors are less responsive
- Corticosteroids are also effective to alleviate brain edema related to brain radiation, radiosurgical treatments, and neurosurgical manipulation.
(ii) bacterial meningitis
- Glucocorticoids are also useful to treat brain edema in cases of bacterial meningitis. Edema in these patients develops as part of the inflammatory
reaction triggered by the lysis of bacterial cell walls induced by antibiotics. The timing of glucocorticoid use may be critical as the maximal reduction
in the production of these inflammatory cytokines occurs only if therapy is started prior to the release of the bacterial cell wall components.
- Glucocorticoid use decreases morbidity and mortality in paediatric and adult acute bacterial meningitis
- In adults the usual dose is 10mg iv Q6hrly for 4 days commencing prior to administration of antibiotics
- there is lingering concern about the appropriateness of this approach in populations with a high incidence of penicillin- resistant
pneumococcus or susceptible to infection by Staphylococcus aureus (eg, neurosurgical patients) since dexamethasone use could
reduce the already limited permeability of the blood-brain barrier to vancomycin.
(iii) head injury
- In patients with severe head injury, the use of glucocorticoids is not recommended for improving outcome or reducing ICP. Several prospective
randomized trials have evaluated different regimens of glucocorticoids in this population and consistently found no evidence of therapeutic benefit.
Furthermore, the recently published CRASH trial found a trend towards increased 2-week mortality rates in head-injured patients treated with large
doses of corticosteroids (methylprednisolone 2 g bolus initiated within 8 hours of the trauma and then infusion of 400 mg/h continued for 48 hours).
These negative results may be explained, at least in part, by the untoward metabolic (particularly hyperglycemia) and nutritional effects exerted by
megadoses of glucocorticoids on critically ill patients.
(iv) ischaemic stroke
- Several randomized clinical trials have consistently shown that corticosteroids have no value in the treatment of ischemic stroke.
Steroid use also failed to benefit patients with intracerebral hemorrhage. However, more recent animal studies have indicated that
steroids might decrease infarct volume and decrease cerebral edema in models of temporary (but not permanent) focal cerebral ischemia.
This raises the possibility that corticosteroids may prove useful in patients that receive intravenous or intraarterial thrombolysis
hyperventilation
- Hyperventilation is very efficacious in reducing elevated ICP. It achieves this effect by producing cerebral vasoconstriction
and hence diminishing cerebral blood volume. Small resistance vessels are very sensitive to the acidity of the cerebrospinal fluid.
- Since the blood-brain barrier is impermeable to bicarbonate and hydrogen ions but permeable to carbon dioxide, changes
in cerebrospinal fluid hydrogen ion concentration can be fostered by changes in serum pCO2.
- The reduction in CBF occurs immediately and lasts for up to 30 minutes. In the setting of intact autoregulation, each torr
change in pCO2 generates a 3% change in CBF.
- The use of chronic hyperventilation to control intracranial hypertension is generally avoided due to concerns that cerebral vasoconstriction may worsen cerebral ischemia.
The choroid plexus buffers the augmented hydrogen ion concentration approximately 3-4 hour after any acute change, but ICP levels may return to prehyperventilation
baseline long before this.
- the only randomized trial evaluating chronic hyperventilation in head trauma found a significantly worse
functional outcome at 6 months in hyperventilated patients with initial GCS motor score of 4-5.
- brief moderate hyperventilation has been shown to reduce brain tissue PO2 below ischemic levels
and to increase extracellular concentrations of markers of anaerobic metabolism (pyruvate, lactate) and excitotoxicity (glutamate).
- Still, in selected cases, brief use of moderate hyperventilation may be justified as a bridge to safer and more definitive antiedema
treatments (such as osmotherapy or hemicraniectomy). Similar concepts may be applied to the case of intracerebral hemorrhage.
barbiturates
- Barbiturates can effectively reduce ICP in patients with severe head injury. They are generally reserved for cases
refractory to other medical measures. Metabolic suppression is the desired effect and presumed mechanism of action.
- Barbiturate dosing is typically titrated to a target ICP, but there is little additional effect on ICP once a burst suppression pattern is present on bedside electroencephalography.
- Whether barbiturates improve outcome remains controversial. Benefit in survival was noted in 1 trial, but no functional improvement was found in others.
Functional recovery after treatment with barbiturates, especially in terms of cognitive function, may be limited. However, acceptable quality of life may
be achieved, particularly by younger patients
- In patients with large ischemic infarctions, barbiturates only seem to offer limited and short-lasting benefits that may
be counterbalanced by adverse effects, especially if hypotension occurs.
other
pharmacological
alternatives
(i) intravenous glycerol
- is sometimes used as an alternative osmotic agent for the treatment of brain edema. It readily reduces ICP for up to 60 minutes
without pronounced or long-lasting effects on serum osmolarity.
- Glycerol diffuses rapidly across the blood-brain barrier and accumulates in the brain shortly after its administration; this
may lead to a brief rebound elevation in ICP. The clinical significance of this phenomenon is not well defined
(ii) THAM
- THAM may be used to buffer cerebrospinal fluid acidity. It has been shown to ameliorate the deleterious
effects of prolonged hyperventilation and may be useful to control raised ICP in patients with traumatic brain injury.
- THAM has not been evaluated in recent studies and is rarely used in practice
(iii) frusemide
-frusemide is sometimes administered in combination with mannitol. This dual therapy has been tested with variable success.
- the risk of volume contraction may outweigh any potential benefit on ICP.
(iv) acetazolamide
- The role of acetazolamide, a carbonic anhydrase inhibitor that reduces production of cerebrospinal fluid, is restricted
to patients with high-altitude illness and benign intracranial hypertension.
surgical
interventions
(i) external ventricular drainage
- In patients with ICP elevation, cerebrospinal fluid drainage is a fast and highly effective treatment measure. This assertion holds true even in the absence of hydrocephalus.
- Unfortunately, external ventricular drainage carries a substantial risk of ventriculitis, even under the best care.
(ii) hemicraniectomy in acute stroke
- While it is clear that hemicraniectomy can be lifesaving in massive stroke, its beneficial impact on the long-term
functional outcome of survivors remains unproven. Older age clearly predicts very poor recovery
(iii) craniectomy in head injury
- In patients with critical, recalcitrant intracranial hypertension after head trauma who fail to respond to all other
therapeutic measures, craniectomy with duraplasty may be a valuable alternative.
- Hemicraniectomy may be preferable in patients with focal lesions, such as hemorrhagic contusions,
but holocraniectomy is necessary in patients with massive global brain edema.
- Good long-term functional outcomes have been reported in 25-56% of young patients after this surgery. The optimal timing and indications for this intervention are not well established
Hypothermia
- Sound experimental data provide a solid foundation to the clinical evaluation of hypothermia to treat acute brain ischemia and traumatic injury.
(i) acute stroke
- While observational studies in acute stroke have established that normothermia and mild hypothermia are predictive of favorable outcome, clinical studies on
therapeutic moderate hypothermia have only included small numbers of patients and different modes of induction of hypothermia. Although these studies
offered encouraging preliminary results, the safety and efficacy of this treatment modality requires validation in larger, randomized trials.
(ii) traumatic brain injury
- Hypothermia (target bladder temperature 33°C reached within 8 hours of injury and maintained for 48 hours) failed to improve
outcome in a large prospective, multicenter, randomized trial of patients with traumatic brain injury and a GCS sum score of 3-8.
paralysis
- Pharmacologic neuromuscular paralysis should be reserved for refractory cases of intracranial hypertension if they are to
be administered at all. Routine use of neuromuscular blocking agents in head trauma patients offers no advantage in ICP control.
- Administration should be monitored using the train-of-4 responses to supramaximal
electrical impulses to avoid prolonged weakness from accumulation of the drug.
- these agents also increase the risk of developing critical illness polyneuropathy, a less predictable and preventable complication.
fluid
management
- Low serum osmolality must be avoided in all patients with brain swelling since it will exacerbate cytotoxic edema. This objective can be achieved by
strictly limiting the intake of hypotonic fluids. In fact, there is clear evidence that free water should be avoided in patients with head injuries and brain edema.
- In patients with pronounced, prolonged serum hyperosmolality, the disorder must be corrected slowly to prevent rebound cellular swelling.
Fluid balance should be maintained neutral (considering insensible losses) to sustain a state of euvolemia.
- Negative fluid balance has been reported to be independently associated with adverse outcomes in patients with severe brain trauma. Avoiding
negative cumulative fluid balance is essential to limit the risk of renal failure in patients receiving mannitol.
blood
pressure
management
- The ideal blood pressure will depend on the underlying cause of the brain edema. In trauma and stroke patients, blood
pressure should be supported to maintain adequate perfusion, avoiding sudden rises and very high levels of hypertension.
- Keeping cerebral perfusion pressure above 60-70 mm Hg is generally recommended after traumatic brain injury.
- Blood pressure targets are controversial in cases of intracerebral hemorrhage, but it is probably safe to treat hypertension
in the acute phase, and this strategy may reduce the risk of early hematoma growth. After the first 24-48 hours of hematoma onset,
blood pressure should be treated to achieve near normotension since the risk of progression of edema persists for much longer.
- In patients with ischemic stroke, rapid blood pressure reductions are detrimental in the acute phase (first 24-48 hours)
since they can produce worsening of neurologic deficits from loss of perfusion in the penumbra.
- However, in patients with large hemispheric strokes, such as malignant middle cerebral artery infarctions, this risk must
be weighed against the hazards of hemorrhagic conversion and progression of edema that may be linked to severe hypertension.
- Normal blood pressure should also be the aim in patients with lesions associated predominantly
with vasogenic edema, such as tumors and inflammatory or infectious masses.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-205-320.jpg)
![management
of traumatic
brain injury
[Created by
Paul Young
11/11/07]
prehospital
care
emergency
department
care
definitive
treatment
medical
treatment
rehabilitation
- the acutely injured brain is vulnerable to damage from systemic hypotension, cerebral hypoperfusion, hypercarbia, hypoxemia & elevated ICP
- care of the TBI victim should begin with evaluating and securing a patent airway and restoring normal breathing and circulation
- early intubation is probably of benefit; however, the benefits of prehospital
intubation have yet to be demonstrated in a randomised controlled trial
- the patient should be sedated and pharmacologically paralysed before intubation
because irritation of the oropharynx causes transient hypertension & increased ICP
- supplemental oxygen should be provided before intubation
- therapeutic hyperventilation is inadvisable unless neurological deterioration is clearly evident during
evaluation and transport; aggressive hyperventilation can cause cerebral ischaemia via vasoconstriction
- rapid fluid resuscitation and restoration of normal blood pressure are critical in the prehosptial setting because hypotension
has been associated with doubling of mortality after severe traumatic brain injury
- hypovolaemia is the likely mechanism and therefore normal saline or Hartmanns should be infused as rapidly as possible
- although preclinical studies suggested hypertonic saline may be more effective for rapid volume resuscitation in head injured patients,
several clinical trials have failed to demonstrate a benefit
- all patients with a distracting injury (including head injury) should be treated as if they have a cervical spine injury
- patients should be transported to a level I or II trauma centre (ensuring the
immediate availability of neurosurgical care when the patient arrives)
- upon arrival at the trauma centre, the emergency medical personnel should report their prehospital assessment and management including
mechanism of injury, stabilising maneouvres, medications given, initial vital signs and GCS and haemodynamic stability during transport
- immediate management should proceed according to the principles of the ATLS
protocol which is designed to identify and treat immediately life threatening injuries
- the airway should be reassessed and the need to intubate the patient should beconsidered; for patients intubated in the field the proper
position of the ET tube is verified both clinically and radiologically as well as with end tidal CO2
- when the airway is secured adequate oxygenation is confirmed using percutaneous oxygen saturation and arterial blood gas analysis
- two large bore iv catheters are inserted to provide sufficient venous access for high volume
fluid resuscitation and isotonic crystalloid should be continued to replace volume loss
- life threatening injuries such as tension pneumothorax, cardiac tamponade and overt
haemorrhage should be treated as they are discovered in the process of ATLS evaluation
- a brief neurological evaluation is performed including assessment of the GCS, pupils & extent of extremity movements
- careful inspection of the head should reveal haemotympanum, periorbital or mastoid ecchymosis and CSF rhinorrhoea or otorrhoea
- oxygen saturation is continually monitored and blood pressure frequently or continuously measured during the primary examination
- a foley catheter is placed to help monitor the fluid status and an orogastric tube is inserted to decompress the stomach
- blood specimens are obtained and analysed for glucose, electrolytes, full blood count, coags, and cross match; serum toxicology
may be appropriate and women of childbearing age should undergo a pregnancy test
- a CT brain should be performed unless haemodynamic instability necessitates an emergent laparotomy or thoracotomy; in these circumstances,
diagnostic burrholes may be appropriate in theatre if the patient has lateralising neurological deficits particularly a unilateral fixed and dilated pupil
physiological
monitoring
- critical to detemining the severity of the brain injury and the appropriate treatment are CT findings
combined with a reliable post-resuscitation GCS score and assessment of pupil size and reactivity
- other determining factors include the size and location of the haematoma, the presence and
extent of an underlying contusion or brain swelling and the results of neurological examination
- neurological deterioration suggests enlargement of the haematoma and a new CT scan should be performed promptly
- haematomas less than 10mm thick that cause midline shift of less than 5mm can usually be observed especially if they do not involve the middle
cranial fossa; a haematoma that compresses the termporal lobe is particularly ominous and can rapidly can uncal herniation so that such lesions
warrant a lower threshold for evacuation
- if a clot is small enough not to require evacuation it should be monitored with frequent CT scans over the first several days after injury. Enlarging
middle fossa haematomas large enough to cause herniation do not always lead to a rise in ICP
- patients with small or deep seated contusions without mass effect can be managed non-operatively initially. Contusions should be followed serially
with CT scanning as there is a 20-30% chance of significant enlargement in the first 24-48 hours
- a temporal contusion can enlarge to the point of uncal herniation without a significant
rise in ICP; thus, the threshold for evacuation of these lesions should be lower
- unilateral frontal or temporal lobectomies are usually well tolerated, do not cause
measurable neurological deficit and provide space for the brain to swell
general:
(i) continual end tidal CO2 and frequent analyses of ABGs allow early detection of deteriorating ventilatory status
(ii) oxygen saturation should be continuously monitored with pulse oximetry
(iii) blood pressure should be invasively monitored
(iv) CVP monitoring is often required & PACs are required in rare circumstances
(iv) urine output is continuously monitoring via an indwelling catheter
icp monitoring
- continuous icp monitoring should be mandatory for all patient with severe TBI and abnormal
CT findings because intracranial hypertension develops in 53-63% of such patients. Monitoring of ICP and MAP allows
calculation of CPP which may a more important value than MAP or ICP.
- the gold standard for icp monitoring is an ventricular catheter which has a
number of potential advantages over alternative systems:
(i) ventricular pressure is considered more reflective of global ICP than subdural,extradural or subarachnoid pressure
(ii) subdural, extradural or subarachnoid catheters are more prone to occlusion
(iii) ventriculostomies can be rezeroed after insertion
(iv) ventriculostomies allow drainage of CSF to treat intracranial hypertension
- the overall complication rate of EVDs is 7.7% with infection occuring in 6.3% & haemorrhage occuring in 1.4% [some
studies indicate that infection rate increases markedly after catheters have been in situ for 5 days]
- alternatives to ventriculostomy include devices that contain a pressure sensing transduced within the tip of the catheter (eg Codmans).
Advantages are:
(i) they provide relatively accurate measurements of global ICP,
(ii) they are easier to insert than EVDs
(iii) they may cause fewer complications than EVDs
- disadvantages of these systems are that they can only be calibrated at insertion and measurement
drift may be significant over the course of a few days
(i) avoidance of hypoxaemia:
- FiO2 should be titrated maintain normal oxygen saturation
- High levels of PEEP may increase ICP; however, clinical studies have shown that
the use of PEEP of up to 15cmH20 in patients with ARDS does not increase ICP
(ii) maintenance of normocarbia
- maintaining an arterial PCO2 of approximately 35 is advised to avoid the cerebral vasoconstriction associated with aggressive hyperventilation
(iii) avoidance of hypotension and hypovolaemia
- hypotension should be aggressively treated with normovolaemia achieved by infusing
normal saline [human albumin is associated with increased morbidity and mortality in severe TBI)
- hypotension which is refractory to volume replacement should be treated with vasopressors or inotropes
- anaemia should be treated; however, the precise level at which transfusion should occur is not clear
(iv) maintenance of CPP
- some advocate use of induced hypertension to maintain a CPP above 70mmHg; however,a randomised trial of patients with TBI comparing a
group whose CPP was kept above 70mmHg to a group whose CPP was allowed to drift to 60mmHg showed no difference in outcome at six months
between the two groups and more use of vasopressors and a higher incidence of ARDs in the group whose CPP was maintained above 70mmHg
- others have found that brain tissue PO2 in patients with TBI does not fall until the CPP drops below 60mmHg
- based on the above findings the current recommendation is to maintain a CPP above 60mmHg
(v) avoidance of intracranial hypertension
- intracranial hypertension is defined as a sustained ICP greater than 20mmHg
- several clinical studies have found that persistent intracranial hypertension is associated with significantly worse morbity and mortality
- based on the association with worse outcome and the premise that intracranial hypertension can compromise cerebral
perfusion and induce ischaemia, the aggressive treatment of intracranial hypertension is almost universally endorsed
- always considere phyysiological causes of raised ICP including seizures, fever, jugular outflow obstruction and agitation
(vi) sedation:
- increasing sedation may lead to rapid control of intracranial hypertension particularly in a patient who is posturing or agitated
- the major disadvantages of sedation are that the ability to determine an accurate GCS
is lost and sedative agents often induce hypotension
(vii) venting of CSF
- in a patient with an external ventricular drain intermittent or continuous venting of CSF is useful
- intermittent venting has the advantage of allowing reliable measurement of ICP
(viii) hyperventilation
- the use of hyperventilation to lower ICP is controversial because of its association
with cerebral vasoconstriction and potential for worsening of brain ischaemia
- recent evidence suggests that even brief periods of hyperventilation may worsen secondary brain
injury by causing and increase in extracellular lactate and glutamate levels
- its only role is probably in the patient in whom other therapies have failed in whom emergent surgery is planned to control ICP
(ix) paralysis and cooling
- paralysis may help control ICP where other measures have failed; however, it is associated with
an increased risk of pneumonia and critical care myoneuropathies
- therapeutic hypothermia to 32-34 degrees has been studied in the 1st 24-48 hours after TBI. While it has not been convincingly demonstrated to
improve outcome, it does consistently reduce ICP. In patients who are cool at arrival to hospital it appears to confer benefit in subgroup analyses
(x) barbiturate coma
- barbiturates are thought to be effective through their ability to reduce cerebral metabolic rate and blood flow
- the major disadvantages with their use is the risk of hypotension and the fact they preclude clinical brain death testing
(vii) osmotherapies
I. mannitol
- intermittent boluses of mannitol (0.25-1g/kg every 3-4 hours as needed) lowers ICP & increases CBF by expanding
intravascular volume and reducing blood viscosity within a few minutes of administration; its duration of action is 3-5 hours
- continuous infusion of mannitol is less desirable than boluses because the latter is less likely to lead to extravasation of drug
into the brain causing a reverse osmotic gradient and increased oedema
- the serum osmolarity and sodium level should be monitored frequently during mannitol administration to minimise the risk of renal
failure from ATN; the drug should be discontinued if the serum sodium exceeds 160mmol/L or the osmolarity exceeds 320mosm
II. hypertonic saline
- 3% saline can be administered as an osmotherapy and titrated to serum sodium
- principle advantages of hypertonic saline in this setting are:
(i) rapid effect which peaks in 10 minutes and wanes after 1 hour
(ii) end point for therapy is serum sodium which is 145-155 and easily monitored through ABGs
(iii) there is less potential for hypovolaemia than with mannitol
(iv) there may be a better effect on CBF for a given reduction in ICP
(v) HS is inexpensive
(vi) there is theoretical benefit in modulating the inflammatory response
- principle disadvantages of hypertonic saline in this setting are:
(i) need for central access
(ii) hypokalaemia & hypercholoraemic acidosis
(iii) lack of outcome data
(iv) increase in circulating volume and risk of CCF
(v) coagulopathy - HS may affect APTT & INR as well as platelet aggregation
(vi) rapid changes in serum sodium concentrations may result in seizures and encephalopathy
(vii) some suggest that HS affects normal brain more than injured brain which theoretically worsens herniation
penetrating injuries:
- high velocity projectiles such as bullets generally cause massive destruction of brain tissue, severe brain swelling & often death
- low veolicty massiles such as knives or arrives do not cause the massive brain injury associated with bullet wounds and usually
only the tissue in the immediate path of the missile is damaged
- dural closure is important in these patients because it reduces the risk of CSF leak and infection
- prophylactic antibiotics should be administered because the missile usually carries skin and hair into the brain
(xi) avoidance of hyperthermia
- there is a log increase in neuronal death in ischaemic brain regions for every degree above 39 for at least 24 hours after brain injury;
aggressive treatment of sources of fever should be pursued and fever should be treated. Whether aggressive cooling and paralysis
to achieve normothermia is warranted is unknown
(xi) seizure prophylaxis
- contusions and subdural haematomas are well known to cause generalised seizures and anticonvulsant
prophylaxis is therefore recommended for patients with these lesions (usually phenytoin is given)
- a proscpective randomised trial has found no benefit in continuing seizure prophylaxis beyond 7 days
- seizures may not be evident in patients who are paralysed therefore seizure prophylaxis should be
continued in these patients and continuous EEG monitoring should be considered
(xii) DVT prophylaxis
- patients with TBI, particularly those or are comatose or have associated injuries such
as pelvic or long bone fractures are at high risk of thromboembolic events
- patients should received early prophylaxis including the use of sequential calf compression devices
- early use of both heparin and enoxaparin (within 2 to 3 days of injury) has been demonstrated to be
safe in clinical trials and has not been demonstrated to cause or worsen intracranial haemorrhage after TBI
(xiii) nutrition
- malnutrition is common after TBI with metabolic expenditure increasing significantly; early enteral nutrition should be instituted
- rehabilition of TBI patients should begin in the ICU within the first few days of injury with passive
range of movement exercise and mobilisation to prevent deep vein thrombosis surgical
treatment
(i) evacuation of mass lesions
- the first response to a rise in ICP should be to repeat a CT brain to exclude a
new or worsening mass lesion that might be amenable to surgical intervention
(ii) decompressive craniectomy
- evidence surrounding decompressive craniectomy is contradictory
- while one study of patients with severe TBI demonstrated that 6 month outcomes were similar among patient given large decompressive
craniectomies than among patients that did not despite lower GCS & more severe radiolgoical abnormalities in the craniectomy group another
study has found that it did not improve ICP, CPP or mortality rates
- another study suggested that for young patients decompressive temporal lobectomy, improves outcome](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-206-320.jpg)

![mechanisms
of antimicrobial
resistance
[created by
Paul Young
02/10/07]
natural
resistance
- Some organisms are naturally resistant to a particular
antimicrobial agent, usually because they do not possess
the molecular target of the drug or are impermeable to it.
acquired
resistance
- Acquired resistance occurs through mutation or the acquisition of new genetic
material carried by mobile elements such as plasmids and transposons.
- Multiple pathways allow free exchange of genetic material within and across
microbial species and even genera.
- The four major mechanisms for acquired resistance are:
(i) drug inactivation,
(ii) target modification,
(iii) reduced permeability and
(iv) drug efflux pumps.
- These mechanisms often act synergistically to produce a resistant
phenotype when a single mechanism alone would not be sufficient.
- Moreover, selective pressure may result in the ‘bundling’ together of several
resistance genes in a single package of exchangeable genetic material. This
is particularly common in highly resistant Gram-negative organisms.
drug
inactivation
target
modification
reduced
permeability
drug
efflux
pumps
Examples:
(i) beta-lactamases
- Beta-lactamases are enzymes that hydrolyse the betalactam ring.
- Penicillin contains such a ring and is therefore inactivated by
these enzymes. The first betalactamase was discovered in S. aureus
- Gram-negative organisms naturally produce a wide range
of beta-lactamases; some are chromosomally encoded and
others reside on plasmids. The first plasmid-mediated betalactamase,
TEM-1, was originally isolated in Escherichia coli in the 1960s and
within a few years had spread to many species of Enterobacteriaceae
and Pseudomonas spp. This beta-lactamase is active against all
penicillins but not against cephalosporins
(ii) extended spectum beta lactamases
- Through amino acid substitutions, the spectrum of enzymatic activity
has increased to include broad-spectrum third generation cephalosporins.
These enzymes are collectively known as the extended spectrum
beta-lactamases.
- Some of these are specific cephalosporinases with some having broader
activity, while others possess resistance to beta-lactamase inhibitors
General:
- This mechanism includes either modification of the antimicrobial
target causing reduced affinity for the drug, or replacement of the
target with an alternative pathway.
Examples
(i) MRSA and coagulase negative S. aureus is principally due to the
production of a novel low-affinity penicillin-binding protein (PBP2a)
(ii) Similarly, alterations in penicillin-binding proteins with low affinity
for beta-lactams occur in other organisms including Enterococci and
Streptococci.
(iii) One of the mechanisms of fluoroquinolone resistance is the
alteration of the A subunit of topoisomerase IV by a point
mutation in the encoding grl-A gene.
(iv) The substitution of an alternative pathway is best illustrated
by the vancomycin-resistance Enterococci, wherea new substrate
for cell wall synthesis (D-alanine D-lactate) is used and this is not
affected by vancomycin
General:
- Reduced antibiotic permeability of the bacterial cell membrane often
acts synergistically with another mechanism such as drug inactivation
to produce clinical resistance when neither alone could do so.
Examples:
(i) The relative impermeability of the outer membrane is one of the
major causes of the high levels of intrinsic drug resistance seen
in opportunistic Gram-negative pathogens like S. maltophilia and
P. aeruginosa.
(ii) Antibiotic movement across the outer membrane occurs through
porin channels that allow hydrophilic molecules to cross the lipid bilayer.
Thus, loss of the OprD porin in P. aeruginosa produces high-level
imipenem resistance and a reduced susceptibility to meropenem
General:
- Drug efflux is the energy-dependent removal of
drugs from organisms before the drug can act
Examples:
(i) substrate-specific efflux pumps like the widespread
macrolide and tetracycline efflux systems
(ii) MexABOprM system which can export a broad range of
substrates, producing cross-resistance to a number of structurally
unrelated agents. This system has been identified in P. aeruginosa,
where the MexB protein is a broadspectrum cytoplasmic pump;
the OprM protein forms a pore that provides a portal through the
outer membrane and the MexA protein physically links these
components. The system confers resistance to penicillins,
cephalosporins, fluoroquinolones, tetracycline and chloramphenicol.
(iii) Combination of the MexAB-OprM operon with loss of OprD
produces resistance to meropenem in addition to imipenem, although
it is not the only efflux mechanism responsible for carbapenem
resistance in P. aeruginosa
(iv) Multi-drug efflux mechanisms have been identified in other organisms
including Enterobacteriaceae. Mutation of a chromosomal locus termed
mar (for multiple antibiotic resistance), which regulates susceptibility to
unrelated antimicrobials, results in a combination of active efflux and
down-regulation of the OmpF porin channel](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-208-320.jpg)
![mechanisms
of traumatic
brain injury
[created by
Paul Young
10/11/07]
epidemiology
- traumatic brain injury is the leading cause for morbidity
and mortality among people aged 1 to 45 years
- motor vehicle crashes are the major cause of head injuries
among those aged 5 to 64 years old while falls are the major
cause among over 65s
- males have twice the risk of traumatic brain injury across
all age groups
skull
fracture
- results from a contact force to the head that is usually severe enough to cause
a brief loss of consciousness
- linear fractures are the most common and typically occur over the lateral
convexities of the skull (most often they are non-displaced)
- a depressed skull fracture usually results from a blunt force from an object
with a small surface area such as a hammer
- the base of the skull can be fractured by severe blunt trauma to the forehead or the
occiput.
examples of injuries associated with skull fracture:
(i) anterior skull base fractures most often involve
the cribriform plate disrupting the olfactory nerves.
(ii) Posterior skull base fractures may extend through the petrous bone
and internal auditory canal thereby damaging the acoustic and facial nerves
(iii) fractures of the squamous temporal bone are frequently accompanied by a tear in
the middle meningeal artery causing an extradural haematoma
(iv) depressed skull fractures are often accompanied by cerebral contusion
(v) dura is often disrupted with basilar skull fracture resulting in CSF leak from
the nose or ear which may allow bacteria to enter the intracranial space
subdural
haematoma
- seen in 20-25% of all comatose victims of traumatic brain injury
- develop between the surface of the brain and the inner surface of the dura and are
believed to result from the tearing of the bridging veins over the cortical surface or from
disruption of major venous sinuses or their tributaries
- typically spread over most of the cerebral convexity with the dural reflections of the falx
cerebri preventing expansion to the contralateral hemisphere
- swelling of the cerebral hemisphere is common due to damage to the underlying brain
tissue; cerebral contusions are found in 2/3rds
- classified as acute, subacute and chronic with each having a characteristic CT appearance
- acute subdural appears white, subacute lesions
are isodense and chronic lesions are hypodense
epidural
haematoma
- develop between the inner table of the skull and the dura, usually when the
middle meningeal artery or one its branches is torn by a skull fracture
- occur in 8-10% of those rendered comatose by traumatic brain injury
- the majority are located in the temporal or parietal regions but they can also occur
over the frontal and occipital lobes and rarely in the posterior fossa
- unlike subdural haematomas their spread is limited by suture lines of the skull where the dura is
very adherent
- an epidural space does not usually exist so the clot must strip the dura from the inner table of
the skull as it enlarges resulting in the classic lenticular shape
- epidural haematomas are uncommon in infants and toddlers presumably because their
skulls are more deformable and less likely to fracture and in patients older than 60 because
the dura is extremely adherent to the skull
intraparenchymal
haematomas
- a haemorrhage within the brain substance that occurs after a very severe TBI & is
usually associated with contusions of the surrounding tissue
- Duret's haemorrhage is a haemorrhage into the base of the pons or midbrain thought
to result from disruption of the perforating arteries at the time of uncal herniation. Such
brainstem haemorrhage almost always leads to death or vegetative survival
subarachnoid
haemorrhage
- traumatic subarachnoid haemorrhage does not produce a haematoma or mass effect
- it may be associated with post-traumatic vasospasm
cerebral
contusions
- contusions are heterogenous lesions comprising punctate haemorrhage, oedema &
necrosis and often associated with other intracranial lesions
- one or more contusions occur in 20-25% of patients with severe TBI
- contusions are most common in the inferior frontal cortex and the anterior temporal lobes where
the surface of the inner table of the skull is very irregular; they may result from shifting of the of
the brain over this irregular surface at the time of impact
- direct blunt force trauma to the head can produce a contusion in the tissue underlying the point of
impact (coup contusion); if the head was in motion upon collision with a rigid surface, a contusion may
occur in the brain contralateral to the point of impact
- because they evolve over time contusions may not be visible on initial CT scan
- local neuronal damage & haemorrhage lead to oedema which may increase over the next 24-48 hours
- depending on their size and location, they may cause significant mass effect resulting in midline shift,
transtentorial or subfalcine herniation
diffuse
axonal
injury
- refers to lacerations or punctate contusions at the interface between the gray and white matter; such punctate
contusions are thought to result from the disparate densities of the grey and white matter and the consequent
difference in centripetal force assoicated with a rotational vector of injury
- occurs most commonly after a high speed motor vehicle accident in which severe angular
and rotational forces are applied to the head
- present in almost 50% of patients with severe TBI and in almost a third of those who die
- a common cause of persistent vegatative state or prolonged coma
general
general:
- trauma to the head causes primary injury such as skull fracture,
cerebral contusion, and haemorrhage that is a direct consequence
of the traumatic incident
- secondary injury occurs hours or days after the injury and may be
the major determinant of the patient's ultimate neurological outcome
primary injury:
(i) contact forces
- produce focal injuries such as skull fractures,
contusions and extra- or subdural haematomas
(ii) inertial forces:
- result from the brain undergoing acceleration or deceleration and can occur
without head impact
- inertial forces can produce focal or diffuse brain injuries: pure translational
acceleration leads to focal injuries such as contrecoup contusions, intracerebral
haematomas and subdural haematomas, whereas, rotational or angular
acceleration, common with motor vehicle accidents leads to diffuse injuries
secondary injury:
- post traumatic ischaemia initiates a cascade of metabolic events that lead to the
surplus production of oxygen free radicles, excitatory amino acids, cytokines &
other inflammatory agents
- post traumatic non-ischaemic events such as increase in intracellular free calcium
via receptor gated or voltage gated ion channels induce release of oxygen free
radicals from the mitochondria
- excessive production of oxygen free radicals causes lipid peroxidation of cell
membranes, oxidation of intracellular proteins and nucleic acids and activation of
phospholipases A2 and C which hydrolyse membrane phospholipids releasing
arachidonic acid which generate free fatty acids, leukotriennes and thromboxane
B2 all of which are associated with neurodegeneration and poor outcome after
experimental traumatic brain injury
- TBI also increase intracellular potassium levels leading to an imbalance of intracellular
and extracellular potassium, disruption of the Na+/K+ ATPase cell membrane regulatory
mechanisms and subsequent cell swelling
- severe TBI also causes a substantial decrease in extracellular magnesium which impairs
normal glycolysis, cellular respiration and oxydative phosphorylation contributing to brain
injury
- the classically described lucid interval after initial period of loss of consciousness followed by
coma occurs in fewer than a third of patients with most either remaining comatose or remaining
conscious after the initial injury
- initial signs and symptoms vary greatly depending on the size and location:
(i) small contusions may cause no symptoms or only mild headache
(ii) contusions in eloquent area of the brain such as speech or motor areas
may cause focal deficits
(iii) large contusions, especially frontal ones, cause elevated ICP and coma
aetiology
of secondary
brain swelling](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-209-320.jpg)
![mesenteric
ischaemia
[created by
Paul Young
02/10/07]
definition
aetiology
symptoms
signs
investigations
treatment
- acute mesenteric ischaemia can be divided into:
(i) acute mesenteric arterial embolus (50% of cases)
(ii) acute mesenteric arterial thrombosus (25% of cases)
(iii) nonocclusive mesenteric ischaemia (20% of cases)
(iv) mesenteric venous thrombosus (<10% of cases)
acute mesenteric ischaemia is a syndrome in which inadequate blood flow through
the mesenteric circulation causes ischaemia and eventual gangrene of the bowel wall
arterial disease:
- embolic causes include mural thrombi after myocardial infarction, atrial thrombi
associated with mitral stenosis and atrial fibrillation, vegetative endocarditis, mycotic
aneurysm and thrombi formed at atherosclerotic plaques or vascular prosthetic grafts
- nonocclusive mesenteric ischaemia is caused by a severe reduction in mesenteric
perfusion with secondary arterial spasm from causes such as septic shock, hypovolaemia,
or vasopressors (eg digoxin, cocaine, vasopressin)
- rare causes include mechanical obstruction from volvulus, intussusception,
tumour compression, aortic dissection, isolated dissection of SMA in trauma
early presentation:
- tenderness is minimal to non-existent
1. bloods:
- no blood test is sufficiently sensitive or specific and results of blood tests should
not delay radiographic study if serious suspicion of mesenteric ischaemia exists
- WCC rises as disease progresses
- Hct is initially elevated from third spacing but it decreases with GI bleeding
- amylase is elevated in 50%
- metabolic acidosis occurs late in the course
- lactate is elevated late in the clinical course but
persistently normal levels makes diagnosis unlikely
2. X-rays:
- plain films warranted to exclude perf
- positive findings are late and non-specific and include thumb printing and portal vein gas
3. CT scanning:
- CT scan helps to evaluate acute mesenteric ischaemia and to exclude other diagnoses
- CT angiography has a sensitivity of 96% and a specificity of 94%
- CT scan may show pneumotosis intestinalis, portal vein gas, bowel wall or mesenteric
oedema, abnormal gas patterns, streaking of mesentery and solid organ infarction; bowel
oedema is the most common finding
4. USS has a specificity of 92-100% and a sensitivity of 70-89%
1. iv fluids & fluid balance
2. NBM
3. pain control (opioid analgesia)
4. antiemetics
5. antibiotics
NB: avoid inotropes as they will make ischaemia worse
venous disease:
- intra-abdominal infection with portal pyemia
- hypercoagulable states
- stasis from portal hypertension or mass effect of abdominal tumours
- direct trauma to mesenteric vessels from surgery
arterial occlusive disease:
- the most important finding is pain out of proportion to the physical findings; pain may be
unresponsive to narcotics
- nausea and vomiting are common (75%)
- abdominal distention and GI bleeding are primary symptoms in up to 25%
embolic acute mesenteric ischaemia:
- has the most abrupt and painful presentation of all types
- vomiting and diarrhoea are observed
- because most emboli are of cardiac origin, patients often have atrial fibrillation or a recent MI
with mural thrombus; valvular heart disease is a less frequent source
thrombotic mesenteric ischaemi:
- typically happens when an artery already partly blocked by atherosclerosis becomes occluded
- up to 50% have a history of abdominal angina (pain starting
soon after and lasting for up to 3 hours after eating)
- precipating event that initiates thrombotic mesenteric ischaemia may be a sudden drop in cardiac
output from myocardial infarction, CCF or plaque rupture. Dehydration due to illness for another reason
may also precipitate it
- bowel viability is usually better preserved due to the presence of collaterals and onset is usually less severe
non-occlusive mesenteric ischaemia:
- occurs mainly in elderly patients and often develops in the context of multiorgan failure
- mainly patients are taking digitalis
- symptoms typically develop over several days and patients may have had a prodrome of malaise and vague
abdominal discomfort. When infarction occurs they develop increased pain and vomiting
mesenteric venous thrombosis:
- symptoms may have been present for weeks
- many patients have a risk factor for hypercoagulability
late presentation:
- tenderness becomes severe and may indicate the location of infarcted bowel
- a palpable tender mass may be present
- bowel sounds range from hyperactive to absent
- peritonitis develops
- signs of septicaemia develop
AF or heart murmurs may indicate site of embolic origin
5. angiography is the gold standard test
6. MRI & MRA are highly sensitive and specific
specific therapies:
(i) angiographically infused thrombolytics
(ii) angioplasty (limited data only available)
(iii) heparin for venous thrombosis](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-210-320.jpg)
![metabolic
acidosis
[created
by Paul
Young
12/12/07]
definition
- A metabolic acidosis is an abnormal primary process or condition leading to an increase
in fixed acids in the blood. This causes the arterial plasma bicarbonate to fall to a level
lower than expected.
causes
Pathophysiological mechanism
- A decrease in plasma bicarbonate can be caused by two mechanisms:
(i) A gain of strong acid
(ii) A loss of base
- All causes of a metabolic acidosis must work by these mechanisms. The gain of strong
acid may be endogenous (eg ketoacids from lipid metabolism) or exogenous (NH4Cl
infusion). Bicarbonate loss may occur via the bowel (diarrhoea, small bowel fistulas) or
via the kidneys (carbonic anhydrase inhibitors, renal tubular acidosis).
metabolic acidosis with increased anion gap:
Methanol, metformin
Uraemia
DKA
Phenformin, paraldehyde, propylene glycol, pyroglutamic acidosis
Iron, isoniazid
Lactic acidosis
Ethanol ketoacidosis, ethylene glycol
Salicylates, starvation ketoacidosis, solvent
classified by anion gap
metabolic acidosis with normal anion gap:
Ureteroenterostomy (K+ decreased)
Small bowel fistula (K+ decreased)
Extra chloride (K+ increased)
Diarrhoea (K+ decreased)
Carbonic anhydrase (K+ decreased)
Renal tubular acidosis (K+ decreased - type 1)
Addison's disease (K+ increased)
Pancreatic fistula (K+ decreased)
maintenance
- The disorder is maintained as long as the primary cause persists.
- Additionally, in many cases the acid-base disturbance tends to increase
in severity while the problem causing it persists though this is not absolute.
effects
Respiratory Effects
(i) Hyperventilation ( Kussmaul respirations) - this is the compensatory response
(ii) Shift of oxyhaemoglobin dissociation curve (ODC) to the right
(iii) Decreased 2,3 DPG levels in red cells (shifting the ODC back to the left)
- The shift of the oxygen dissociation curve to the right due to the acidosis occurs rapidly.
After 6 hours of acidosis, the red cell levels of 2,3 DPG have declined enough to shift the
oxygen dissociation curve (ODC) back to normal.
Cardiovascular Effects
(i) Depression of myocardial contractility
(ii) Sympathetic overactivity (incl tachycardia, vasoconstriction,decreased arrhythmia
threshold)
(iii) Resistance to the effects of catecholamines
(iv) Peripheral arteriolar vasodilatation
(v) Venoconstriction of peripheral veins
(vi) Vasoconstriction of pulmonary arteries
(vii) Effects of hyperkalaemia on heart
- The cardiac stimulatory effects of sympathetic activity and release of catecholamines
usually counteract the direct myocardial depression while plasma pH remains above 7.2.
- At systemic pH values less than this, the direct depression of contractility usually predominates.
- The direct vasodilatation is offset by the indirect sympathetically mediated vasoconstriction and
cardiac stimulation during a mild acidosis. The venoconstriction shifts blood centrally and this
causes pulmonary congestion. Pulmonary artery pressure usually rises during acidosis.
Other Effects
(i) Increased bone resorption (chronic acidosis only)
(ii) Shift of K+ out of cells causing hyperkalaemia
compensation
- Compensation for a metabolic acidosis is hyperventilation to decrease the
arterial pCO2.
- The metabolic acidosis is detected by both the peripheral and central chemoreceptors
and the respiratory center is stimulated. The initial stimulation of the central
chemoreceptors is due to small increases in brain ISF [H+]. The subsequent increase in
ventilation causes a fall in arterial pCO2 which inhibits the ventilatory response.
- Maximal compensation takes 12 to 24 hours
- The chemoreceptor inhibition acts to limit and delay the full ventilatory response
until bicarbonate shifts have stabilised across the blood brain barrier. The increase
in ventilation usually starts within minutes and is usually well advanced at 2 hours
of onset but maximal compensation may take 12 to 24 hours to develop.
- The arterial pCO2 at maximal compensation has been measured in many patients with a
metabolic acidosis. A consistent relationship between bicarbonate level and pCO2 has
been found. It can be estimated from the following equation:
Expected pCO2 = 1.5 (Actual [HCO3] ) + 8 mmHg
(Units: mmols/l for [HCO3], and mmHg for pCO2).
- The limiting value of compensation is the lowest level to which the pCO2 can fall - this
is typically 8 to 10mmHg, though lower values are occasionally seen.
- If a patient with a severe metabolic acidosis requires intubation and controlled
ventilation in hospital, the acidosis can markedly worsen unless the hyperventilation is
maintained. The ventilation should be set to mimic the compensatory hyperventilation to
keep the pCO2 low.
- Carbon dioxide crosses cell membranes readily so intracellular pH falls rapidly also,
resulting in depression of myocardial contractility, arrhythmias and a rise in intracranial
pressure.
correction
General principles are as follows:
1. Accurate diagnosis of the cause of the metabolic acidosis is essential because this
allows correct treatment of the underlying disorder
2. Treat the underlying disorder as the primary therapeutic goal
3. Provide supportive treatment (eg fluids, oxygen, treatment for hyperkalaemia)
including all appropriate emergency management
4. In most cases, IV sodium bicarbonate is NOT necessary, NOT helpful, & may even be
harmful in the treatment of metabolic acidosis.
Kidney: Renal generation of new bicarbonate
- This usually occurs as a consequence of an increase in ammonium excretion.
Liver: Hepatic metabolism of acid anions to produce bicarbonate
- The normal liver has a large capacity to metabolise many organic acid anions (eg
lactate, ketoanions) with the result that bicarbonate is regenerated in the liver. In severe
ketoacidosis there is often a large loss of ketoanions due to the hyperglycaemia induced
osmotic diuresis. This leaves a shortfall of ketoanions to be used to regenerate
bicarbonate as a consequence of their metabolism in the kidney.
Exogenous Administration of sodium bicarbonate
- This is the time honoured method to 'speed up' the return of bicarbonate levels to
normal. Indeed, this may be useful in mineral acidosis (hyperchloraemic metabolic
acidosis) where there are no endogenous acid anions which can be metabolised by the
liver. However, in most other cases of metabolic acidosis this administration is either not
helpful or may be disadvantageous.
assessment
- A metabolic acidosis is often strongly suspected because of the clinical presentation of
the patient (eg diabetes, renal failure, severe diarrhoea). Three clues from a typical
hospital automated biochemical profile are:
(i) Low 'bicarbonate' (or low 'total CO2')
(ii) High chloride
(iii) High anion gap
- In addition to arterial blood gases, some other investigations useful for indicating a
metabolic acidosis and for differentiating between the various major causes are:
(i) Urine tests for glucose and ketones
(ii) Electrolytes (incl chloride, anion gap, 'bicarbonate')
(iii) Plasma glucose
(iv)Urea and creatinine
(v) Lactate
- useful additional indices in assessment of metabolic acidosis include:
(i) Anion gap
(ii) Delta ratio
(iii) Urinary anion gap
(iv) Osmolar gap](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-211-320.jpg)
![metabolic
alkalosis
[created
by Paul
Young
14/12/07]
definition
- A metabolic alkalosis is a primary acid-base disorder which causes the plasma
bicarbonate to rise to a level higher than expected. The severity of a metabolic alkalosis is
determined by the difference between the actual [HCO3] and the expected [HCO3].
causes
general:
- The kidney rapidly excretes bicarbonate if the plasma level is elevated
- This ability of the kidney to rapidly excrete bicarbonate if its level is high is in complete contrast
to its powerful ability to reabsorb all of the filtered load if plasma [HCO3] is low or normal.
- The persistence of a metabolic alkalosis requires an additional process
which acts to impair renal bicarbonate excretion.
- This means that two issues must to be considered when analysing a metabolic alkalosis:
(i) Initiation: What process is initiating the disorder?
(ii) Maintenance: What process is maintaining the disorder?
The Initiating Process
- Classification of Initiating Processes for Metabolic Alkalosis
1. Gain of alkali in the ECF
(i) from an exogenous source (eg IV NaHCO3 infusion, citrate in transfused blood)
(ii) from an endogenous source (eg metabolism of ketoanions to produce bicarbonate)
2. Loss of H+ from ECF
(i) via kidneys (eg use of diuretics)
(ii) via gut (eg vomiting, NG suction)
- Excessive intravenous administration of alkali alone will cause a metabolic alkalosis
which is only short-lived because of rapid renal excretion of bicarbonate
- Hepatic metabolism of citrate, lactate, acetate or certain other organic acid anions to
bicarbonate can cause a brief metabolic alkalosis. This may occur after a massive blood
transfusion because of the metabolism of the administered citrate. The kidneys excrete
the bicarbonate and the urine will be relatively alkaline.
Maintenance of Alkalosis
- Maintenance of the alkalosis requires a process which greatly impairs the kidney's
ability to excrete bicarbonate and prevent the return of the elevated plasma level to
normal.
- The four factors that cause maintenance of the alkalosis (by increasing bicarbonate
reabsorption in the tubules or decreasing bicarbonate filtration at the glomerulus) are:
(i) Chloride depletion
(ii) Reduced glomerular filtration rate (GFR)
(iii) Potassium depletion
(iv) ECF volume depletion
chloride
depletion
General
- The commonest causes in clinical practice are those causing chloride depletion
- Administration of chloride is necessary to correct these disorders. The two commonest
causes of chronic metabolic alkalosis accounting for 90% of cases are loss of gastric
juice and diuretic therapy.
(i) Gastric alkalosis
- most marked with vomiting due to pyloric stenosis or obstruction because the vomitus is acidic gastric
juice only. Vomiting in other conditions may involve a mixture of acid gastric loss and alkaline duodenal
contents and the acid-base situation that results is more variable. Histamine H2-blockers also decrease
gastric H+ losses despite continued vomiting or nasogastric drainage and alkalosis will not occur if the
fluid lost is not particularly acidic
- indeed loss of alkaline small intestinal contents can even result in an acidosis if gasric acid secretion is suppressed.
(ii) Diuretics
-diuretics such as frusemide and thiazides interfere with reabsorption of chloride and sodium in the renal tubules.
Urinary losses of chloride exceed those of bicarbonate. The patients on diuretics who develop an alkalosis are
those who are also volume depleted (increasing aldosterone levels) and have a low dietary chloride intake ('salt
restricted' diet). Hypokalaemia is common in these patients.
- The effect of diuretic use on urinary chloride levels depends on the relationship of the time of urine
collection to diuretic effect: it is high while the diuretic is acting, but drops to low levels afterwards.
(iii) other causes
- Villous adenomas typically excrete bicarbonate and can cause a hyperchloraemic metabolic
acidosis. Sometimes they excrete chloride predominantly and the result is then a metabolic alkalosis.
- Chloride diarrhoea is a rare congenital condition due to an intestinal transport defect,
where the chronic faecal chloride loss can (if associated with volume depletion and K+
loss as maintenance factors) result in a metabolic alkalosis.
potassium
depletion
General
- Potassium depletion occurs with situations of mineralocorticoid excess. Bicarbonate
reabsorption in both the proximal and distal tubules is increased in the presence of
potassium depletion. Potassium depletion decreases aldosterone release by the adrenal
cortex.
Primary Hyperaldosteronism
- This condition is one cause of 'saline-resistant' metabolic alkalosis. The increased
aldosterone levels lead to increased distal tubular Na+ reabsorption and increased K+ &
H+ losses. The increased H+ loss is matched by increased amounts of renal HCO3-
leaving in the renal vein. The net result is metabolic alkalosis with hypochloraemia and
hypokalaemia, often with an expanded ECF volume.
Cushing's Syndrome
- The excess corticosteroids have some mineralocorticoid effects and because of this can
produce a metabolic alkalosis. The alkalosis is most severe with the syndrome of ectopic
ACTH production.
Severe K+ depletion
- Cases have been reported of patients with metabolic alkalosis and severe hypokalaemia
([K+] < 2 mmol/l) due to severe total body potassium depletion. Investigation has not
shown increased mineralocorticoid activity. The aetiology in these patients is not
understood but correction of the alkalosis requires correction of the potassium deficit.
These patients do not respond to saline loading unless K+ replacement is sufficient to
correct the deficit. Urinary chloride losses are high (>20mmol/l).
Bartter's syndrome
- This is a syndrome of increased renin and aldosterone levels due to hyperplasia of the
juxtaglomerular apparatus. It is inherited as an autosomal recessive disorder. The
increased aldosterone levels usually result in a metabolic alkalosis. The condition is
usually found in children. Patients who present with hypokalaemic alkalosis of uncertain
cause are often suspected of having this condition but other causes which may be denied
by the patient should be considered eg surreptitious vomiting and/or use of diuretics for
weight loss or psychological problems. Rare genetic disorders such as Gitelmann's
syndrome should also be considered.
effects
of
metabolic
alkalosis
Adverse Effects of Alkalosis
(i) decreased myocardial contractility
(ii) arrhythmias
(iii) decreased cerebral blood flow
(iv) confusion
(v) mental obtundation
(vi) neuromuscular excitability
(vii) impaired peripheral oxygen unloading (due shift of oxygen dissociation curve to left).
- Hypoxaemia may occur and oxygen delivery to the tissues may be reduced.
- Factors involved in impaired arterial oxygen content are:
(i) Hypoventilation (due respiratory response to metabolic alkalosis)
(ii) Pulmonary microatelectasis (consequent to hypoventilation)
(iii) Increased ventilation-perfusion mismatch (as alkalosis inhibits hypoxic pulmonary vasoconstriction)
- Peripheral oxygen unloading may be impaired because of the alkalotic shift of the
haemoglobin oxygen dissociation curve to the left. The body's major compensatory
response to impaired tissue oxygen delivery is to increase cardiac output but this ability is
impaired if hypovolaemia and decreased myocardial contractility are present.
compensation
- The hypoventilation causes a compensatory rise in arterial pCO2 but the magnitude
of the response has generally been found to be quite variable.
- Failure of hypoventilation may be attributed
(i) Hyperventilation due to pain
(ii)Hyperventilation due to pulmonary congestion.
- Some patients with metabolic alkalosis due to diuretic use have subclinical pulmonary congestion
sufficient to stimulate intrapulmonary receptors and cause tachypnoea and give a sensation of
dyspnoea. This slight hyperventilation is sufficient to negate the rise in arterial pCO2.
(iii) Hyperventilation due to hypoxaemia.
- An associated hypoxaemia will stimulate the peripheral chemoreceptors and cause
hyperventilation if the arterial pO2 is below 50 to 55mmHg.
- The expected pCO2 due to appropriate hypoventilation in simple metabolic alkalosis can
be estimated from the following formula:
Expected pCO2 = 0.7 [HCO3] + 20 mmHg (range: +/- 5)
- While it is widely believed that the maximum value of arterial pCO2 due to
compensatory hypoventilation is 55 to 60mmHg arterial pCO2 can rise higher than this
and values up to 86mmHg have been reported in severe cases of metabolic alkalosis
treatment
1. Correct cause if possible (eg correct pyloric obstruction, cease diuretics)
2. Correct the deficiency which is impairing renal bicarbonate excretion (ie give chloride, water and K+)
- chloride administration is essential for correction of chloride depletion metabolic alkalosis
3. Expand ECF Volume with N/saline (and KCl if K+ deficiency)
- Mineralocorticoid excess causes renal potassium wasting. This can maintain a metabolic alkalosis
even in the absence of chloride depletion.
4. If the diagnosis is not obvious, spot urine chloride is useful: low levels suggest Cl- depletion and need
for replacement; high levels suggest adrenocortical excess and need for K+ replacement
5. Rarely ancillary measures such as:
- HCl infusion
- Acetazolamide (one or two doses only)
- Oral lysine hydrochloride
6. Supportive measures (eg give O2 in view of hypoventilation; appropriate monitoring and observation)
Avoid hyperventilation as this worsens the alkalaemia
urinary
chloride
measurements
Metabolic Alkalosis Classification Based on Urinary Chloride
1. Urine Cl- < 10 mmol/l
- Often associated with volume depletion (increased proximal tubular reabsorption of HCO3)
- Respond to saline infusion (replaces chloride and volume)
- Causes: previous diuretic therapy, vomiting
2. Urine Cl- > 20 mmol/l
- Often associated with volume expansion and hypokalaemia
- Resistant to therapy with saline infusion
- Cause: Excess aldosterone, severe K+ deficiency
- Other causes: diuretic therapy (current), Bartter's syndrome
- Recent diuretic use can acutely elevate the urinary chloride level but as the diuretic
effect passes the urinary chloride level will fall to low levels. So seek information on the
timing of diuretic use. (This variability in urine chloride levels has been used as an
indicator of surreptious diuretic use)
- A 'spot' urine chloride may be misleading if bladder urine contains a mixture of urine
from during and after diuretic effect.
- A high urinary chloride in association with hypokalaemia suggests mineralocorticoid excess.
- The urinary chloride/creatinine ratio may occasionally be useful as it is elevated if there
is an extra-renal cause of alkalosis.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-212-320.jpg)
![metabolic
responses
to critical
illness
[created
by Paul
Young
15/12/07]
general
mediators
the
metabolic
response
factors
affecting
the
metabolic
response
- magnitude of the response is proportional to extent of injury
- other factors impacting on the response include:
(i) ischaemia and reperfusion
(ii) nutritional status
(iii) surgical procedures
(iv) drugs
(v) genetic polymorphisms
- some components of the response are destructive
& modulation represents a potential therapeutic target
Cytokines:
- soluble, non-antibody, regulatory proteins responsible primarily
for the inflammatory response
- the following are the major cytokines involved in the response to stress
(i) TNF-alpha
- an early mediator after exposure to endotoxin
- TNF-alpha administration reproduces all features of septic shock including
hypermetabolism, fever, anorexia, hyperglycaemia, protein catabolism &
lactic acidosis
(ii) Interleukins
- IL-1 is a potent inducer of the HPA axis as well as noradrenergic neurons
- IL-6 is the main mediator of the acute phase response
- IL-8 induces neutrophil adhesion, chemotaxis and enzyme release
- IL-4 and IL-10 are anti-inflammatory cytokines
(iii) colony stimulating factors
- stimulate the proliferation of haematopoetic cells, superoxide and cytokine
production by neutrophils & macrophages
(iv) interferon gamma
- participates in acquired cell-mediated immunity
neuroendocrine mediators
- afferent neuronal impulses and cytokine release from the site of injury or
infection activate the sympathetic nervous system and the HPA axis
(i) catecholamines
- are increased
(ii) HPA axis
- activation results in gluconeogenesis, proteolysis & lipolysis
(iii) insulin and glucagon levels
- are increased but the insulin levels are
inappropriately low for the level of hyperglycaemia
(iv) growth hormone
- levels increase transiently but IGF-1 is depressed
(v) thyroid hormone
- T4 levels are usually low-normal
(vi) ADH, renin, angiotensin, aldosterone & prolactin levels increase
cellular metabolic events:
(i) HSPs
- synthesised in response to a variety of stress
- have protective roles in sepsis and ischaemia-reperfusion
(ii) leukocyte activation
- leads to oxidative burst, production of free radicals, proteases and
arachidonic acid metabolites
(iii) apoptosis
- TNF alpha, IL-10, cortisol and NO have all been implicated in this process
intermediary metabolism
(i) protein metabolism
- IL-1, TNF-alpha & other cytokine and hormonal responses lead
to extreme protein catabolism.
- glutamine, alanine and other amino acids are mobilised from skeletal muscle
& taken up by hepatocytes and gut mucosa; glutamine depletion may occur
- fraction of energy derived from glucose is reduced while that derived from
amino acid oxidation in the Krebs cycle is increased
(ii) carbohydrate metabolism
- hyperglycaemia results from glycogenolysis, accelerated gluconeogenesis and
peripheral insulin resistance
(iii) fat metabolism
- lipolysis is increased with increased turnover of triglycerides and fatty acids
- ketosis is suppressed
(iv) electrolyte & micronutrient metabolism
- salt & water retention occurs with hyponatraemia
- potassium, magnesium & phosphate loss occurs
- Zinc is redistributed to liver and bone marrow
- iron levels decrease
systemic protein system responses
(i) acute phase response
- a systemic response to injury characterised by redirection of
hepatic protein synthesis and haematological alterations
- production of protein involved in defence is increased (eg fibrinogen, CRP,
haptoglobulin, complement C3) while synthesis of serum transport & binding
molecules is reduced (albumin, transferrin)
(ii) complement cascade
- triggers production of chemoattractants (C3a, C5a), vasoactive anaphylactoids
(C4a, C5a), opsonins (C3b), stimulation of neutrophil & monocyte burst (C3b)
& neutrophil adherence to endothelium (C5a)
energy balance and oxygen delivery
- hypermetabolism increases oxygen demand and consumption; however,
aerobic glycolysis rather than anaerobic glycolysis is characteristic of the
metabolic response to stress in usual circumstances
surgical techniques
- minimally invasive surgical techniques are associated with reduced cytokine release
starvation & nutrition
- starvation alone produces adaptive hypometabolism while critical illness is
associated with prominent protein catabolism; malnourishment in combination
with critical illness is associated with increased morbidity & mortality
drugs:
- steroids are associated with critical illness myoneuropathy
- catecholamines, theophylline, calcium channel blockers and anitbiotics all
have immunomodulatory effects
genetic polymorphisms
- mediators of the metabolic response and their effector pathways are under genetic control
- genetic polymorphisms in IL-1, TNF-alpha and HSPs may be important in sepsis outcomes
pros &
cons of the
metabolic
response
advantages:
(i) increase supply of substrates to tissues involved in defense
(ii) inflammation localises the area of injury
(iii) cardiovascular changes divert blood to inflammed areas and vital organs
(iv) salt and water retention maintains overall perfusion
disadvantages:
(i) increased oxygen consumption and myocardial work
(ii) redistribution away from gut may result in bacterial translocation to the blood stream
(iii) high catecholamine levels are arrhythmogenic
(iv) systemic inflammation can result in tissue destruction
(v) hyperglygaemia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-213-320.jpg)
![micronutrients
oxidative
stress &
SIRS
Free radicals are atoms or molecules containing one or more
unpaired electrons; they are unstable and strive to restore
parity, resulting in both positive and negative biological effects
SIRS is associated with a redistribution of vitamins and trace elements
from the circulating compartment to tissues and organs, which are
involved in protein synthesis and immune cell production
The circulating concentrations of most trace elements (iron, selenium,
zinc) and of their carrier proteins decrease as do the water-soluble vitamins
causing a relative deficit in circulating antioxidants
- Free radicals cause a cascade of intracellular events resulting in the liberation
in cytoplasm of nuclear transcription factor kappa B from its inhibitory protein
I[kappa]B, which permits its translocation into the nucleus, where it binds to
DNA, enabling the initiation of the transcription process.
- NF[kappa]B controls the production of the acute phase mediators such as
tumour necrosis factor alpha, IL-2, and IL-2 receptors, which in turn activate
NF[kappa]B, amplifying the inflammatory cascade
micronutrient
status
The interpretation of the low plasma levels observed in critically ill patients
is complex, as the causes are multifactorial.:
(i) SIRS redistribution is an important cause
(ii) acute losses through biological fluids (exudates , drains, effluents
from continuous renal replacement, chylous losses, other digestive
losses),
(iii) dilution as a result of resuscitation fluids and
(iv) insufficient intakes
supplement
trials
Antioxidant research in the critically ill has focused on five micronutrients:
copper, selenium, zinc, vitamins C and E, and the vitamin B group.
- A recent meta-analysis investigated whether supplementing critically ill
patients with antioxidants (trace elements and vitamins) positively influences
survival.
- Bibliographic databases from 1980 to 2003 were searched for randomized
studies, reporting clinically important endpoints in critically ill patients, and
comparing various combinations: only 11 articles met the inclusion criteria.
- Aggregated trials suggested that overall antioxidants were associated
with a significant reduction in mortality [risk ratio (RR) 0.65, P = 0.03].
Studies using parenteral antioxidants were associated with a significant
reduction in mortality (RR 0.56, P = 0.02), whereas studies of enteral
antioxidants were not. Selenium supplementation (alone and in combination
with other antioxidants) appeared to be associated with a reduction in
mortality (RR 0.59, P = 0.09), whereas non-selenium antioxidants were not.
- The authors concluded that trace elements and vitamins that support
antioxidant function, particularly high-dose parenteral selenium either
alone or in combination with other antioxidants, are safe and might be
associated with a reduction in mortality in critically ill patients. Most of the
studies performed to date have, however, been small single-centre studies,
prompting the need for further research before definitive conclusions can be
reached.
- a study of 200 critically ill cardiac and trauma patients randomly
assigned to either 5 days of antioxidant supplements (selenium,
zinc, vitamin B1) or placebo showed a trend to shorter hospital
stay in trauma patients (-10 days, P = 0.07). The SOFA score,
which reflects the number of failing organs, decreased significantly
over time in both groups, but declined faster in the antioxidant group (P = 0.05).
- two small randomized placebo-controlled trials in patients with major
burns showed that this trace element supplementation (copper, selenium,
zinc) was associated with a reduction of nosocomial pneumonia
adverse
effects
- Trace elements and vitamins have dose response
curves, with the risk of toxicity at high levels of intake.
- Most toxicity data relate to chronic intakes of food ingested over many months or years
- Zinc toxicity, in the form of a negative impact on immunity and
progressive cholestasis, has been reported over 50 mg per day
- Copper toxicity is reflected primarily by liver damage
- Selenium toxicity data in humans are based on both single observations
and epidemiological data: an upper limit of intake of selenium in the diet
has been set at 400 g (5 g/kg) per day; an upper limit for safe short-term
intravenous supplementation of 750-1000 g selenite per day has been suggested
- The results of a meta-analysis of 19 randomized, placebo-controlled trials
in the community suggest that long-term high dosages of vitamin E increase
the risk of all-cause mortality; relevance to short-term dosage in critically ill is not clear](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-214-320.jpg)


![motor
neuron
disease
[created
by Paul
Young
14/11/07]
general
- Amyotrophic lateral sclerosis (aka motor neuron disease) is a devastating
illness with uncertain pathogenesis.
- Amyotrophic lateral sclerosis is a progressive disorder that involves
degeneration of the motor system at all levels.
clinical
features
- The clinical features of amyotrophic lateral sclerosis are indicative of the
loss of neurons at all levels of the motor system-from the cortex to the
anterior horn of the spinal cord. Physical signs of this disorder thus
encompass both upper motor neuron and lower motor neuron findings.
- Objective sensory findings are incompatible with a diagnosis of amyotrophic lateral
sclerosis unless they can be accounted for by neurological comorbidity.
- The clinical features can be considered in relation to neurological regions or levels:
bulbar, cervical, and lumbar.
Bulbar-onset ALS
- Bulbar-onset patients present with slurring of speech (dysarthria), difficulty
swallowing (dysphagia), or both.
- Exclusion of other potentially treatable diseases is important-eg, oesophageal
carcinoma and myasthenia gravis. Bulbar involvement can be lower motor neuron
(bulbar palsy), upper motor neuron (pseudobulbar palsy), or both.
- Bulbar palsy is associated with upper and lower facial weakness and poverty
of palatal movement with wasting, weakness, and fasciculation of the tongue.
- Pseudobulbar palsy is characterised by emotional lability (also known as
pathological laughing or crying), brisk jaw jerk, and dysarthria.
Cervical-onset ALS
- Cervical-onset amyotrophic lateral sclerosis presents with upper-limb symptoms,
either bilateral or unilateral. Proximal weakness can present as difficulty with tasks
associated with shoulder abduction (eg, hair washing,combing, etc), and distal
weakness can manifest with impairment of activities requiring pincer grip.
- Upper limb signs might also be upper motor neuron, lower motor neuron, or both.
The arm can be strikingly wasted with profuse fasciculation and brisk reflexes.
Lumbar onset ALS
- Lumbar onset implies degeneration of the anterior-horn cells of the lumbar
enlargement and is associated with lower motor neuron symptoms and signs in
the legs, such as a tendency to trip (foot drop) or difficulty on stairs (proximal
weakness).
therapy
prognosis
-The course of the disorder is inexorably progressive, with 50% of patients dying
within 3 years of onset.
epidemiology
- The incidence of sporadic ALS is between 1.5 and 2.0 per 100 000
population per year, giving a prevalence of around 6 per 100 000.
- Males are usually affected more than females (ratio about 1.6:1).
related
conditions
Progressive muscle atropy
- Progressive muscular atrophy is a lower motor neuron syndrome without
upper motor neuron signs. The relation between progressive muscular
atrophy and amyotrophic lateral sclerosis has been debated extensively.
- Some patients with progressive muscular atrophy progress fairly slowly, prompting
the suggestion that the disorder is a variant of spinal muscular atrophy, a much less
aggressive motor neuron disease. Other affected individuals presenting with progressive
muscular atrophy eventually develop full amyotrophic lateral sclerosis.
Primary lateral sclerosis
- Primary lateral sclerosis is a pure upper motor neuron disease without lower motor
neuron involvement. This entity has also been debated widely. In a review of 39 patients
with primary lateral sclerosis, 16 remained free of lower motor neuron signs throughout
their clinical course but 13 eventually presented with evidence of lower motor neuron
involvement, suggesting that a substantial proportion of these individuals develop
amyotrophic lateral sclerosis before death.
Bulbospinal muscular atrophy
- Although technically a variant of spinal muscular atrophy, bulbospinal muscular
atrophy (Kennedy's syndrome)-an X-linked recessive lower motor neuron syndrome
with bulbar involvement-can be confused with amyotrophic lateral sclerosis. Tongue
wasting and fasciculation, gynaecomastia, testicular atrophy, and infertility are
characteristic findings.
Multifocal motor neuropathy
- Multifocal motor neuropathy is an important differential diagnosis because it is
potentially treatable. Weakness generally affects distal arm muscles and can be in
the distribution of individual nerves. Cranial nerves and respiratory muscles are
rarely affected.
- Upper motor neuron signs are absent and the disease can be very slowly progressive,
over a period of up to 30 years.
Disease-modifying treatments
- Many putative disease-modifying strategies for amyotrophic lateral sclerosis have been
tested in clinical trials but only one drug (riluzole) has so far been licensed. It prolongs the
lifespan of patients with amyotrophic lateral sclerosis by an average of 3 months.
symptomatic treatments
key elements include management of nocturnal hypoventilation, dysphagia, dysarthria,
dyspnoea, psychosocial and palliative care; tracheostomy in the terminal phase is likely
to lead to an essentially 'locked-in' state](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-217-320.jpg)

![Myaesthenia
Gravis [created
by Paul Young
29/11/07]
general
clinical
features
drugs that
may increase
weakness in
myaesthenia
- myaesthenia gravis is a consequence of autoimmune attack on the
acetylcholine receptor complex at the postsynaptic membrane of the
neuromuscular junction
aetiology
- occurs at a rate in early adulthood in women but later in life the
rates for men and women become nearly equal
- reported prevalence is 14.2 cases per 100,000 population
- results in weakness with a fluctuating pattern that is most marked after
prolonged exertion
- typically involves ocular muscles producing ptosis and diplopia as well as
bulbar muscle weakness resulting in dysphagia and dysarthria
- the diagnosis should be considered in patients who have acute respiratory
failure with these cranial nerve findings
investigations
- a clinical diagnosis of myaesthenia gravis may be supported by:
(i) edrophonium testing (tensilon test)
(ii) electrophysiological studies including repetitive
nerve stimulation studies and single fibre EMG
(iii) ACh receptor and muscle specific receptor tyrosine kinase antibody testing
- approximately 20% of patients develop myaesthenia crisis
with respiratory failure requiring mechanical ventilation
- the most common precipitating factors for myaesthenic crisis include:
(i) bronchopulmonary infections (29%)
(ii) aspiration (10%)
- other precipitating factors include:
(i) sepsis
(ii) surgical procedures
(iii) rapid tapering of immunomodulatory therapy
(iv) beginning treatment with corticosteroids
(v) pregnancy
(vi) exposure to certain drugs
- thymomas are associated with more fulminant disease and are identified in
about 1/3rd of patients in myaesthenic crisis
- intensivists may also encounter myaesthenic patients for management of
complications of immunomodulatory treatment or for postoperative care after
thymectomy
(i) neuromuscular blocking agents
(ii) selected antibiotics:
- aminoglycosides (especially gentamycin)
- macrolides
(iii) selected cardiovascular agents
- beta blockers
- calcium channel blockers
- procainamide
- quinidine
(iv) quinine
(v) corticosteroids
(vi) magnesium
(vii) iodinated contrast agents
(viii) d-penicillamine
(ix) morphine & pethidine
- upper airway muscle weakness is a common mechanism leading to myaesthenic
crisis due to oropharyngeal and laryngeal weakness resulting in upper airway
collapse with obstruction along with inability to swallow secretions leading to
obstruction or aspiration
- findings of bulbar myaesthenia associated with upper airway compromise include:
(i) flaccid dysarthria with hypernasal, staccato or hoarse speech
(ii) dysphagia sometimes associated with nasal regurgitation
(iii) chewing fatigue
- jaw closure is often weak and cannot be maintained against resistance
- patients with myaesthenic tongue weakness may be unable to protrude the tongue
into either cheek
treatment
- patients with features of impending myaesthenic crisis including severe bulbar
weakness, vital capacity of less than 20-25ml/kg, weak cough with difficulty
clearing secretions should be admitted to an intensive care unit
- respiratory function tests are often performed; however, these measurements are
often inaccurate due to difficulty sealing lips around the spirometer. They may also
fail to predict respiratory failure due to the fluctuating nature of the disease
- criteria for intubation are similar to other neuromuscular conditions:
(i) failure to protect airway
(ii) fatigue
(iii) hypercapnic respiratory failure (the majority who become hypercapnic require intubation)
plasma exchange:
- an effective short term treatment for myaesthenia gravis and for surgical
preparation in symptomatic myaesthenic patients with significant improvements
having been demonstrated in several case series (no controlled trials have been
performed)
- onset of improved strength is generally seen after 2 or 3 exchanges
IVIg
- may represent an alternative short term treatment for myaesthenia candidates who are
poor candidates for plasma exchange sue to difficult vascular access or septicaemia
- comparable efficacy with plasma exchange has been demonstrated in a small
randomised controlled trial of IVIG at 1.2 and 2g/kg over 2-5 days; however, a
larger retrospective study suggested plasma exchange was more effective
Corticosteroids:
- eg prednisilone 1mg/kg/day are occasionally used in prolonged myaesthenic
crises that fail to respond to to treatment with plasma exchange or IVIG
- initiation of corticosteroids may lead to a transient increase in weakness
cholinergic
crisis
- in the context of myaesthenic crisis, excessive dosing of cholinesterase inhibitors
may superimpose a cholinergic crisis owing to depolarisation blockade and result in
increased weakness (worsening with a tensilon test indicates that the patient is
likely to be suffering from over administration of anticholinergics)
- other symptoms of cholinergic crisis include muscle fasiculations and prominent
muscarinic symptoms including miosis, lacrimation, sweating, salivation, abdominal
cramps, diarrhoea, vomiting, increased bronchial secretions and bradycardia
- relatively rare event because it is now common practice to avoid repeated dose
escalation of cholinesterase inhibitors in myaesthenic crisis and to discontinue their
use after intubation to reduce muscarinic complications
Thymectomy:
- may result in long-term improvement in patients with a suspected thymoma
or with a life expectancy of greater than 10 years
Acetylcholinesterase inhibitors:
- pyridostigmine
- rivastigmine](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-219-320.jpg)
![myocarditis
[created by
Paul Young
15/10/07]
general
- inflammation of the heart muscle
aetiology
- Coxsackie virus B (an enterovirus) is the most common cause of viral myocarditis
- HIV is generally associated with another infection rather than being causative itself
- Rhematic fever is an important post-infectious cause
- Systemic diseases such as SLE, polymyositis, scleroderma & sarcoidosis can be complicated by myocarditis
- Infiltrative cardiomyopathies such as haemochromatosis or amyloidosis may have myocarditis as a feature
(i) active viral
(ii) post viral (lymphocytic)
(iii) hypersensitivity
(iv) autoimmune
(v) infectious
(vi) giant cell myocarditis
clinical
presentation
- most often presentation is with chest pain, fatigue, dyspnoea & palpitations
- frequently there is prodrome of fever, malaise & arthralgias
- examination can show fever, tachycardia, S3 & S4,
pericardial rub & signs of biventricular failure
investigations
- blood tests may reveal leukocytosis, eosinophilia & an elevated ESR;
cardiac biomarkers may be elevated & rheumatological serological
markers and HIV testing should be undertaken
- ECG shows sinus tachycardia and nonspecific
ST elevation & T wave changes most often
- there may be arrhythmias or conduction block
- echocardiography is essential
- myocardial biopsy is the most definitive diagnostic technique with
histopathological diagnosis made on the basis of the Dallas criteria
- biopsy should be strongly considered when results will affect management
clinical
course
- patients with heart failure & myocarditis can recover normal LV function;
however, a number progress to chronic cardiomyopathy
- rarely patients present with a fulminant course with severe acute
heart failure, pulmonary oedema & cardiogenic shock
- paradoxically, patients will fulminant myocarditis have the best
long-term prognosis with >90% 1 year and 10 year survival rates
therapy
general heart failure therapies:
- there are no controlled trials in humans that have evaluated standard heart failure
medications in patients with myocarditis; however, use of ACE inhibitors in particular
is supported by animal models & beta blockers & aldosterone antagonists are also used
intensive care therapies:
- inotropes and vasopressors may be required
- in patients with fulminant myocarditis, mechanical ventricular assist devices
& IABP should be considered because of the potential for spontaneous resolution
& good outcome
- cardiac transplant is the final option for treating critically ill patients with myocarditis;
however, it should only be used as a last resort
immunosuppressive therapies:
- clinical trials do not support the routine use of immunosuppressive in patients
with lymphocytic myocarditis; however, this treatment should be considered in
patients positive biopsy findings who continue to deteriorate despite routine care
& in patients with severe heart failure
- immunosuppressive therapy should be used in patients with myocarditis associated
with rheumatological diseases
- commonest feature on myocardial biopsy is infiltration of the myocardium with lymphocytes
& fibroblasts accompanied by myocyte necrosis (associated with lymphocytic myocarditis)](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-220-320.jpg)
![myxoedema
coma features
& diagnosis
[created by
Paul Young
02/12/07]
general
- Myxedema coma represents the most extreme form of hypothyroidism, so
severe as to readily progress to death unless diagnosed promptly and treated
vigorously.
- Like uncomplicated hypothyroidism, the diagnosis rests on a determination of serum thyroid-
stimulating hormone (TSH). Most hospital and commercial laboratories can turn around
aTSH result within hours, and once the diagnosis is made, therapy should be initiated
immediately. Nevertheless, even with reasonably early diagnosis and customary
therapy, the mortality rate approaches 50% to 60%.
epidemiology
- Because hypothyroidism is some eightfold more common in women than in
men, most patients who might present with myxedema coma are women.
- Because hypothyroidism is most common in the later decades of life, most of these
women are elderly.
general
features
precipitating
factors
- Whatever the precipitating cause, the course is typically one of lethargy progressing to stupor
and then coma, with respiratory failure and hypothermia, all of which may be hastened by the
administration of drugs that depress respiration and other brain functions.
- The characteristic features of severe hypothyroidism are present, such as dry skin, sparse hair,
a hoarse voice, periorbital edema and nonpitting edema of the hands and feet, macroglossia, and
delayed deep tendon reflexes, and moderate to profound hypothermia is common.
- In addition to hyponatremia and hypoglycemia, a routine laboratory evaluation may indicate
anemia, hypercholesterolemia, and high serum lactate dehydrogenase and creatine kinase
concentrations
diagnosis
- The probable diagnosis of myxedema coma should readily come to mind, given a patient with a
history of or physical findings compatible with hypothyroidism in the presence of stupor,
confusion, or coma, especially in the setting of hypothermia.
- Given a reasonable index of suspicion, therapy with thyroid hormone should be begun
immediately, while awaiting the results of measurements of serum thyrotropin (TSH) and
thyroxine(T4). In elderly patients, however, especially those with underlying cardiac
disease, thyroid hormone therapy should be undertaken more cautiously because of the risks.
-thyroid hormones can be measured in several hours on a routine basis or, if necessary, should
be so requested on an emergency basis. Although markedly elevated serum TSH would be
expected, patients with severe nonthyroidal systemic illness may demonstrate a phenomenon
parallel to the ''euthyroid sick'' syndrome, which can be called the ''hypothyroid sick'' syndrome.
In such circumstances, pituitary TSH secretion is reduced and the blood levels may not be as
high as one might otherwise expect.
- approximately 5% of cases of myxedema coma are diagnosed on the basis of central
hypothyroidism and could have normal or low serum TSH concentrations.
- Irrespective of whether the disease is primary or secondary thyroid failure, all patients with
myxedema coma have low serum total and free T4 and triiodothyronine (T3) concentrations.
neuro-
psychiatric
features
cardiac
features
infections
Neuropsychiatric manifestations
- In patients with myxedema coma, there may be a history of lethargy, slowed mentation, poor
memory, cognitive dysfunction, depression, or even psychosis, as can also be seen in patients
with uncomplicated hypothyroidism. They do not complain of these symptoms, however, because
of their impaired state of consciousness.
- Focal or generalized seizures may be seen in up to 25% of patients, possibly related to
hyponatremia, hypoglycemia, or hypoxemia because of reduced cerebral blood flow.
Cardiovascular manifestations
- Typical cardiovascular findings in myxedema coma as well as in hypothyroid heart disease
include nonspecific electrocardiographic abnormalities, cardiomegaly, bradycardia, and reduced
cardiac contractility.
- Low stroke volume and cardiac output occur as a result of the reduction in cardiac contractility,
but frank congestive heart failure is rare. Cardiac enlargement may be real and attributable to
ventricular dilatation or could represent a pericardial effusion.
- Hypotension may be present because of decreased intravascular volume and cardiovascular
collapse, and shock may occur late in the course of the disease. In shock, the hypotension may
be refractory to vasopressor therapy unless thyroid hormone is also being given.
Infections
- Because hypothermia is the rule in myxedema coma, the presence of a ''normal'' temperature
should be a clue to underlying infection. Other signs of infection, such as diaphoresis and
tachycardia, are also absent. Patients who fail to survive often have been shown to have had
unrecognized infection and sepsis.
- The possibility of an underlying infection should always be considered while maintaining a low
threshold for initiation of systemic antibiotic coverage. The presence of pneumonia also worsens
or even causes hypoventilation, and there is a heightened risk of pneumonitis attributable to
aspiration caused by neurogenic dysphagia, semicoma, or seizures.
gastro-
intestinal
features
Gastrointestinal manifestations
- Patients with myxedema coma may have anorexia, nausea, abdominal pain, and constipation
with fecal retention. A distended quiet abdomen may be present, reduced intestinal motility is
common, and paralytic ileus and megacolon may occur.
- A type of neurogenic oropharyngeal dysphagia has been described that is associated with
delayed swallowing, aspiration, and risk of aspiration pneumonia.
- Gastric atony, if present, may serve to reduce absorption of oral medications.
respiratory
features
Respiratory system
- The reduced hypoxic respiratory drive and decreased ventilatory response to hypercapnia
known to occur in hypothyroidism are likely responsible for the respiratory depression commonly
seen in myxedema coma, but impaired respiratory muscle function and obesity may exacerbate
the hypoventilation
- The respiratory depression leads to alveolar hypoventilation and progressive hypoxemia and,
ultimately, to carbon dioxide narcosis and coma. Although there are many contributing causes to
the coma in these patients, the principal factor seems to be a depressed respiratory center
response to carbon dioxide.
- Mechanically assisted ventilation is required in most patients, irrespective of the cause of the
respiratory depression and hypoventilation. Respiration may be impaired in these patients as
well by the presence of pleural effusions or ascites, by reduced lung volume, and by macroglossia
and edema (myxedema) of the nasopharynx and larynx, which serve to reduce the
effective airway opening.
- Even after initiation of thyroid hormone therapy, assisted ventilation may have to be continued
because of delayed recovery
renal
&
electrolytes
Renal and electrolyte manifestations
- Patients may have bladder atony with urinary retention. Hyponatremia in any patient may cause
lethargy and confusion, and hyponatremia and a reduced glomerular filtration rate are consistent
findings in patients with myxedema coma.
- The hyponatremia results from an inability to excrete a water load, which is caused by
decreased delivery of water to the distal nephron and excess vasopressin secretion. Urinary
sodium excretion is normal or increased, and urinary osmolality is high relative to plasma osmolality.
hypothermia
Hypothermia
- As noted previously, hypothermia is present in virtually all patients and may be quite profound.
In many of the reported cases, hypothermia was the first clinical clue to the diagnosis of myxedema
coma.
- The ultimate response to therapy and survival has been shown to correlate with the degree of
hypothermia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-221-320.jpg)
![myxoedema
coma
treatment
[created
by Paul
Young
03/12/07]
general
ventilatory
support
hypothermia
hypotension
glucocorticoid
therapy
thyroid
hormone
therapy
- Because of the potentially high mortality without vigorous multifaceted therapy, all patients
should be admitted to an intensive care unit to permit continuous close monitoring of their
pulmonary and cardiac status.
- Thorough attention to an evaluation of respiratory function should include assessment of
pulmonary function (blood gas measurements) and physical examination and imaging to rule out
pneumonia or airway obstruction attributable to macroglossia or myxedema of the larynx.
- Insertion of an endotracheal tube or performance of a tracheostomy may be required to
achieve adequate oxygenation.
- Mechanical ventilatory support is required typically for 24 to 48 hours, especially in patients
whose hypoventilation and coma result from drug-induced respiratory depression, and some
patients may require it for several weeks
- External warming of patients with hypothermia with an electric blanket is advisable but should
be done cautiously because of the risk of hypotension caused by vasodilatation with a fall in
peripheral vascular resistance.
- Therapy with thyroid hormone is absolutely essential for ultimate restoration of normal body
temperature, but the amelioration of hypothermia by thyroid hormone may take several days.
- Because external warming may worsen hypotension, it should be preceded and accompanied
by careful intravenous volume repletion
- Some patients require vasopressors to maintain their blood pressure until thyroid hormone
action begins.
- Because of its nonspecific presumed effects on vascular stabilization, hydrocortisone (100 mg
administered intravenously every 8 hours) is usually administered and is definitely warranted if
pituitary disease or concomitant primary adrenal insufficiency is suspected.
- As mentioned previously, steroid therapy is indicated in those patients with myxedema coma
attributable to pituitary or hypothalamic disease because they may have corticotropin deficiency
as well as TSH deficiency.
- Primary adrenal insufficiency could be present in patients with primary hypothyroidism caused
by Hashimoto disease on an autoimmune basis (Schmidt syndrome).
- There may be other clinical and laboratory clues to the coexistence of adrenal insufficiency in
patients with myxedema coma, such as hypotension, hypoglycemia, hyponatremia, hyperkalemia,
hypercalcemia, lymphocytosis, and azotemia
- In most patients with myxedema coma, the serum cortisol concentrations are within the
reference range.
- It is generally deemed prudent to treat with hydrocortisone because of the possibility of
coexistent primary or secondary adrenal insufficiency but also because of the possibility that
thyroid hormone therapy may increase cortisol clearance and precipitate adrenal insufficiency
- Hydrocortisone usually is given intravenously (50-100 mg every 6 to 8 hours for several days),
after which it is tapered and discontinued on the basis of clinical response and plans for further
diagnostic evaluation. Such short-term glucocorticoid therapy is safe and can be discontinued
when the patient has improved and pituitary-adrenal function has been assessed to be adequate.
- Patients with myxedema coma need thyroid hormone and die without it. Nevertheless, although
the need to treat these patients with thyroid hormone is so patently obvious, the regimen by which
to conduct this treatment remains somewhat controversial.
- The question is how to restore the low serum and tissue thyroid hormone concentrations to
normal safely, and the controversy, simply put, relates to whether to administer T4 or T3.
- Whether one is administering T4 or T3, additional concerns relate to the dosage, frequency, and
route of administration. We need to choose an approach to thyroid hormone therapy that
balances concern for the high mortality of untreated myxedema coma against the risks of high-
dose thyroid hormone therapy, which may include atrial tachyarrhythmias or myocardial infarction.
- No one really knows what constitutes the optimal therapeutic approach and recommendations
tend to be empiric at best.
- One argument for using T4 is that serum levels are easier to measure than are those for serum
T3, but this is really not the case any longer in modern laboratories. Serum T4 measurements
may be easier to interpret, however, because the values do not vary as much between doses as
would serum T3 values. T4 therapy may also provide a steadier and smoother, albeit slower,
onset of action with a lower risk of adverse effects.
- Conversely, the onset of action of T3 is quicker, and its serum (and probably tissue)
concentrations fluctuate more between doses.
- In either case, monitoring serum TSH values can provide the information necessary to adjust
dosage to achieve the desired impact of treatment at the tissue level.
- Parenteral T4 preparations are available in vials containing 100 and 500 mcg. A high single
intravenous bolus dose (usually 300-600 mcg) has been used for decades, based on a report
suggesting that replacement of the entire extrathyroidal pool of T4 was desirable to restore near-
normal hormonal status as rapidly as possible.
- An average estimate of total body T4 is 500 mcg hence, that initial dose. Thereafter, the body T4
pool is maintained by administration of 50 to 100 mcg daily given intravenously or orally. With the
large initial dosage, serum T4 concentrations rapidly rise to supranormal values and then fall to
within the normal reference range in 24 hours. In sequence, as T4 is converted to T3, the serum
T3 concentrations begin to rise and serum TSH concentrations start falling.
- T3 is available for intravenous administration in vials containing 10 mcg. When given alone, the
usual dose is 10 to 20 mcg, followed by 10 mcg every 4 hours for the first 24 hours and then 10 mcg
every 6 hours for 1 or 2 days; by that time, the patient should be alert enough to continue therapy
by the oral route.
- Measurable increases in body temperature and oxygen consumption occur within 2 to 3 hours
after intravenous administration of T3 but may take 8 to 14 hours or longer after intravenous
administration of T4. These changes after T3 therapy are likely to be accompanied by significant
clinical improvement within 24 hours but at a greater risk of adverse cardiovascular side effects.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-222-320.jpg)
![necrotising
fasciitis &
other rapidly
progressive
skin & soft
tissue infections
[created by
Paul Young;
03/10/07]
causative
organisms
risk
factors
- Underlying comorbidities that may predispose to necrotizing fasciitis include
diabetes mellitus, alcohol abuse, peripheral vascular disease, renal failure,
odontogenic infection, and malignancy; it may complicate chicken pox.
- Group A streptococcal necrotizing fasciitis, however, often occurs in young,
previously healthy patients. This is postulated to be due to the absence of
previous exposure to these more virulent strains of bacteria, as an absence of
protective antibody appears to predispose persons to infection
- Penetrating and crush injuries are particularly likely to cause these infections
(chicken pox) in children and adults.
prognosis
- Mortality rates range from 20% to 40%.
- Higher mortality rates are found in people with diabetes, malnutrition,
obesity, arteriosclerosis, and advancing age.
- In addition, delay in diagnosis and treatment and infections with
invasive group A streptococcus are associated with higher mortality
rates.
clinical
features
- Necrotizing fasciitis often begins with pain deceptively
out of proportion to any skin findings.
- The clinical presentation changes to an exquisitely tender,
swollen area of extensive soft tissue erythema
- The disease progresses at an alarming rate, with skin changing
from a shiny red-purple to a pathognomonic gray-blue with ill-
defined patches often within 36 hours after onset.
- Necrosis of the superficial fascia and fat produces a thin,
watery, malodorous fluid. The area may later become
anesthetic as cutaneous nerves are destroyed. A hard,
wooden feel of the subcutaneous tissues may be present.
- Crepitance has been noted in approximately 30% and is
associated with polymicrobial infections, including Enterobacteriaceae
and Clostridium.
- Patients can become extremely toxic, with high fever, anxiety, altered
mental status, leukocytosis, shock, and tachycardia.
- The most common primary site is an extremity, although necrotizing
fasciitis can affect any body part.
- When present in the perineum and genitalia, it is known as Fournier's
gangrene, which is due to infection with group A streptococci or mixed
infection with enteric bacilli and anaerobes.
- This entity originates from the scrotum and rapidly progresses
to the perineum and anterior abdominal wall. The testes are spared from
necrosis because of their separate blood supply. Urethral obstruction can
occur from excessive penile edema.
pathology
- The histological hallmark is extensive inflammation and
necrosis of the subcutaneous fat, fascia, and muscle.
therapy
- Extensive surgical debridement (fasciotomy) is the mainstay of effective treatment.
- Antimicrobial therapy is directed toward the results of the initial
Gram's staining and culturing of aspirate. Initial broad-spectrum
therapy with a b-lactam/ b lactamase inhibitor and clindamycin
- There is evidence to suggest that clindamycin, a protein synthesis inhibitor,
suppresses toxin production by streptococci, making it a necessary component
of initial antibiotic therapy, until cultures andsensitivities are available.
- In nosocomial infections where MRSA is prevalent or in cases
with serious penicillin allergy, empiric therapy with vancomycin
and clindamycin would be considered.
- Hyperbaric oxygen therapy remains controversial; however, if available, it
may be a beneficial adjunct for a subset of patients with anaerobic
gram-negative necrotizing fasciitis.
- Intravenous immunoglobulin (IvIG) has been useful in uncontrolled reports
for patients with severe group A streptococcal necrotizing fasciitis.
infective
causes of
soft tissue
crepitus
- These infections can be caused by:
1. monomicrobial pathogens including:
(i) streptococci especially Streptococcus pyogenes (approximately 10%
are caused by group A streptococcus alone)
(ii) Clostridium perfringens (gas gangrene) and other clostridial species,
(iii) Staphylococcus aureus,
(iv) Vibrio vulnificus and other Vibrio species,
(v) Aeromonas hydrophila
2. polymicrobial synergistic gangrene involves:
(i) mixed aerobe-anaerobe bacterial flora (eg Escherichia coli, Bacteroides fragilis,
streptococci and staphylococci).
Empirical therapy
- For empirical therapy, where the diagnosis is uncertain and until tissue and
blood culture results are available, use initially:
meropenem 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly
PLUS EITHER
clindamycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly
OR
lincomycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly.
- Penicillin is commonly added but is theoretically unnecessary.
- Consider the use of immunoglobulin if Streptococcus pyogenes necrotising
fasciitis is suspected.
Streptococcus pyogenes necrotising fasciitis
- For Streptococcus pyogenes necrotising fasciitis, in addition to surgical
debridement, use:
benzylpenicillin 1.8 g (child: 45 mg/kg up to 1.8 g) IV, 4-hourly
PLUS EITHER
clindamycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly
OR
lincomycin 600 mg (child: 15 mg/kg up to 600 mg) IV, 8-hourly
PLUS (consider after expert advice)
immunoglobulin 0.4 to 2 g/kg IV, for 1 or 2 doses during the first 72 hours.
- For patients hypersensitive to penicillin (excluding immediate hypersensitivity),
substitute for benzylpenicillin:
cephalothin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly
OR
cephazolin 2 g (child: 50 mg/kg up to 2 g) IV, 8-hourly.
Polymicrobial necrotising fasciitis and synergistic gangrene
- Synergistic gangrene is so-called because it is polymicrobial and the organisms
are thought to act synergistically. The term Fournier’s gangrene is used for
synergistic gangrene of the genitalia, usually following spread from a perianal,
retroperitoneal or urinary tract infection, or following genital trauma (eg postpartum).
- For synergistic gangrene and for polymicrobial necrotising fasciitis, in addition to
surgical debridement, use:
meropenem 1 g (child: 25 mg/kg up to 1 g) IV, 8-hourly.
- Modify therapy according to culture and susceptibility results.
Clostridial infection
- Clostridial infection varies from mild cellulitis to overwhelming myonecrosis
(gas gangrene). The basis of treatment is surgical debridement of necrotic
tissue, resuscitation and antibiotic therapy.
- In severe infections, hyperbaric oxygen should be considered if available.
- The diagnosis of gas gangrene is a clinical one. Neither the isolation of
clostridia nor the presence of gas in tissue is diagnostic of the condition.
- For clostridial infection with or without myositis/myonecrosis (gas gangrene), use:
benzylpenicillin 2.4 g (child: 60 mg/kg up to 2.4 g) IV, 4-hourly.
- For patients with immediate penicillin hypersensitivity, use:
metronidazole 500 mg (child: 12.5 mg/kg up to 500 mg) IV, 8-hourly.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-223-320.jpg)

![renal colic
[created by
Paul Young
02/10/07]
definition
aetiology
symptoms
investigations
treatment
classical presentation is of acute colicky pain radiating to the groin
as the stone descends in the ureter, the pain may localise to the abdominal
area overlying the stone & radiate to the groin
as the stone approaches the ureterovesical junction, lower quadrant pain
radiating to the tip of the urethra, urinary frequency & urgency & dysuria
are characteristic
1. MSU
- gross or microscopic haematuria occurs in approximately 90% of patients
2. imaging:
(i) CT
- sensitivity of CT approaches 100% & when CT is negative it reveals an alternative
diagnosis in 57% of patients
(ii) KUB
- KUB should be performed when CT reveals the presence of stones or if CT is not
available; 75-90% of urinary calculi are radioopaque
(iii) USS
- specificity is greater than 90% but sensitivity is only 11-24%
- an appropriate initial investigation in pregnancy
Urgent urological intervention is indicated for:
(i) obstructed infected upper urinary tract
(ii) impending renal deterioration
(iii) intractable pain or vomiting
(iv) anuria
(v) high grade obstruction of a solitary or transplanted kidney
acute colicky flank pain radiating to the groin associated with passage of a ureteric stone
signs
vital signs:
- often hypertension & tachycardia are present
- patient roles around the bed & tries to find a comfortable position
A. treatment of infection:
- infection proximal to a stone is suggested by fever, urinanalysis showing pyuria &
bacteruria & leucocytosis. Impaired GFR associated with obstruction inhibits entry
of antibiotics into the collecting system & requires emergency decompression by
means of either percutaneous nephrostomy or ureteral stenting; E. coli is the most
common organism & antibiotics should cover this
12% of the population have a urinary stone in their lifetime & recurrence approaches 50%
peritoneal signs are absent
tenderness over the costovertebral angle or lower quadrant may be present
owing to the shared splanchnic innervation of the renal capsule & intestines,
hydronephrosis may produce nausea & vomiting
B. treat pain & nausea. treatments for pain include:
- ketorolac 30-60mg IV or IM loading dose then 15mg IV or IM every 6 hours
- diclofenac 50mg PO 2-3Xs/day
- morphine sulphate 0.1mg/kg IM or IV every 4 hours
NB: because intractable pain is caused by renal capsule distention, treatment is
by decompression of the obstruction
C. likelihood of passage of ureteral stones
<2mm - pass in mean of 8 days & 3% need intervention
3mm - pass in mean of 12 days & 14% need intervention
4-6mm - pass in mean of 22 days & 50% need intervention
>6mm - unlikely to pass & 99% need intervention
NB: 2/3rds of stones will pass within 4 weeks of onset of symptoms;
a stone which has not passed within two months is unlikely to. Furthermore,
stones that are still symptomatic after 4 weeks have a complication rate of 20%
(including renal deterioration, sepsis & ureteral stricture)
uric acid stones can be suspected based on history of gout
1. radioopaque stones
2. radiolucent stones:
- uric acid stones
- matrix stones (made of organic material & seen in patients with urease producing bacteria)
- indinavir stones
D. uric acid stones:
- uric acid stones are unique in that they can be managed medically with
urinary alkalinisation; solubility of uric acid increases above 6.5
- Rx 20mmol of potassium citrate 2-3Xs/day with reassessment to ensure
urinary alkalinisation to pH 6.5-7.0
- imaging can be repeated at one month to ensure that dissolution has occurred
otherwise treatment should proceed as for a radioopaque stone
E. metabolic evaluation & prophylaxis
- renal deterioration is more likely from repeated episodes
- options for metabolic evaluation include:
(i) stone composition analysis
(ii) 24hr urine collection for volume, calcium, oxalate, uric acid
phosphate, sodium, citrate, creatinine & sulphate +/- cystine
(iii) serum calcium & uric acid
- general advice includes restriction of animal protein & salt,
drinking enough to produce 2L urine / day
- specific abnormalities should be treated](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-225-320.jpg)
![neurocritical
care
[created by
Paul Young
02/10/07]
general
- The birth of neurocritical care stemmed from the appreciation that an already
affected brain (primary injury) is greatly influenced by systemic alterations that
may adversely affect its function (secondary injury).
outcome
measures
monitoring
therapy
acute ischaemic stroke:
(i) rt-PA:
- rt-PA within 3 hrs of symptom onset can result in clinical and statistical significant improvement
- at least 30% of treated patients will be completely independent 3 months after treatment.
(ii) intraarterial thrombolysis:
- may increase the window treatment to 6 hrs
- may be used as rescue therapy after intravenous thrombolysis
(iii)ultrasound-enhanced systemic thrombolysis
- uses transcranial doppler to enhance thrombolysis
intracerebral haemorrhage
- One of the major discoveries has been the realisation that intraparenchymal hematomas
grow in about 38% of patients within 3hrs of onset . Such growth may result in increased mortality.
(i) recombinant factor VIIa
- The most promising intervention to limit hematoma growth with resulting improved mortality and
functional outcome thus far has been the administration of recombinant activated factor VIIa.
(ii) Surgical evacuation
- Surgical evacuation of intracerebral hematomas within 24 hrs has not shown benefit when
compared with initial conservative treatment
- The one group of patients who may benefit from surgery with improved functional outcome is that
with cerebellar hematomas.
(iii) Blood pressure management:
- On the one hand, there is the risk of increasing the size of the hematoma if blood pressure remains
elevated, and on the other, there may be the theoretical risk of causing cerebral ischemia if blood
pressure is reduced.
- A prospective study is under way to evaluate the optimal blood pressure control level in these patients.
subarachnoid haemorrhage:
(i) cerebral vasospasm treatments:
- Cerebral vasospasm is a frequent cause of cerebral ischemia after subarachnoid hemorrhage.
- Calcium antagonists, particularly nimodipine and possibly magnesium, reduce the risk of poor
outcome and cerebral ischemia.
- volume expansion has been commonly used under the assumption that hypovolemia is related
to cerebral ischemia. However, convincing evidence of its benefit is lacking.
(ii) hypothermia:
- The use of intraoperative (i.e., during aneurysm clipping) hypothermia does not improve clinical outcome
(iii) coiling vs clipping:
- randomized trial revealed that in patients with ruptured cerebral aneurysms, for which both endovascular
coiling or surgical clipping are treatment options, the outcome in terms of disability at 1 yr is better for
patients undergoing endovascular coiling
(iv) hypoxic ischaemic insult:
- Evidence from randomized controlled trials has demonstrated that institution of mild-to-moderate
hypothermia results in improved survival and functional outcome of these patients.
(v) traumatic brain injury:
- patients admitted to specialized trauma centers are more likely to experience a reduced hospital
length of stay and mortality, with improved functional outcome.
- aggressive management of hypotension in the prehospital setting is important. A recent randomized
clinical trial of aggressive fluid management in the prehospital setting revealed decreased mortality, most
likely related to avoidance of hypotension.
- induced hypothermia has also been applied to patients with severe traumatic brain injury. Studies
have revealed that induced hypothermia may confer benefit particularly to those patients with elevated
intracranial pressure. However, the routine use of this treatment remains controversial.
(vi) treatment of fever:
- Elevated core body and brain temperature is associated with worsening neurologic injury and
functional outcomeof critically ill neurologic patients, regardless of the type of injury. Such
association is very important because fever is a frequent occurrence in neurologic patients while
in the ICU.
- What remains to be answered is whether effective fever reduction results in significantly improved
functional outcome and mortality rates in these patients.
icp
waveforms](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-226-320.jpg)
![neuroimaging
[created by
Paul Young
27/11/07]
CT
general:
- the most widely used imaging modality for evaluation of critically
ill patients with CNS pathology. It is widely available, rapid &
accurate and has virtually no contraindications in the acute setting
- the clinical utility may be increased by multiple methods including
contrast enhancement, window techniques and various reconstructions
- with contrast agents, lesions that cause a breakdown of the blood brain
barrier as well as normal or abnormal vascular structures 'light up'
- spiral or helical CT allows rapid imaging through a large volume of the
body usually with a single breath-hold. Rapid, thin-section axial images
can be obtained with very little artefact & they can be merged and reproduced
in any plane
- xenon CT involves the inhalation of xenon gas over a period of time with
sequential cuts and subsequent calculations of xenon uptake. This technique
is valuable for measuring cerebral blood flow
brain
imaging
patterns
of
disease
oedema:
- cerebral oedema is caused by localised or diffuse abnormal accumulation of water and sodium.
This differs from cerebral engorgement caused by vasodilation or obstructed venous outflow
- three types of oedema have been described:
(i) vasogenic oedema:
- is the result of increased capillary permeability and involves mainly white matter
- most often associated with tumour, abscess or trauma but can also been seen
with infarct and ischaemia
(ii) cytotoxic oedema:
- is the result of cellular swelling and involves both grey and white matter.
- ischaemia, anoxia and hypoosmolar states are the most common causes
(iii) interstitial oedema:
- is the result of cerebrospinal fluid into the periventricular white matter
- this form of oedema is secondary to conditions that impede CSF absorption
- except for location, the CT and MRI appearance of all types of oedema is similar
haemorrhage:
- intracranial haemorrhage may be parenchymal or extraaxial (epidural, subdural or subarachnoid)
- parenchymal haemorrhage can be traumatic in origin but is more likely non-traumatic from
underlying disease such as hypertension, neoplasia or vascular anomaly
- extradural and subdural haematoma are most likely the result of trauma
- subarachnoid haemorrhage is most often traumatic but may be associated with ruptured aneurysm
- the imaging appearance of haemorrhage is dependent on the age of the haemorrhagic event.
- On CT, acute haemorrhage typically appears as hyperdense; however they may appear as
isodense in anaemic patients or in patients with coagulopathy who fails to produce clot retraction.
As clot retracts the density may rise for 2 to 3 days after the initial event. The CT appearance then
gradually reduces in density progressing through an isodense stage at 1-6 weeks depending on
the size and finally a hypodense stage
- MRI appearances of haemorrhage are more complicated because of the varying paramagnetic
properties of blood breakdown products
mass effect & herniation:
(i) subfalcine herniation
- occurs when the medial surface of a hemisphere is compressed against or
displaced beneath the falx
- early signs may appear as compression or distortion of the lateral ventricles
- later stages are recognised by deviation of the falx & identification of midline
structures that are crossing the midline
(ii) transtentorial herniation
- occurs when a mass arising on either side of the tentorium results in brain herniation through
the tentorium results in brain herniation through the tentorial incisura
- descending transtentorial herniation is caused by a supratentorial mass that
displaces the medial temporal lobe throught the incisura. On CT the herniated brain pushes against
and rotates the brainstem producing widening of the ipsilateral brainstem cistern and effacement of
the contralateral cistern
- ascending transtentorial herniation is caused by an infratentorial mass that displaces the pons,
vermis & adjacent portions of the cerebellar hemispheres upward throught the incisura. On CT,
the brainstem cisterns are symmetricallyeffaced as the cerebellar vermis bulges up through the
incisura
(iii) tonsillar herniation
- occurs when the cerebellar tonsils are pushed through the foramen magnum
neoplasm
- On CT, low grade gliomas may appear as subtle non enhancing masses while higher grade gliomas
often demonstrate heterogenous enhancement with large areas of necrosis & vasogenic oedema
- On CT, metastatic lesions may be low density and enhancing masses as seen with breast
or lung carcinoma or they be high density with haemorrhagic components as seen with renal
cell carcinoma, melanoma & thyroid tumours
- MRI has high sensitivity but low specificity in evaluation of neoplasms
head
trauma
- CT is the primary modality for the initial evaluation of patients with head injury
- although MRI is more sensitive in detecting intracranial traumatic lesions, it is limited by a longer
examination time, less conspicuity of hyperacute haematomas & difficulty in monitoring patients.
MRI can identify small foci of old haemorrhage and gliosis and can evaluate the presence and extent
of diffuse axonal injury (shear injury) with greater sensitivity than CT
MRI
Disadvantages of MRI:
- MRI is contraindicated in patients with:
(i) pacemakers
(ii) certain cardiac valves
(iii) intraocular metal fragments
- careful screening is required for the presence of cerebral aneurysm clips
& other metallic devices, stents and surgical implants
- respirators and physiological monitors must be MRI compatible &
only oxygen cylinders composed of aluminium may enter the scanner
- delays result from all of the above precautions and modifications
- basic medical instruments such as stethoscopes,
haemostats, & scissors must remain outside the scanner
General:
- uses magnetic field gradients and radiofrequency pulses rather than ionising radiation
- many sequences that vary the MRI signal parameters are obtained allowing tissue
characterisation based on the tissue's inherent response to magnetic field and
radiofrequency pulses
- a gadolinium-based contast agent can be injected intravenously which allows
better visualisation of intracranial and intraspinal pathology
- diffusion weighted MRI is based on the evaluation of free versus restricted movement
of water molecules. Diffusion weighted MRI is now considered the standard sequence
in evaluation of acute stroke because it is more sensitive than standard MRI for identification
of acute stroke and for differentiating stroke for other pathologies
other
modalities
nuclear medicine studies:
- evaluation of CNS pathology with nuclear medicine techniques is still undergoing investigation.
- the major use for this technique is in demonstrating absence of cerebral blood flow in
patients in whom clinical brain death testing and cerebral angiography are precluded
angiography:
- percutaneous transfemoral catheterisation is used to evaluate cerebral and spinal vascular
anatomy and integrity.
- cerebral angiography is an invasive procedure & imposes some risks. The overall
complicationrate is 2-4% with most complications being minor and transient such as groin
haematoma,infections and minor allergic reactions. More severe complications such as
cerebral infarction,seizure and death occur infrequently
- cerebral angiography remains the gold standard for establishing the presence of cerebral
aneuryms, or vascular malformations
- interventional neuroradiology techniques include embolisation of vascular tumours,
aneurysms,and AV malformations; stent placement; angioplasty and thrombolysis
advantages of CT:
(i) useful for diagnosis of CNS trauma, SAH, ICH, haemorrhagic and ischaemic stroke,
hydrocephalus, cerebral oedema and the presence of space occupying lesions
(ii) lower cost than MRI
(iii) readily available with short examination time
(iv) safe in the presence of pacemakers, surgical clips & ferromagnetic substances
disadvantages of CT:
(i) the need to transfer the patient to a site where resuscitation & monitoring facilities are limited
(ii)) the need to sedate and possibly intubate patients who are agitated
(iii) low sensitivity in acute stroke
(iv) low sensivity for detecting brainstem lesions
(v) potential need for iv contrast with risk of anaphylaxis and renal failure
Advantages of MRI:
(i) provide superior contrast and resolution of grey & white matter compared with CT facilitating easy
identification of deep structures within the brain & visualisation of the brainstem & posterior fossa
(ii) use of non-ionising energy
vascular
lesions
- although CT only demonstrates about half of infarct within the first 48 hours, it remains the imaging
modality of choice in evaluating patients with symptoms of TIA, RIND or completed stroke
- in the acute setting, CT can identify the location and extent of infarction; distinguish
among ischaemic stroke, primary intracerebral haemorrhage & effectively exclude mimics
- hypertensive encephalopathy is a syndrome that occurs in patients with elevated blood pressure of
any cause. It causes hyperintensity of white matter at the grey-white junction on T2-weighted images.
Cortical and subcortical white matter changes occur primarily in the occipital lobes
- hypotensive encephalopathy can occur in patients who have suffered a severe hypotensive episode
or cardiac arrest. It is characterised by infarction in a watershed distribution
- venous infarction can occur in isolation and is associated with thrombosis of a dural sinus or large
draining vein. Venous infarction is typically haemorrhagic and primarily affects the white matter
- subarachnoid haemorrhage is evaluated by non contrast CT imaging.
- if the CT is positive and the patient is a surgical candidate
an angiogram is performed to identify aneurysms or AVMs
- for patients with suspected vasospasm, xenon CT and transcranial doppler have proved useful
- vascular malformations inlcude AVMs, capillary telangiectasia, cavernous
angioma & venous angiomas. They may not be visible on plain CT.
parenchymal
infection
- parenchymal infections include encephalitis, cerebritis & abscess
(i) encephalitis:
- MRI is more sensitive than CT for encephalitis & demonstrates the changes earlier
- On MRI, affected brain typically hypodense on T1-weighted images & hyperintense on T2-weighted images
- In herpes simplex encephalitis imaging studies show gyral oedema with a predilection for the temporal lobes
(ii)cerebritis & cerebral abscess
- an early phase of abscess formation that looks like encephalitis but is more focal in nature
- cerebral abscess produces a localised collection of pus surrounded by a fibrous capsule
- on CT, an abscess cavity demonstrates central hypodensity, a thin isodense wall & surrounding
low density oedema. Following contrast administration, there is enhancement of the capsule
(iii) extraaxial collections
- include ventriculitis, meningitis, subdural and extradural empyema
- MRI is generally the modality of choice and in general with both CT & MRI contrast is required
CT imaging in TBI](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-227-320.jpg)
![neuromuscular
cause of acute
respiratory
failure [created
by Paul Young
08/11/07]
spinal
cord /
AHC
lesions
(i) tetanus
(ii) amyotrophic lateral sclerosis
(iii) poliomyelitis
(iv) rabies
peripheral
nerve
(i) Guillain Barre
(ii) critical Ilness polyneuropathy
(iii) diptheria
(iv) porphyria
(v) Ciguatera poisoning
(vi) paralytic shellfish poisoning
(vii) pufferfish poisoning (tetrodotoxin)
(viii) thallium, arsenic or lead poisoning
neuromuscular
junction
(i) myaesthenia gravis
(ii) botulism
(iii) Lambert Eaton syndrome
(iv) organophosphate poisoning
(v) tick paralysis
(vi) snake bite
muscle
(i) polymyositis / dermatomyositis
(ii) acute quadriplegic myopathy
(iii) eosinophillic myalgy syndrome
(iv) muscular dystrophies
(v) mitochondrial myopathy
(vi) acute hypokalaemic paralysis
(vii) stonefish myotoxin poisoning
(viii) rhabdomyolysis
(ix) hypophosphataemia](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-228-320.jpg)
![non-cardiogenic
causes of
pulmonary
oedema
causes
pathophysiology
of cardiogenic vs
non-cardiogenic
pulmonary oedema
fluid movement = k[(Pc + OSMi) - (Pi + OSMc)]
general
- The most common cause of noncardiovascular pulmonary edema is ARDS.
- In most syndromes of noncardiovascular pulmonary edema a combination of factors
including inflammation, direct damage to the capillary-alveolar membrane, and
hypoxia causing leakage of the capillary-alveolar barrier and decreased alveolar fluid
clearance are prominent pathogenetic mechanisms
postoperative
- a relatively common finding, especially when the surgical procedures are extensive and
the patient is elderly and suffers from significant cardiac comorbidities.
- The pathogenesis of postoperative pulmonary edema is diverse. Cardiovascular factors
are major contributors to pulmonary edema in patients sustaining a postoperative
myocardial infarction, whereas alveolar capillary leakage and reduced alveolar fluid
clearance play a major role in postoperative pulmonary edema related to major infections.
- In the absence of predisposing risk factors, fluid overload may be the main reason for
pulmonary edema.
pregnancy-
related
General:
- Pulmonary edema is an uncommon complication of pregnancy.
- It usually occurs in the peripartum period from a combination of factors, including
mobilization of fluids and fluid administration, use of tocolytic treatment, and
preeclampsia.
Tocolytics:
- Tocolytic treatment use is the most common cause of pregnancy-related pulmonary
edema (26%). In most cases, multiple tocolytics that include a beta-mimetic agent are
administered, probably inducing a significant increase in systemic vascular resistance.
Cardiac disease
- In a further 26%, pulmonary edema is related to a preexisting cardiac disease that is
exacerbated during the peripartum period and in combination with the large volume shifts
during this period that induce pulmonary edema.
Fluid overload
- Fluid overload per se is the main etiology of pulmonary edema in 22% of patients. In
these cases pulmonary edema is related to a large volume transfusion of approximately 6
L over a short period of time.
Preeclampsia
- Finally, preeclampsia is the main cause of pulmonary edema in 18% of cases.
Preeclampsia causes pulmonary edema through a combination of cardiovascular (reduced
left ventricular contractility and increased systemic vascular resistance) as well as
noncardiovascular factors (endothelial damage leading to increased fluid leak into the alveoli).
Peripartum cardiomyopathy
- Peripartum cardiomyopathy is an important entity causing pulmonary edema but should
be listed among the causes of cardiovascular pulmonary edema.
postobstructive
- This syndrome occurs after the relief of either acute or chronic obstructions of the upper airways.
- The most common cause is relief of obstruction occurring during anesthesia, although
other acute causes of upper airways obstruction such as epiglottitis, croup, foreign bodies,
strangulation, tumors, goiter, vocal cord paralysis, and obstruction of endotracheal tubes
have been reported.
- Pulmonary edema develops minutes to hours after the relief of obstructions, and its incidence
may be up to 10% after relief of acute obstructions and up to 40% after relief of chronic obstruction
- The pathophysiology of postobstructive pulmonary edema is not known, but a combination
of increased pulmonary capillary pressure owing to significant negative pressure during the
obstructive period combined with hypoxia leading to decreased alveolar fluid clearance,
increased systemic vascular resistance due to sympathetic overflow, and stress failure of the
alveolar-capillary membrane have all been postulated as possible causative mechanisms.
neurogenic
- an uncommon complication of various neurologic insults such as head injury,
intracranial and subarachnoid hemorrhage, as well as some acute neurologic diseases,
including seizures, tumors, hydrocephalus, and neurosurgical procedures.
- The clinical course is highly variable.
- The syndrome is often acute and fulminant but may be subclinical and smoldering,
manifesting as a mild progressive shortness of breath.
- The pathogenesis of neurogenic pulmonary edema is probably related to a combination
of increased sympathetic discharge leading to both increased systemic vascular resistance
and decreased left ventricular contractility, as well as increased alveolar-capillary leakage.
- some authorities in the neurologic literature advocate the use of alpha-adrenergic blockers
such as phentolamine and phenoxybenzamine owing to the possible role of sympathetic
overflow in this syndrome. However, these treatment options have never been
examined in a prospective, controlled study and hence should be used with caution.
re-expansion
- Pulmonary edema may occur after evacuation of a large pneumothorax or pleural effusion.
- The pathogenesis is not known, but leaks in the alveolar capillary membrane after
prolonged atelectasis and rapid re-expansion were suggested by some authors. The
treatment is symptomatic.
- The prognosis is not known, although in some older series a mortality of up to 20% was
described.
postpneumonectomy
- Pulmonary edema develops in 2.5% to 4.5% of patients after pneumonectomy.
- The pathogenesis of this syndrome is unknown. However, a combination of large fluid
transfusion, excessive negative pressure in the operated hemithorax due to underwater
suction systems, major lymphatic interruption related to extensive surgery, and damage to
the alveolar-capillary membrane have been implicated as possible causes.
- The fatality of this syndrome is significant, up to 85% in one series. Hence, prevention
is of great importance.
high-altitude
- a syndrome related to climbing to high altitudes.
- Its exact pathophysiology is unknown, but in a few recent studies it was demonstrated
that a combination of hypoxia-induced vasoconstriction leading to increased pulmonary
capillary pressure and alveolar fluid transudation together with decreased alveolar fluid
clearance leads to alveolar fluid accumulation and edema.
- The clinical presentation is typical, ranging from cough to full-blown respiratory failure.
- The treatment includes oxygen administration, rapid descent to lower altitudes or
simulated descent by a hyperbaric chamber, and possibly administration of calcium
antagonists. Furosemide and dexamethasone are probably not efficacious.
exertional
- Pulmonary edema has been reported to occur during and especially after strenuous
exercise and diverse sports activities and is especially common after prolonged swimming in cold water.
drug, substance
& toxic inhalation
- The most common cause of drug-induced pulmonary edema is the use of cardiodepressants
such as beta-adrenergic blockers and some calcium blockers and antiarrhythmics.
- Pulmonary edema has been associated with the intake or toxicities of drugs that provoke
edema through different mechanisms.](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-229-320.jpg)
![normal
anion gap
acidoses
[created
by Paul
Young
15/12/07]
general
- In hyperchloraemic acidosis, the anion-gap is normal (in most cases). The anion that
replaces the titrated bicarbonate is chloride and because this is accounted for in the anion
gap formula, the anion gap is normal.
- if hyponatraemia is present the plasma [Cl-] may be normal despite the presence of a
normal anion gap acidosis. This could be considered a 'relative hyperchloraemia'.
reasons
why high
AG acidoses
may give
a normal AG
1. One possibility is the increase in anions may be too low to push the anion gap out of the reference range.
- In lactic acidosis, the clinical disorder can be severe but the lactate may not be grossly high (eg lactate of
6mmol/l) and the change in the anion gap may still leave it in the reference range. So t](https://image.slidesharecdn.com/medicineinmindmaps-150716131716-lva1-app6892/85/Medicine-in-Mind-Maps-230-320.jpg)