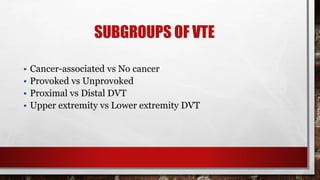
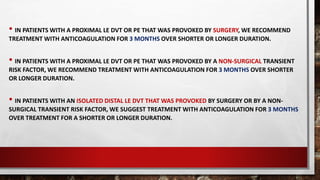
- The 44-year-old man presented with an unprovoked left proximal leg deep venous thrombosis 3 months ago and has since been stable on warfarin therapy with therapeutic INR levels. For unprovoked proximal DVT, guidelines recommend extended anticoagulation therapy indefinitely due to the risk of recurrence, unless the patient has a high bleeding risk. Therefore, the most appropriate management would be to continue anticoagulation indefinitely (Option A).