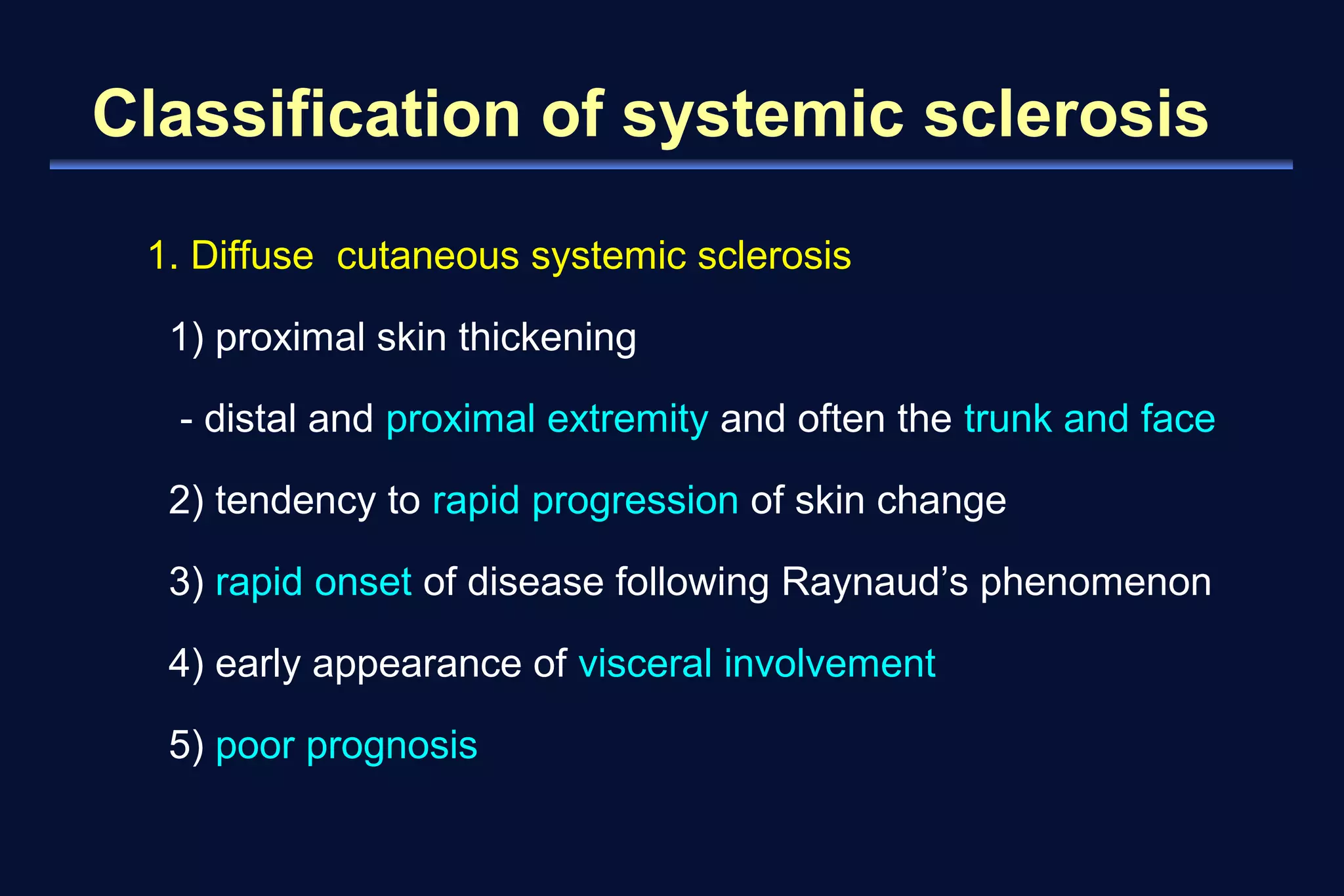
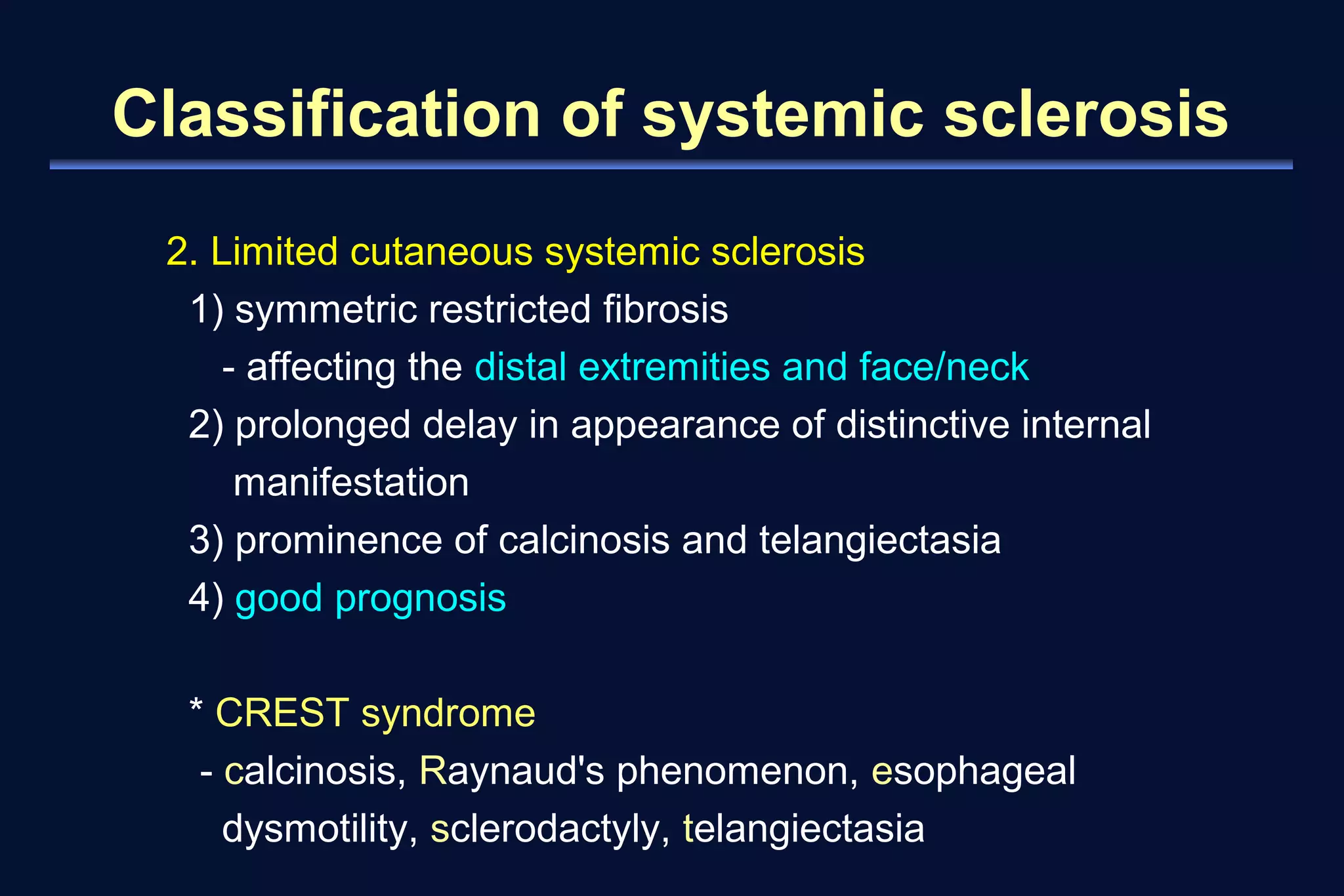
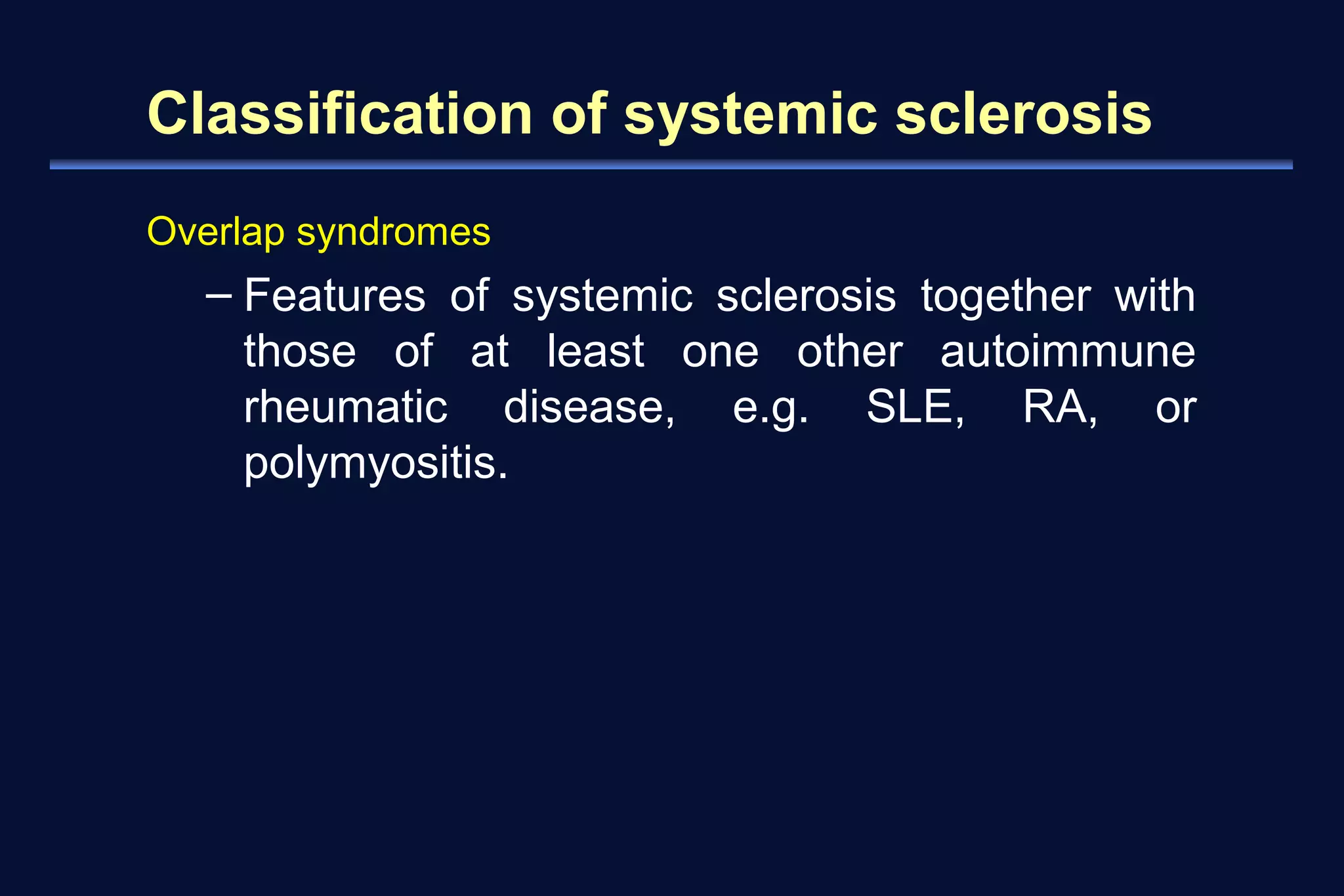
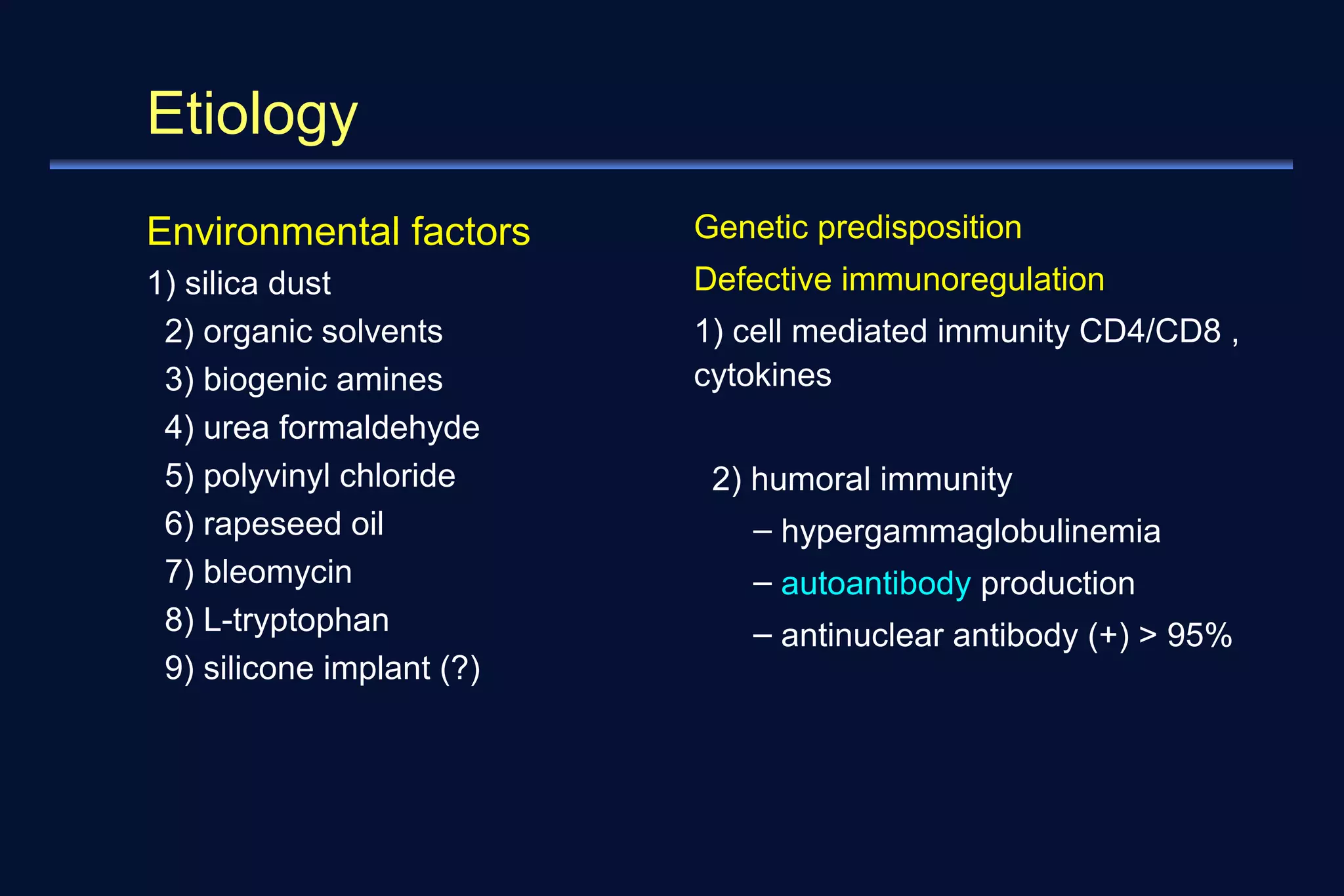
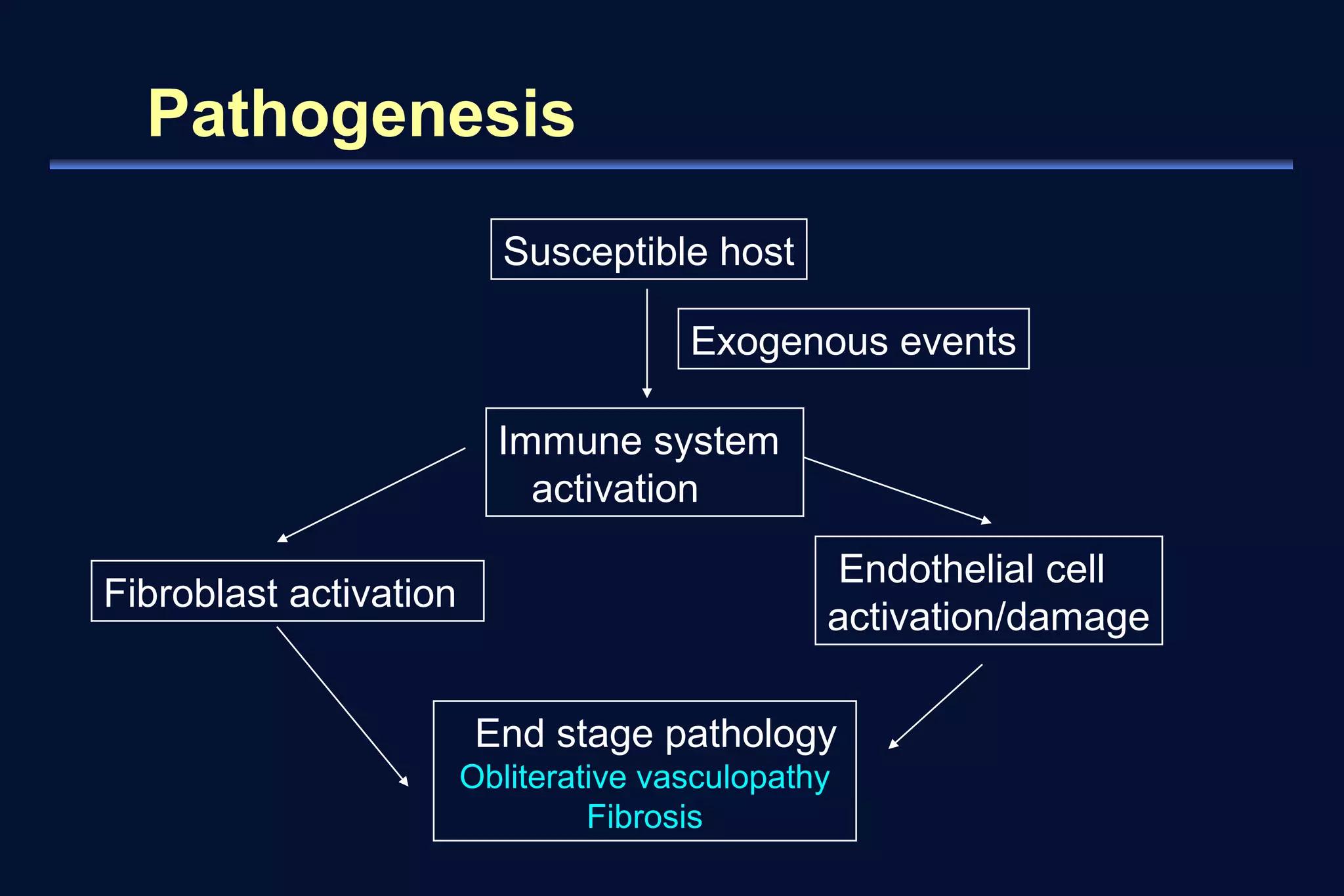
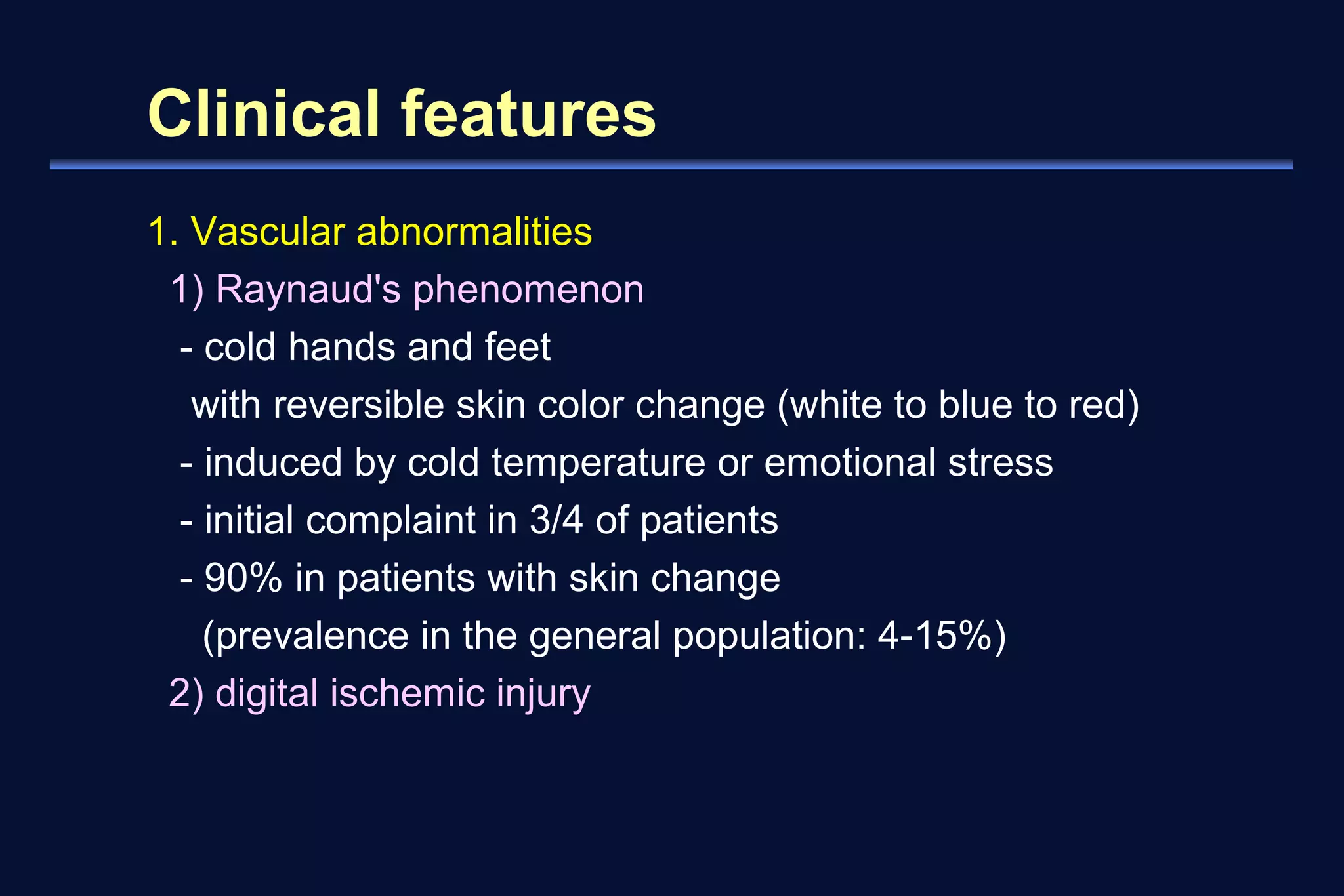
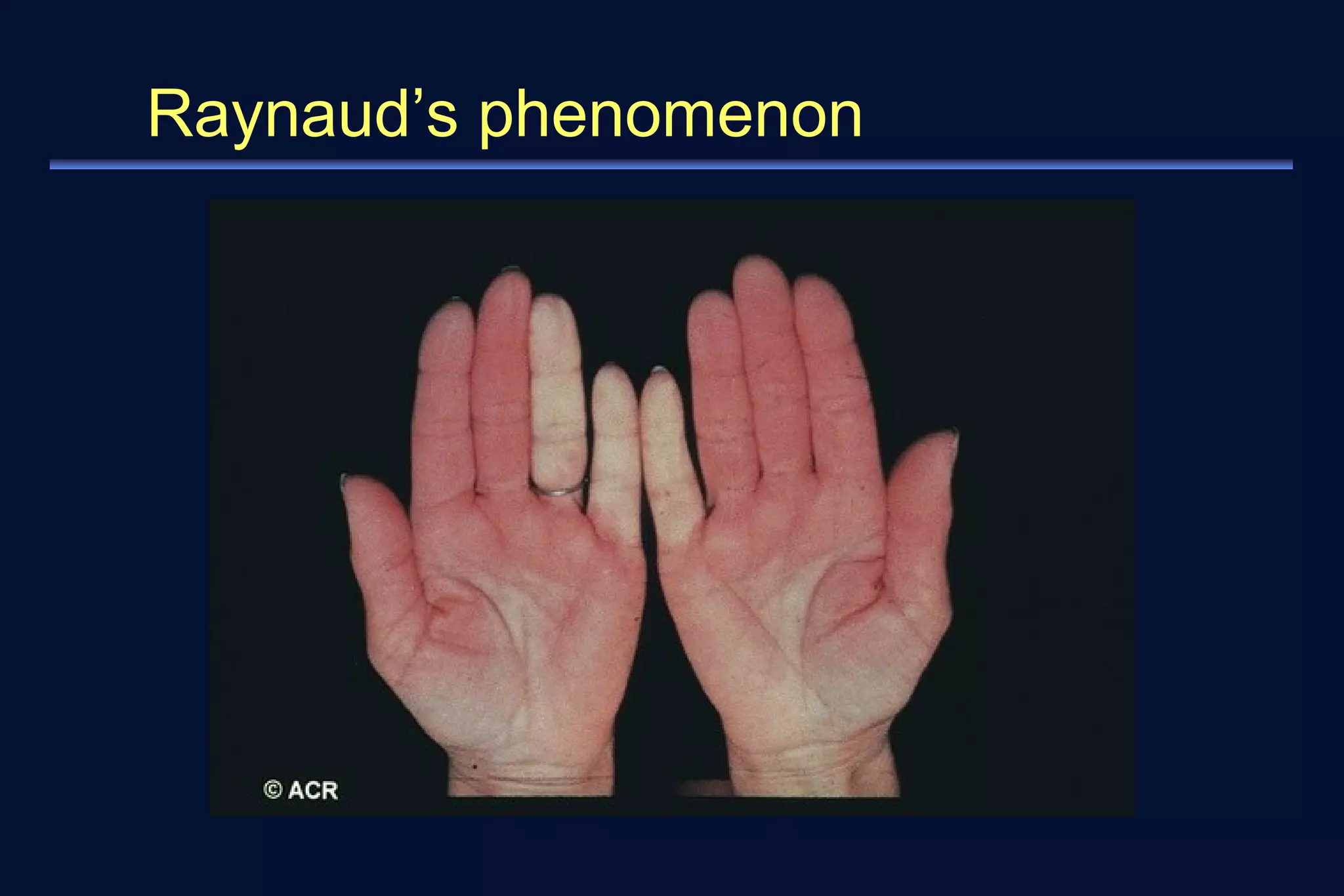
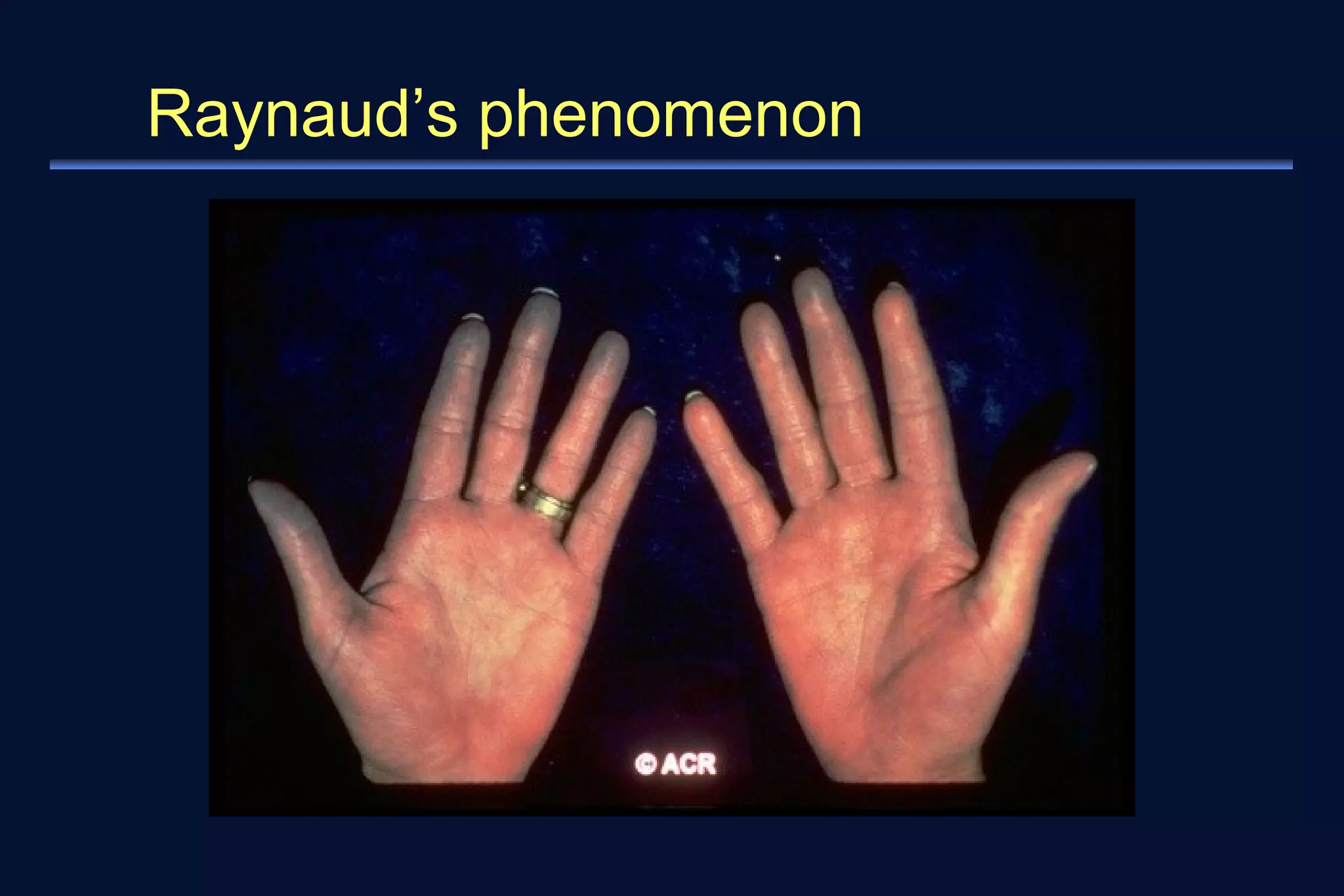
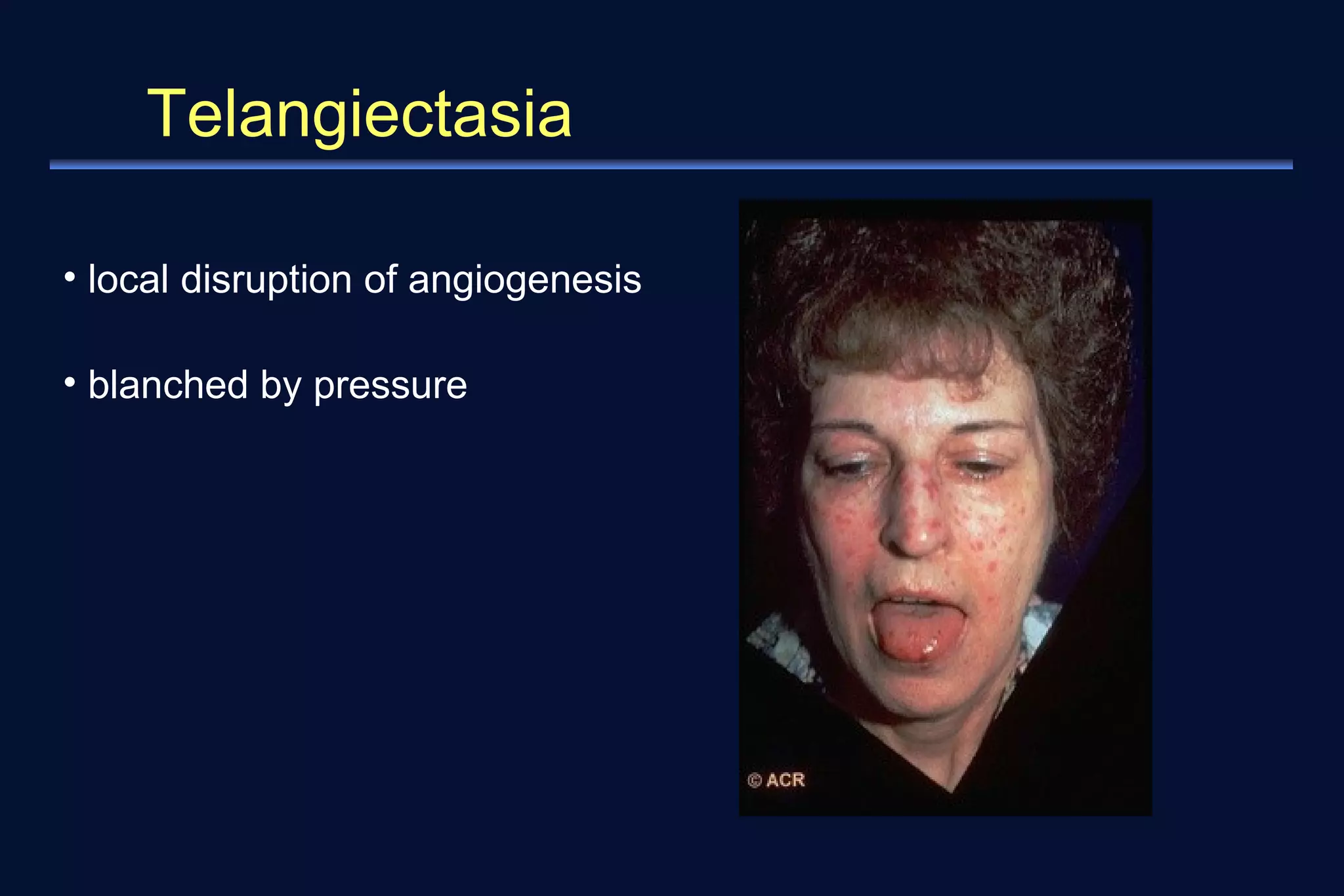
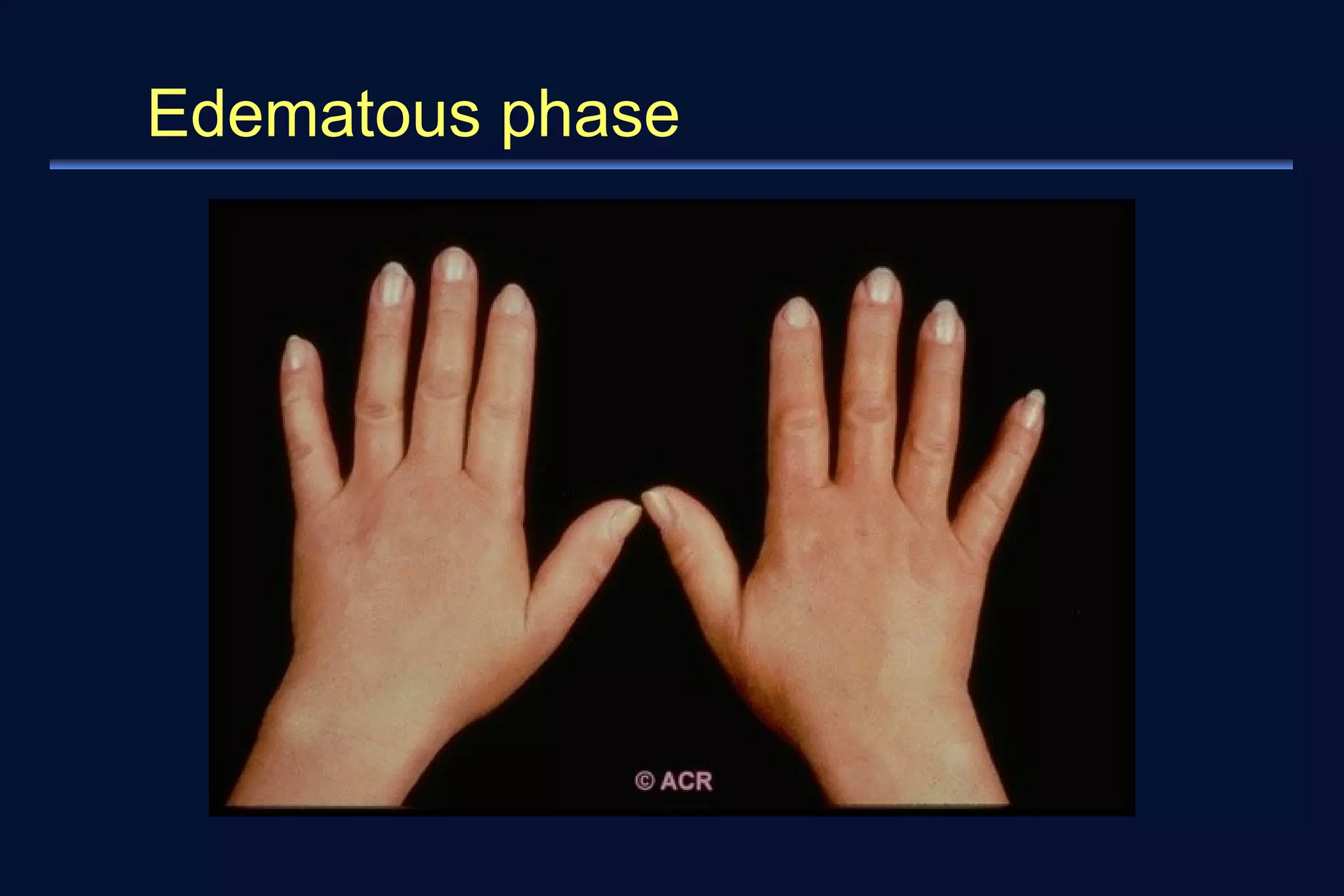
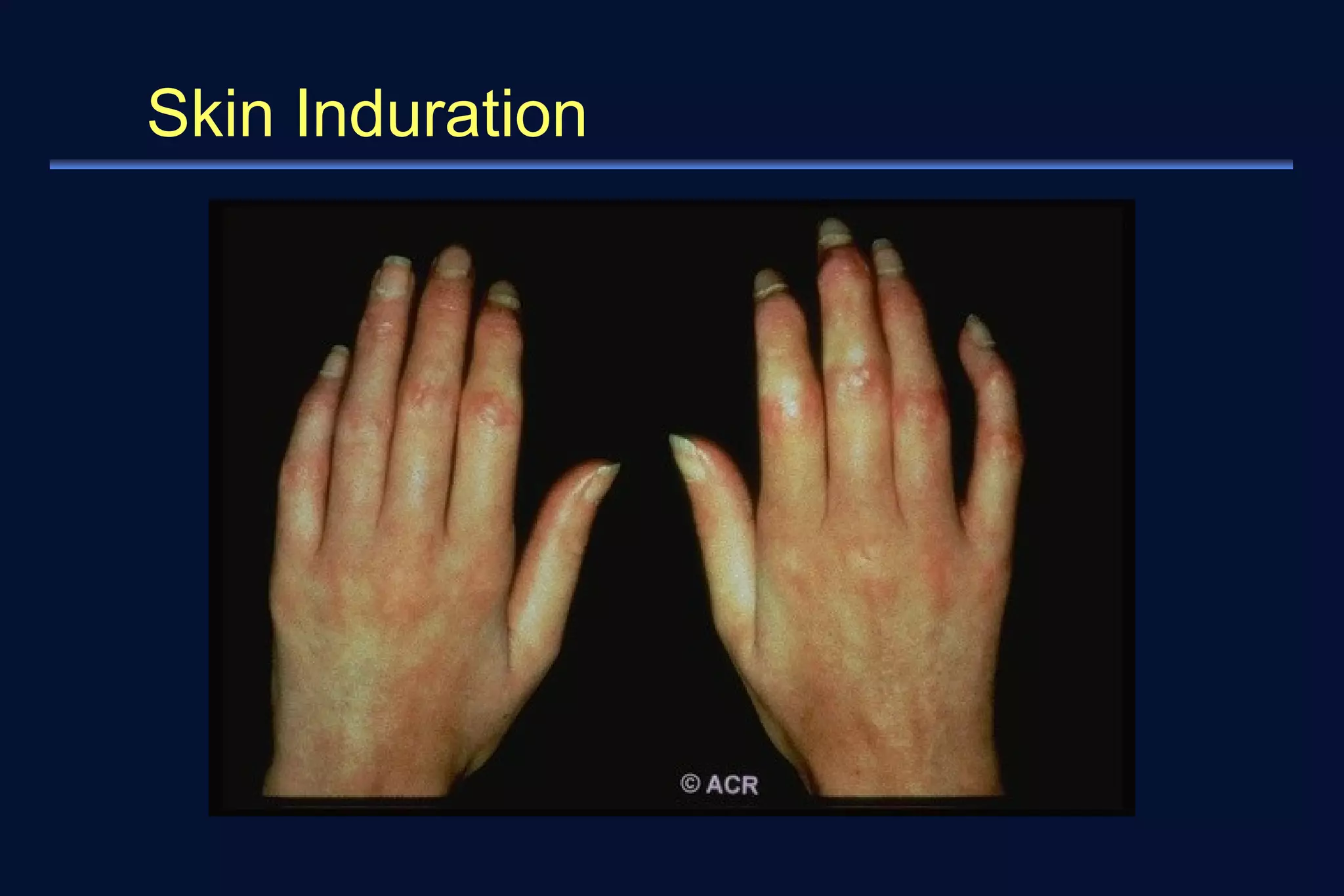
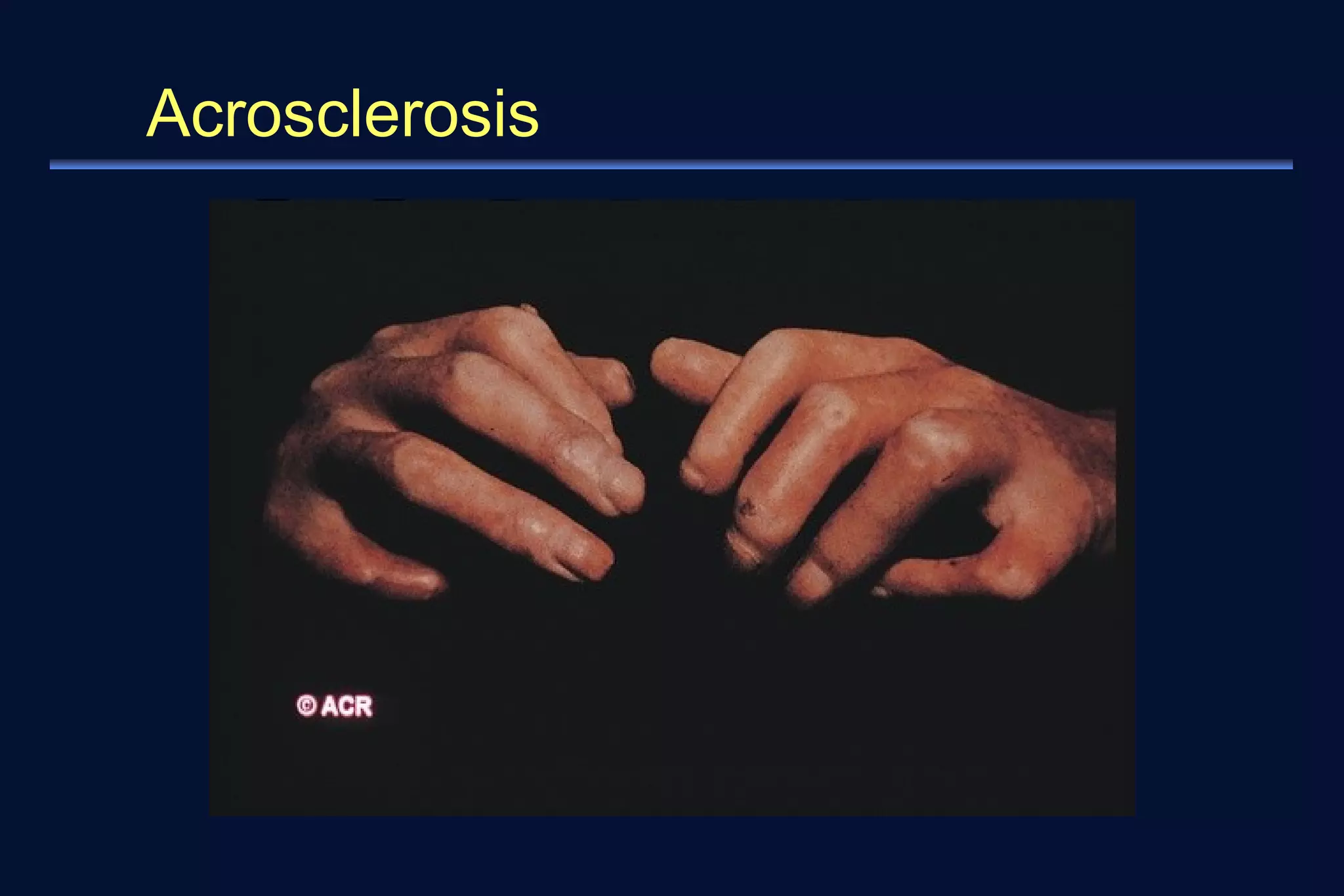
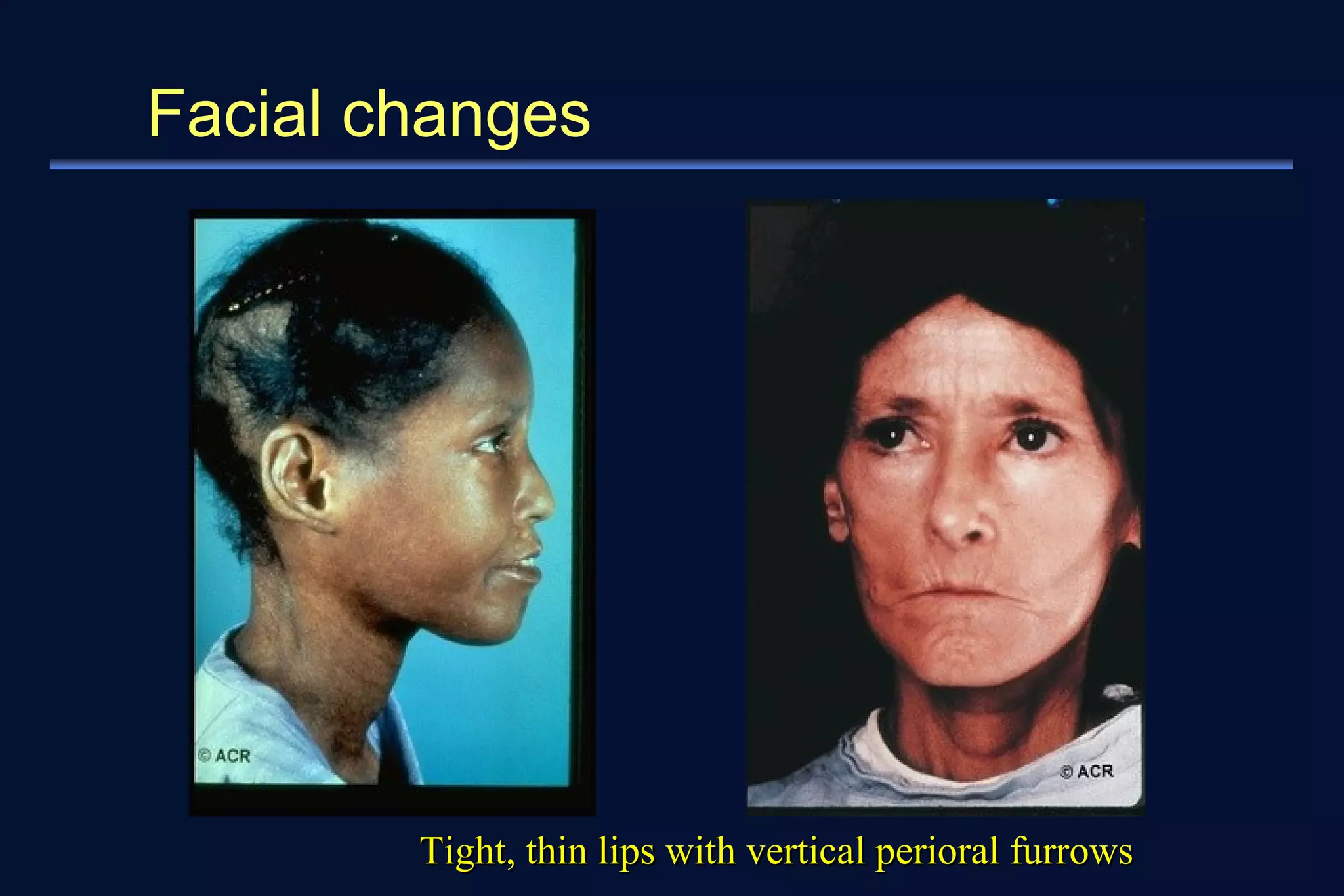
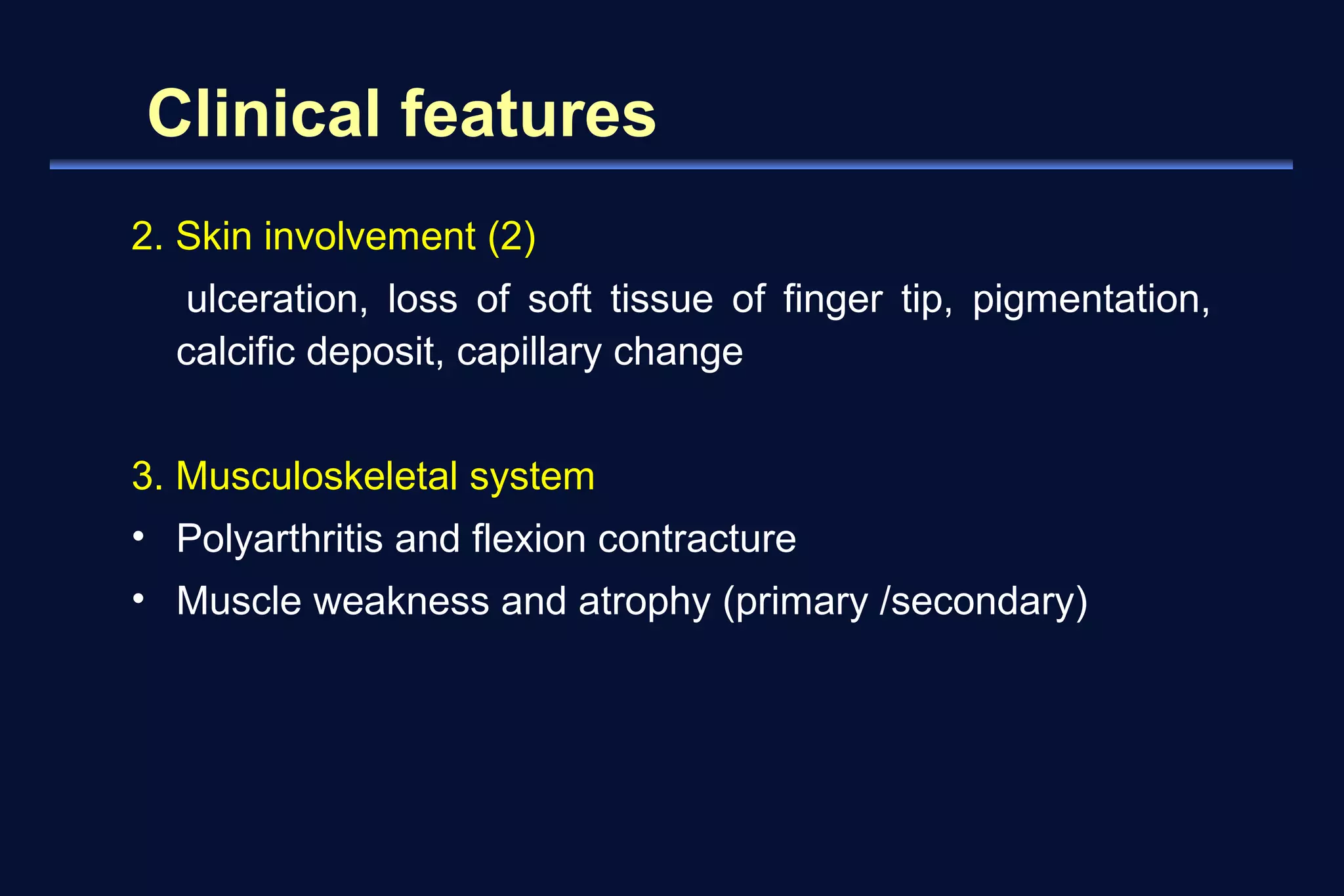
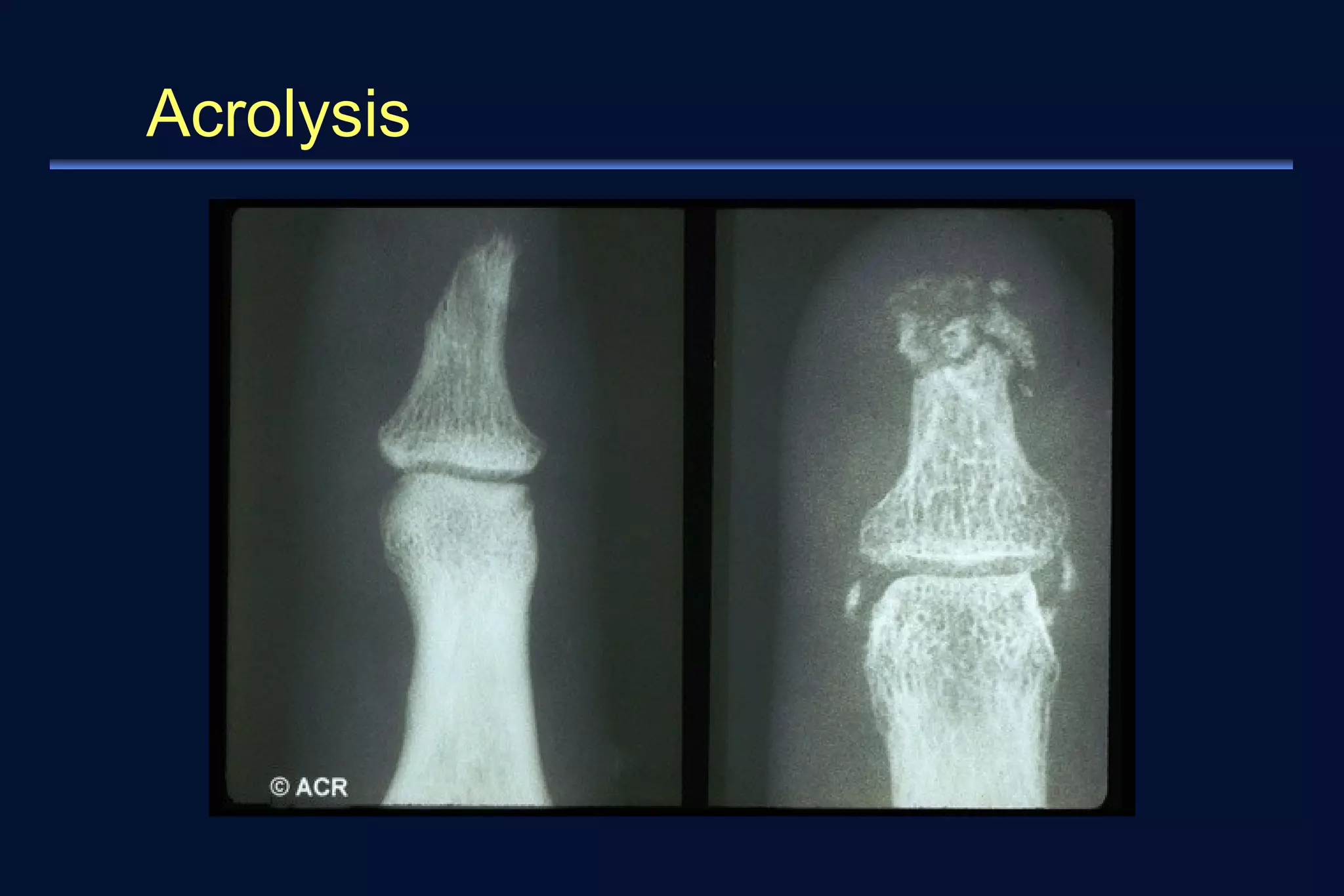
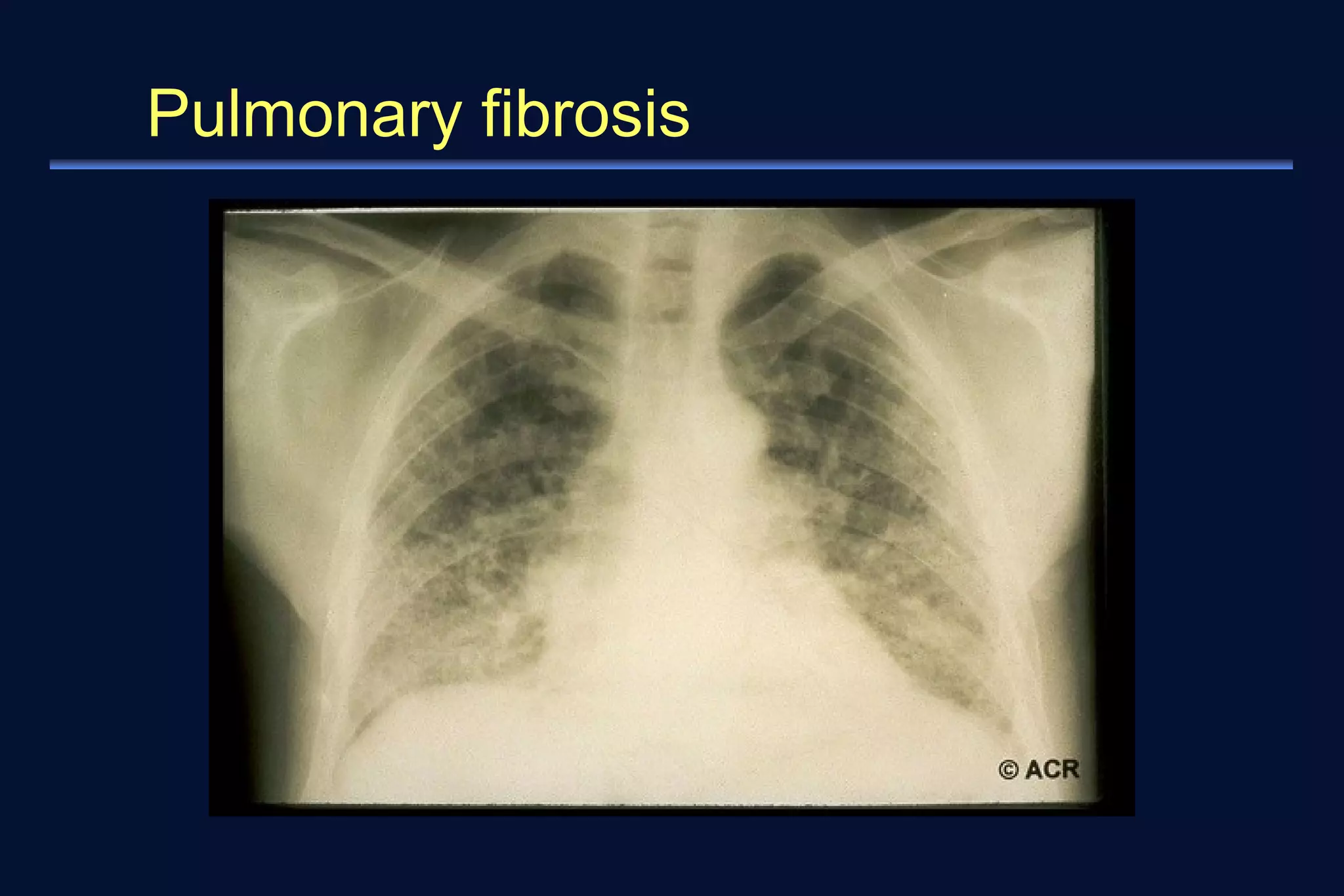
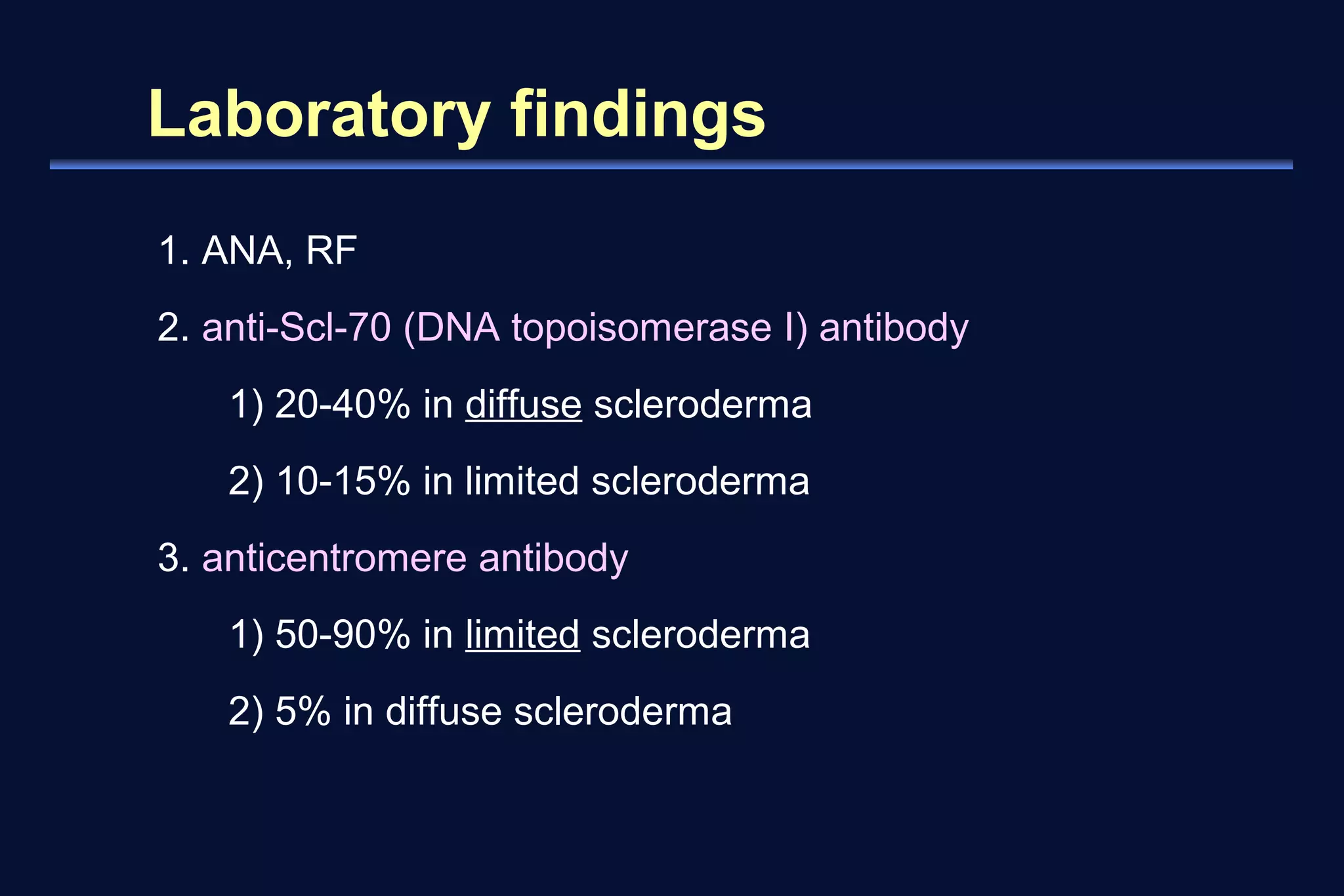
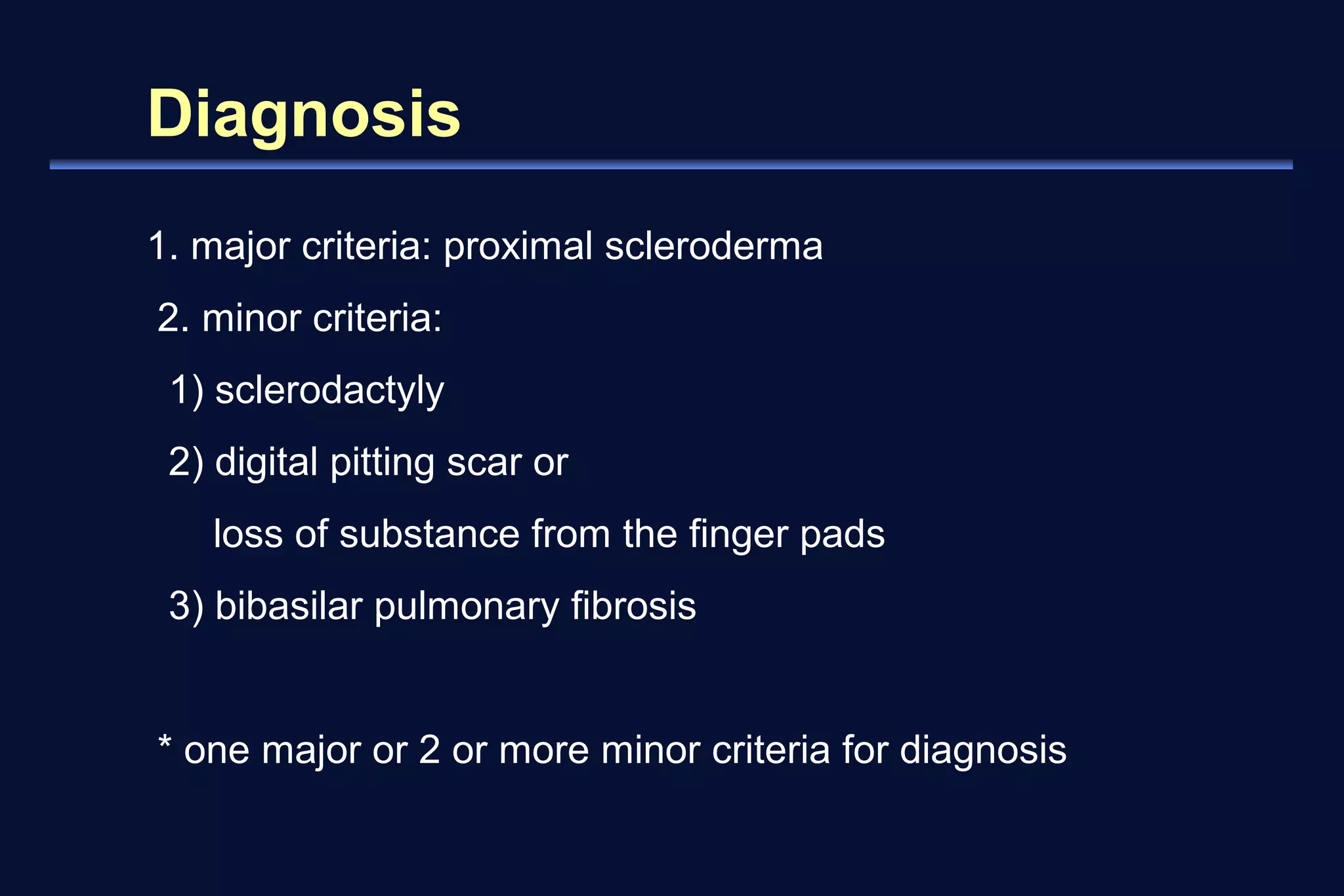
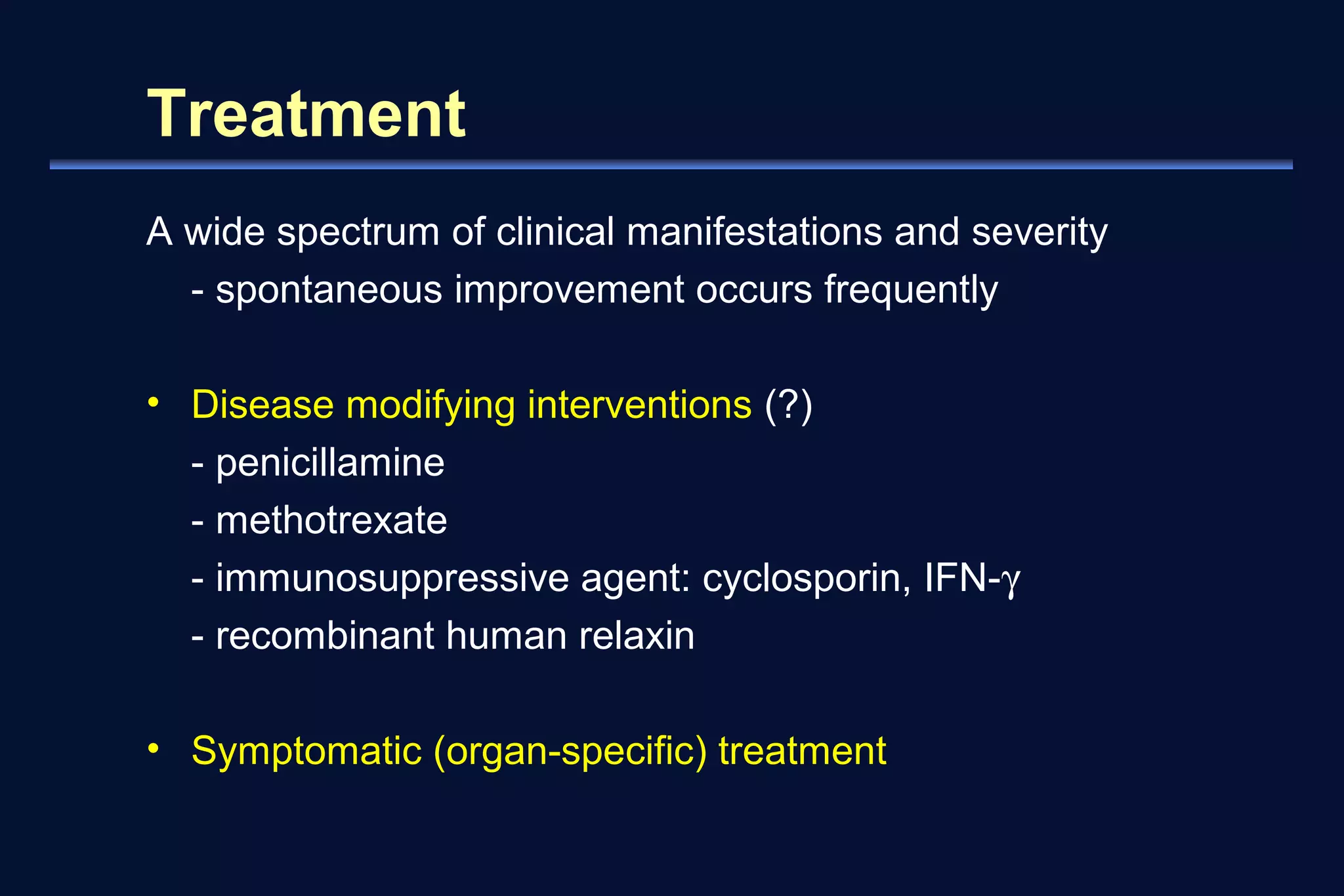
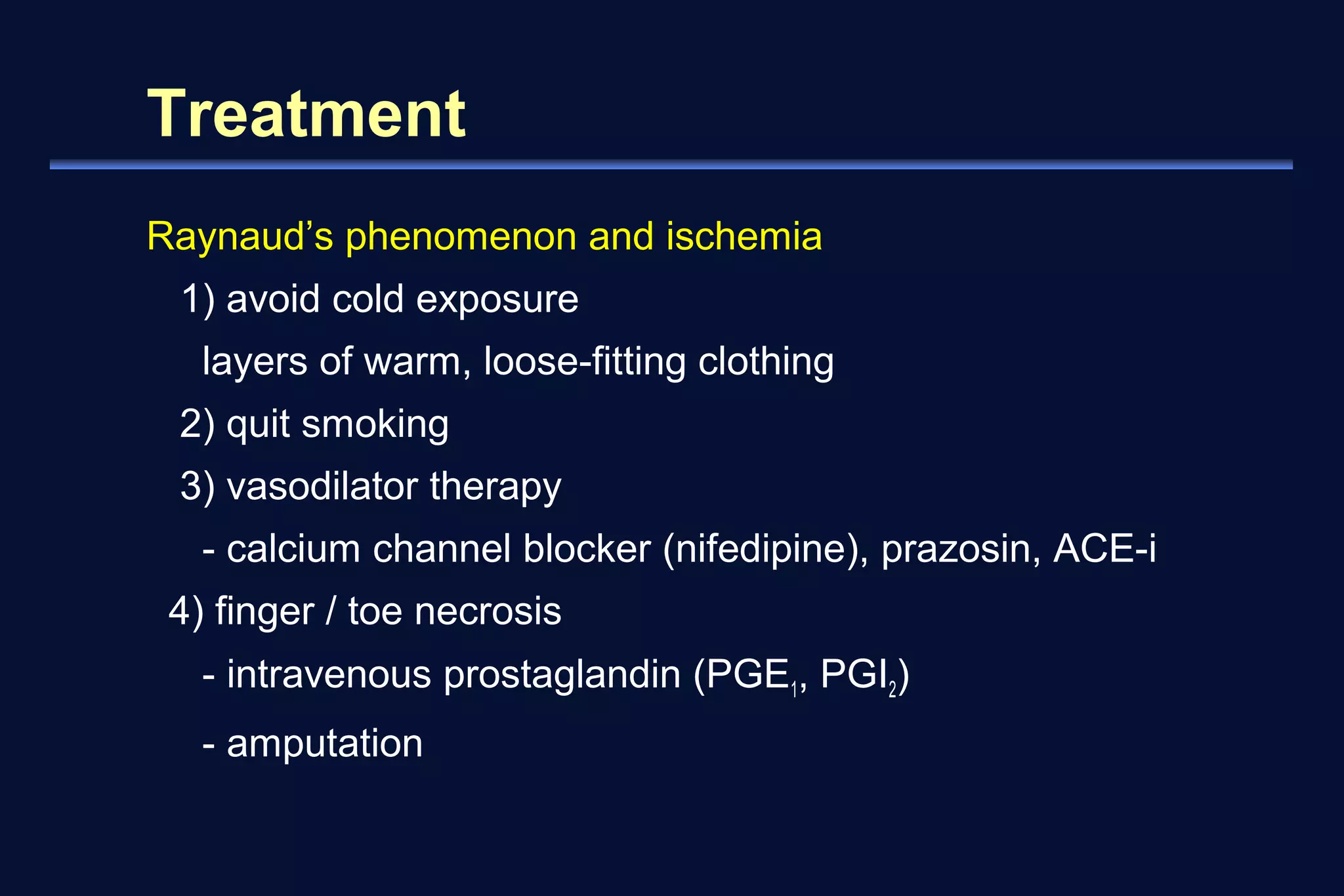
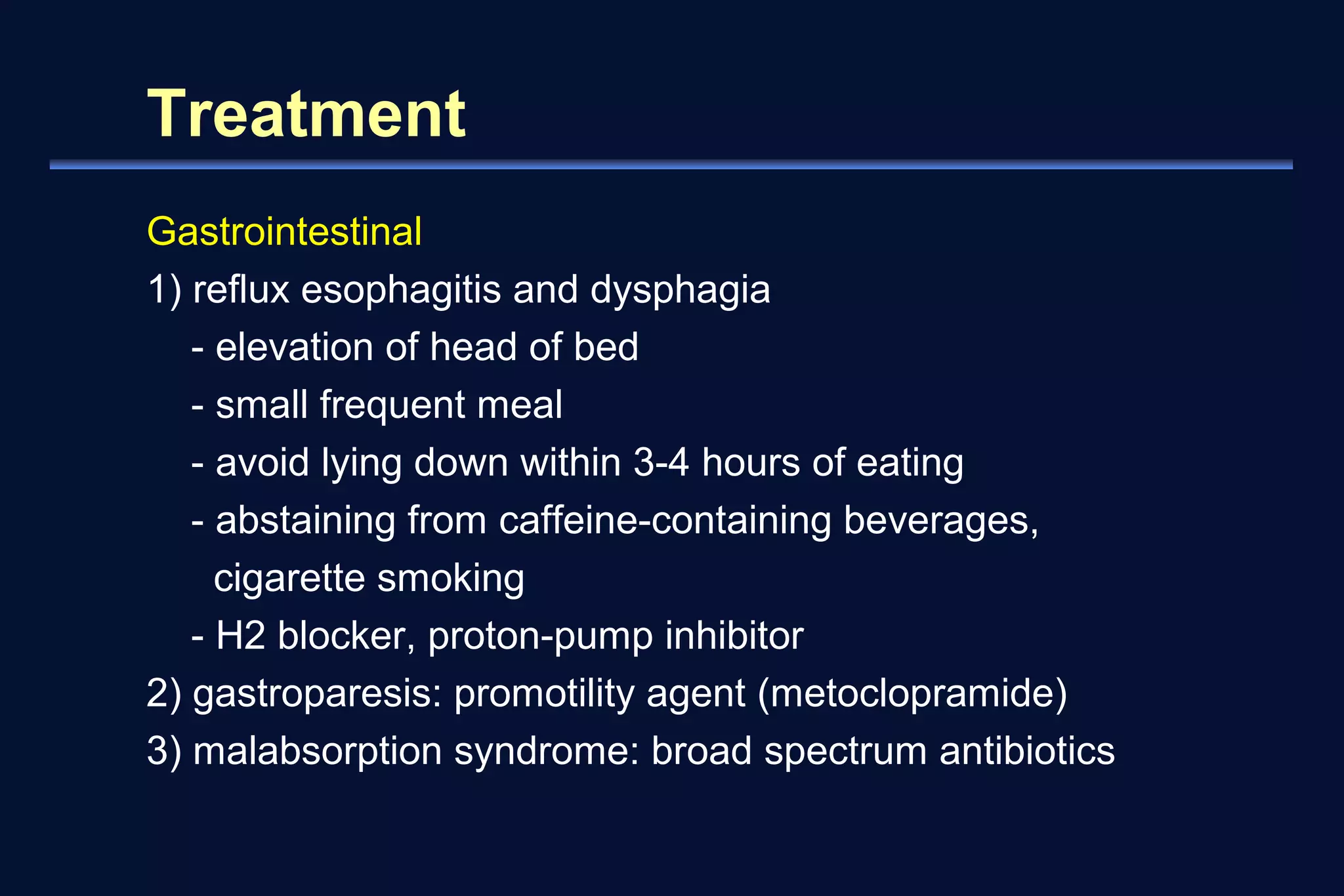
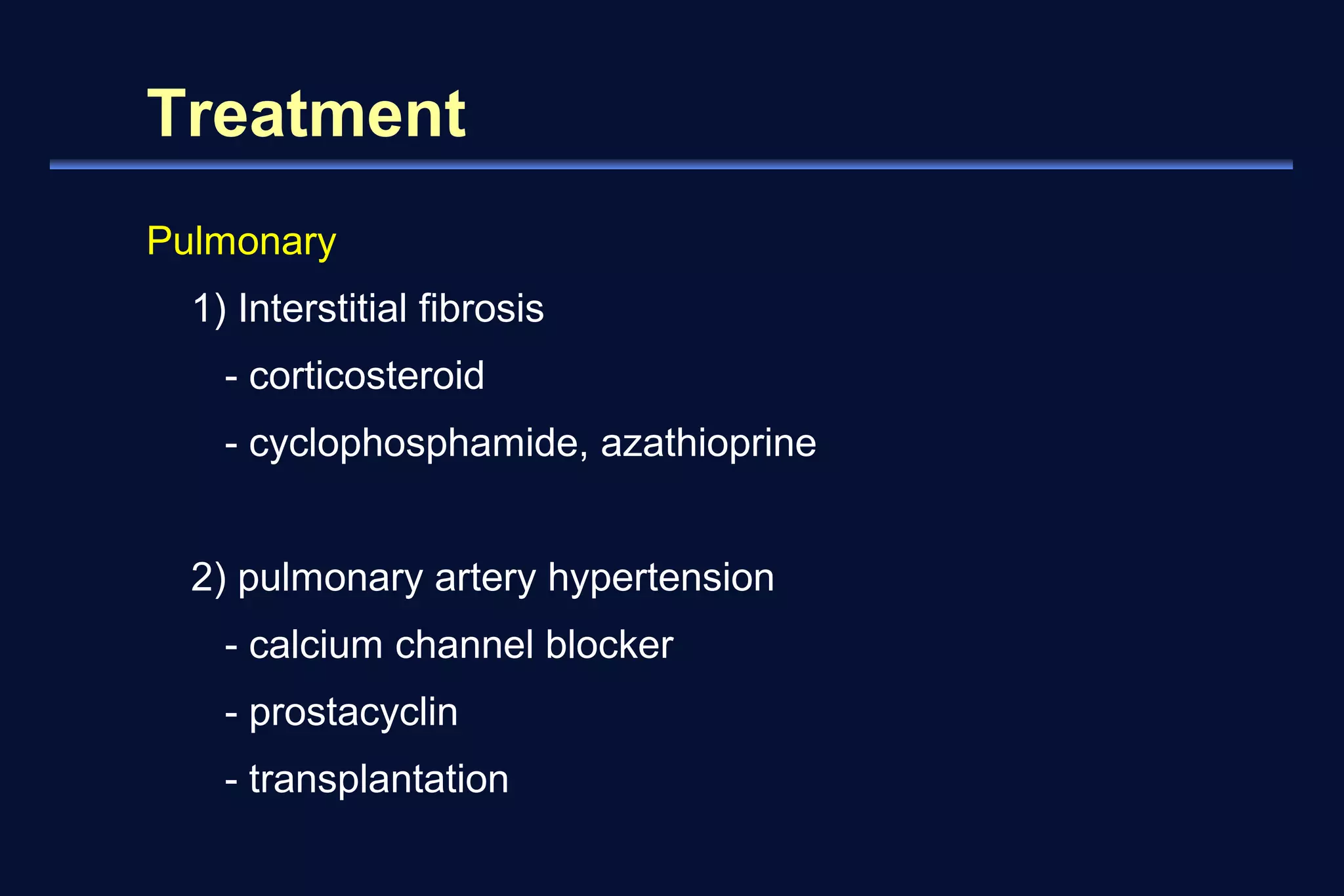
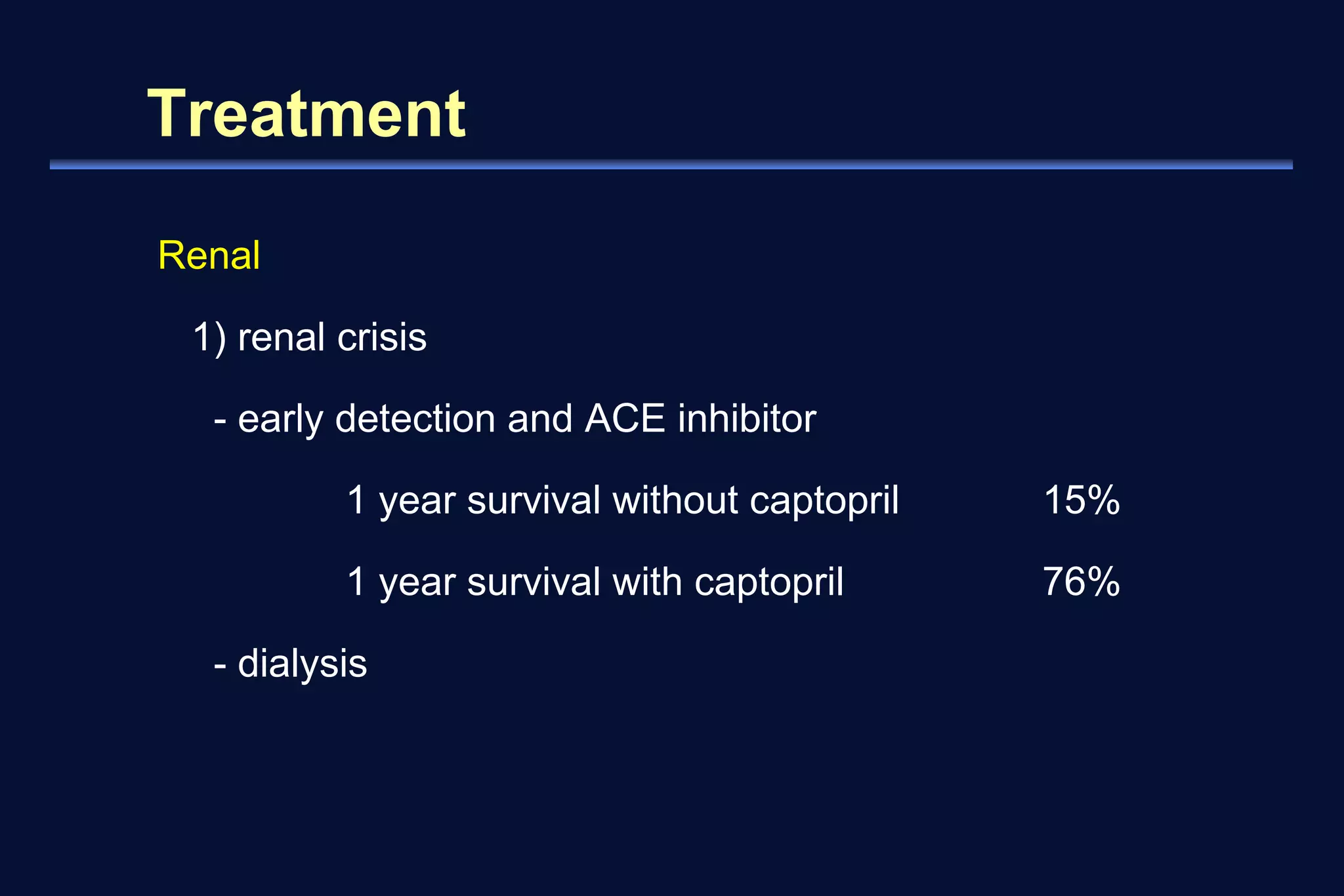
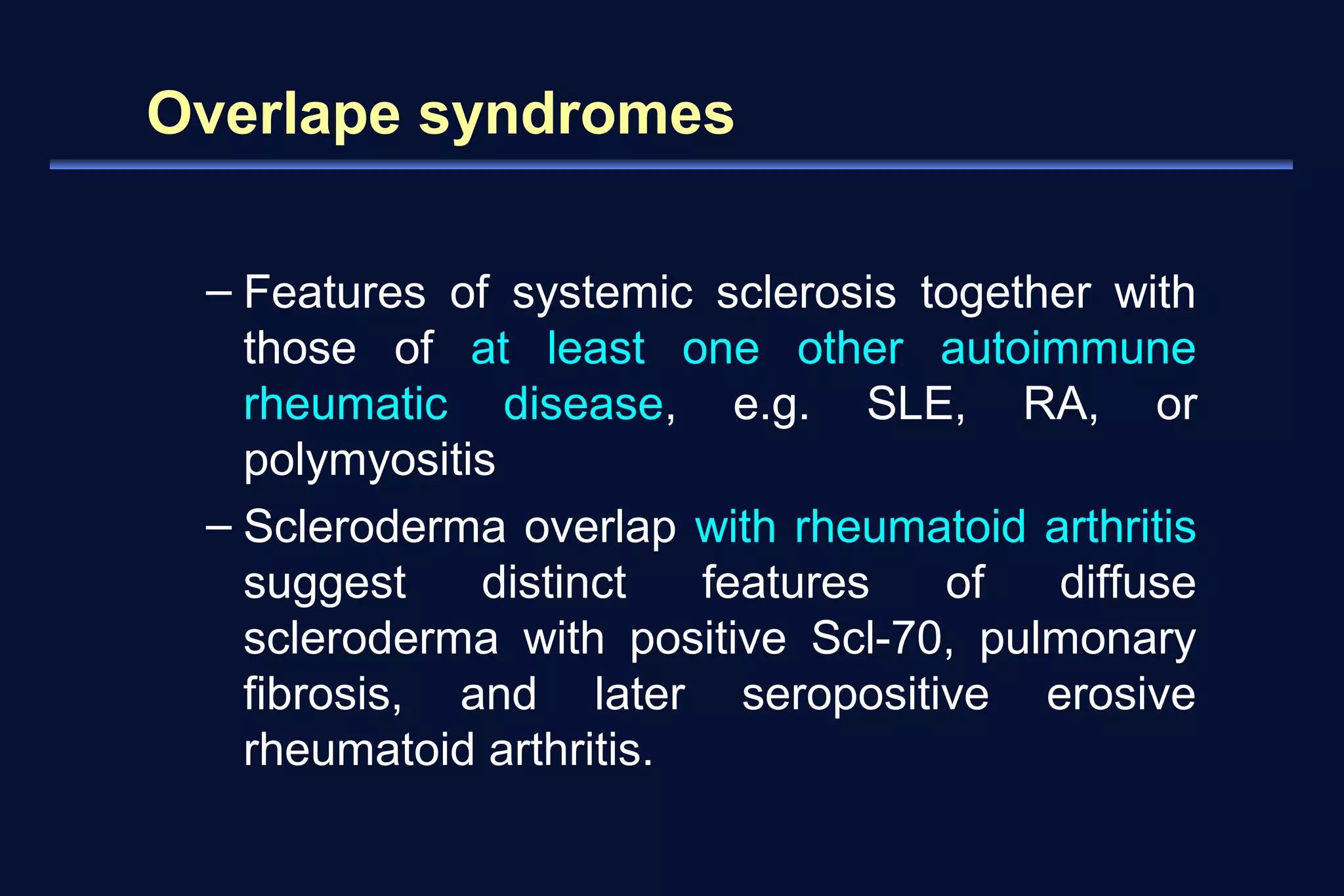
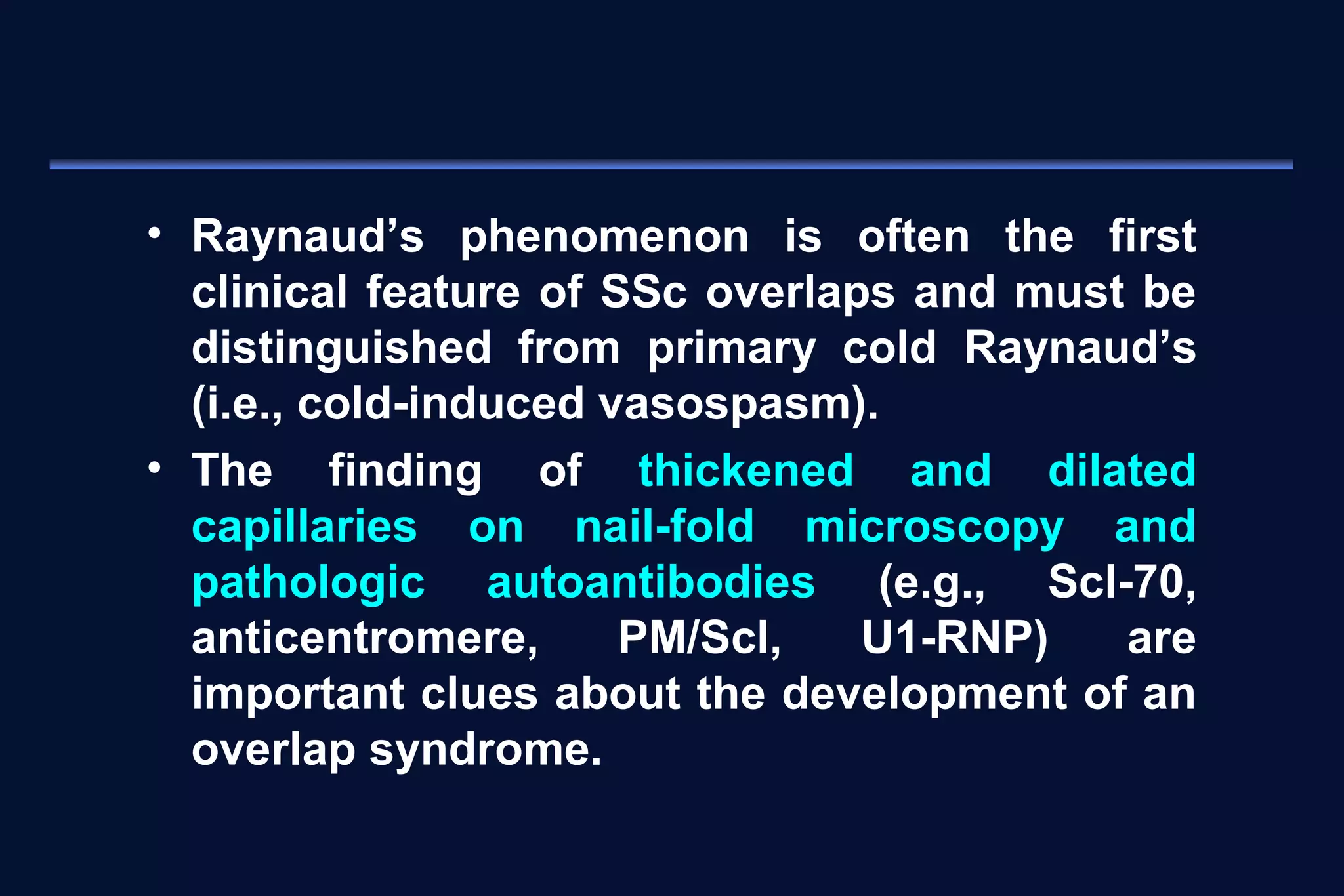
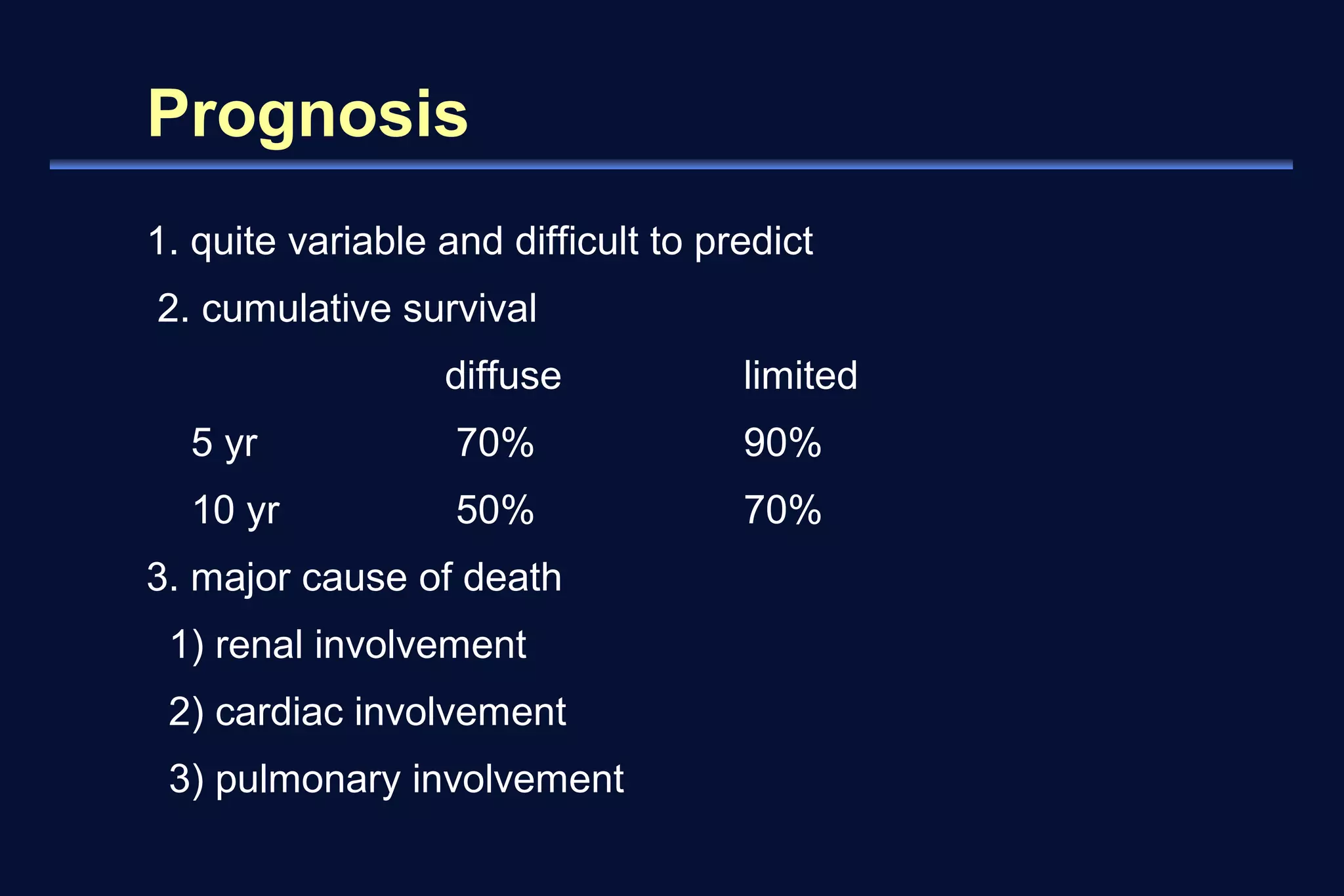
Systemic sclerosis, or scleroderma, is a multisystem disorder characterized by vascular abnormalities, skin and organ fibrosis, and immune system activation. It can be classified as either diffuse or limited cutaneous systemic sclerosis based on the extent and pattern of skin involvement. Common clinical features include Raynaud's phenomenon, skin thickening, gastrointestinal issues, lung fibrosis, and renal crisis. Treatment involves managing symptoms, with immunosuppressants sometimes used to modify disease progression. Prognosis depends on subtype, with limited scleroderma carrying a better long-term survival rate than diffuse disease.