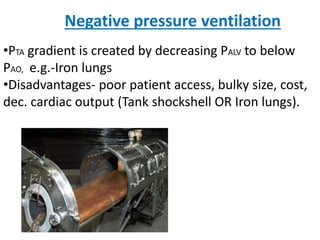
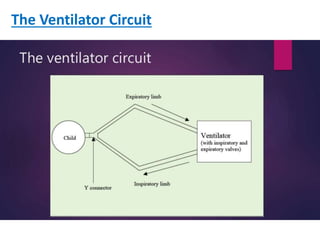
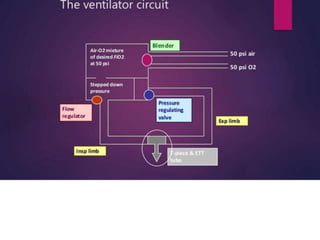
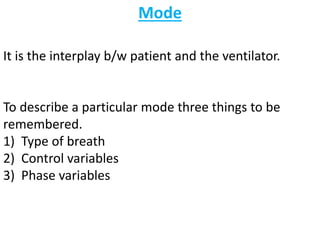
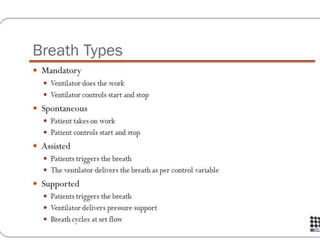
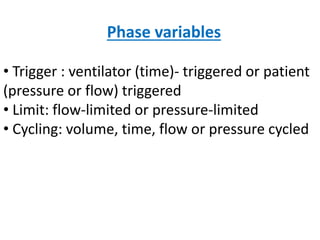
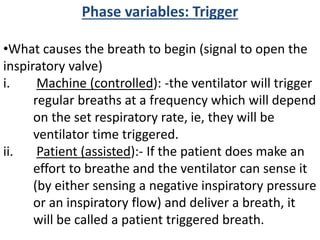
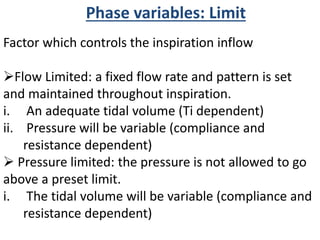
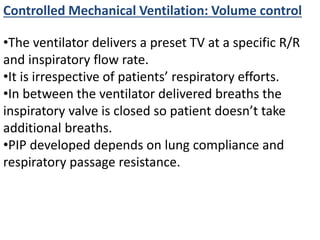
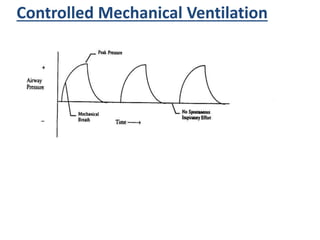
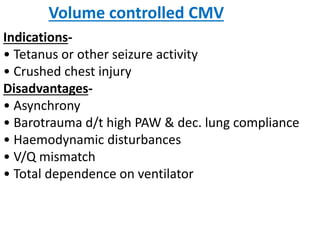
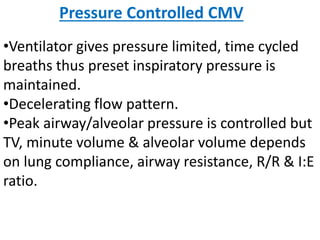
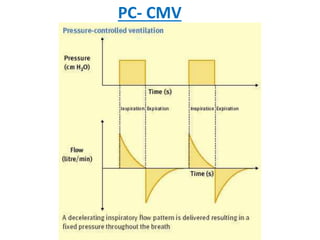
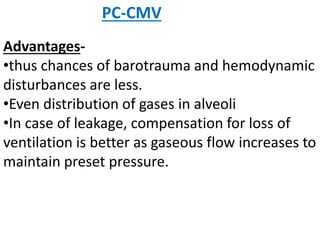
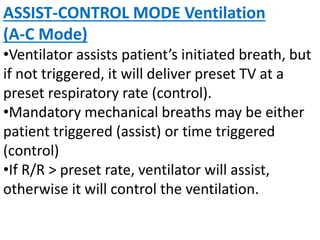
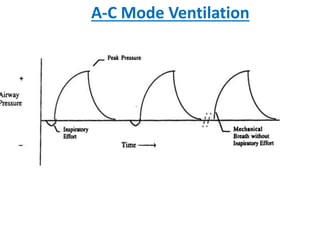
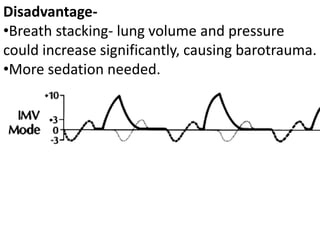
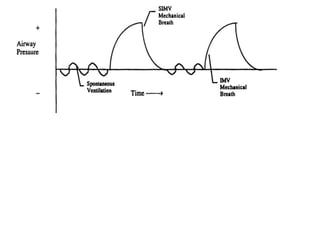
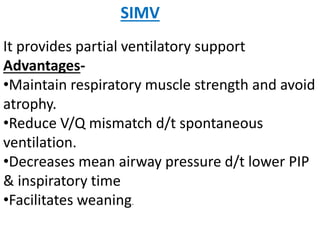
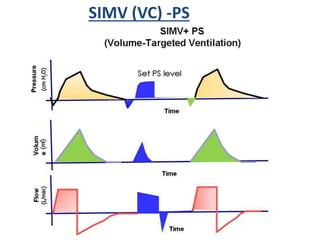
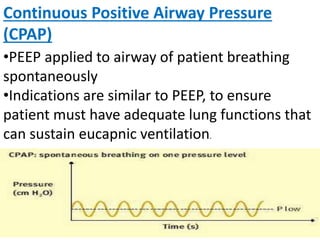
This document discusses different modes of mechanical ventilation. It begins by introducing mechanical ventilation and its purpose of providing respiratory support. It then describes the basic components of a ventilator and ventilator circuit. The document outlines several modes of mechanical ventilation including controlled mechanical ventilation, assist-control ventilation, intermittent mandatory ventilation, and synchronized intermittent mandatory ventilation. It provides details on the characteristics, advantages, and disadvantages of each mode.