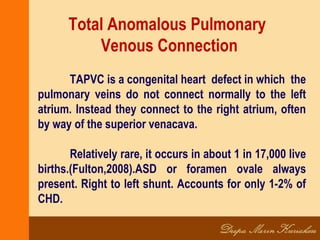
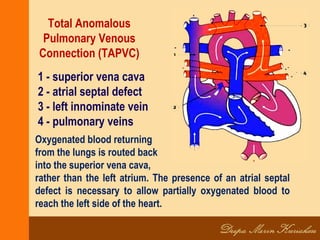
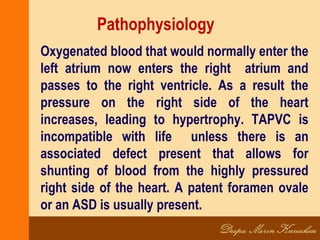
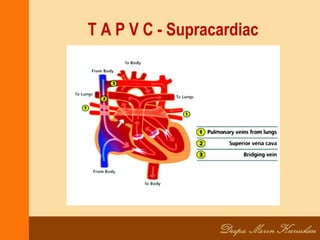
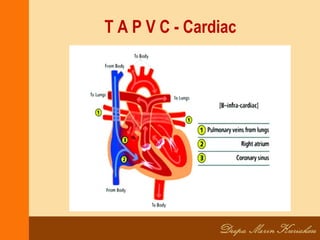
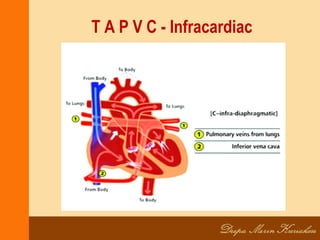
TAPVC is a congenital heart defect where the pulmonary veins do not connect normally to the left atrium, instead connecting to the right atrium, often via the superior vena cava. This causes oxygenated blood from the lungs to mix with deoxygenated blood. An ASD or PFO is always present to allow blood to reach the left side of the heart. Without treatment, TAPVC is fatal. Surgical repair is required to reconnect the pulmonary veins to the left atrium and close any defects. Post-surgery, patients require monitoring for complications, but long-term survival is generally good if repaired.