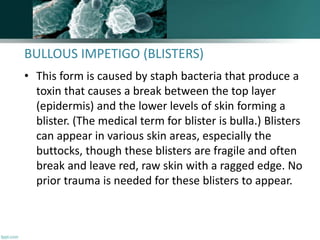
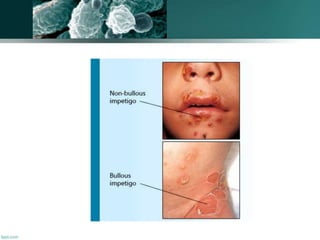
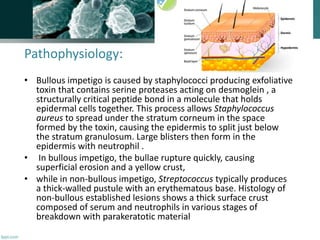
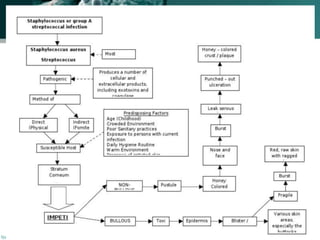
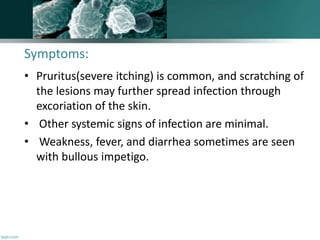
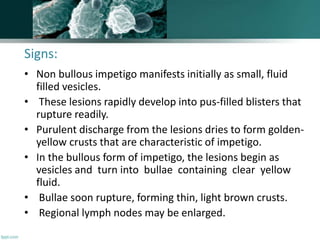
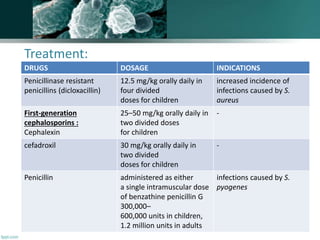
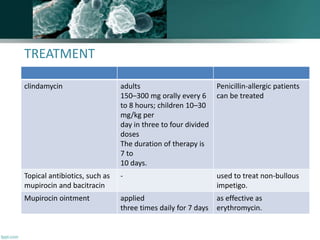
Impetigo is a highly contagious superficial skin infection primarily affecting children, caused by Staphylococcus aureus and Streptococcus pyogenes. It manifests as blisters, which can become crusted, and is common in warm, humid conditions, with significant prevalence in low-income areas, affecting over 162 million children globally. Treatment involves topical antibiotics like mupirocin for mild cases or oral antibiotics for more severe infections, with preventive measures emphasizing hygiene to avoid spreading the condition.