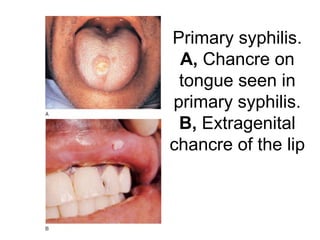
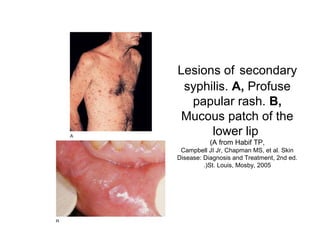
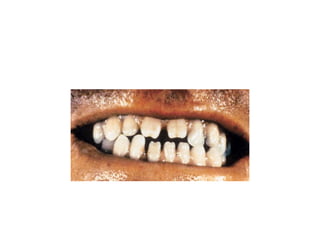
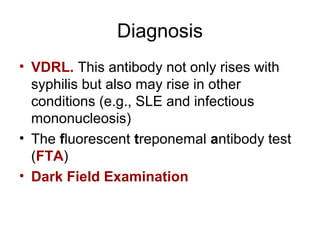
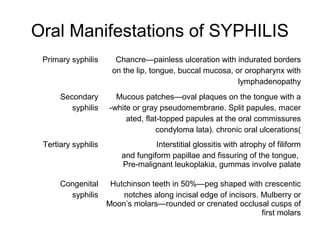
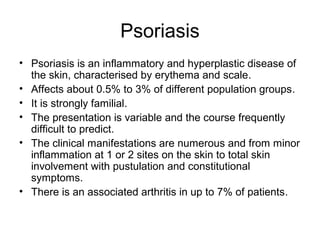
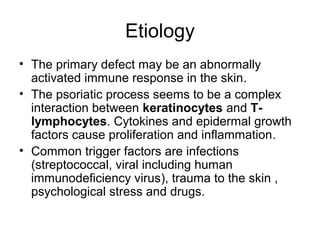
Syphilis is caused by the spirochete Treponema pallidum. It is transmitted through direct contact with lesions and has four stages: primary, secondary, latent, and tertiary. The primary lesion is a painless chancre. Secondary syphilis causes a rash and mucous patches. Latent syphilis is asymptomatic but infectious. Tertiary syphilis can cause damage to internal organs. Proper barrier techniques prevent transmission. Diagnosis involves serological tests and darkfield microscopy of lesions. Psoriasis is a chronic inflammatory skin condition affecting about 3% of the population. It has numerous clinical manifestations and is strongly familial. Treatment ranges from topical agents to systemic immunosup