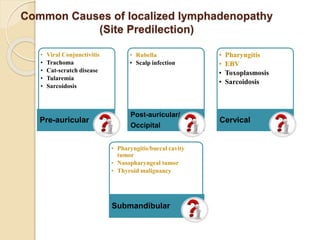
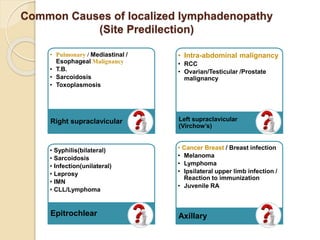
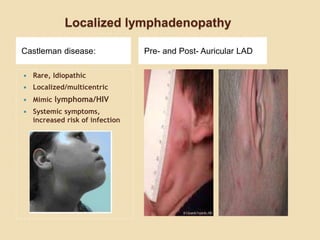
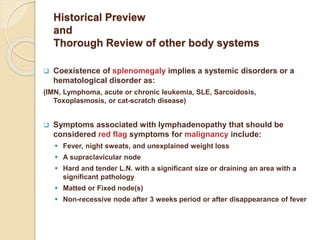
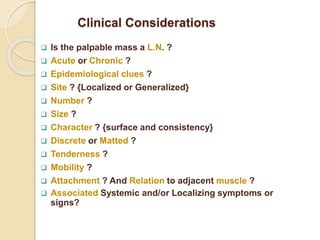
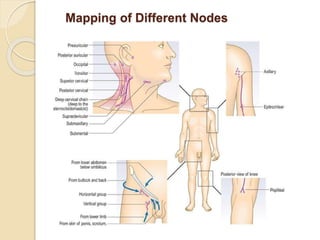
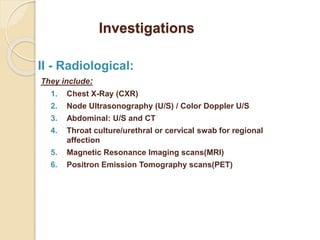
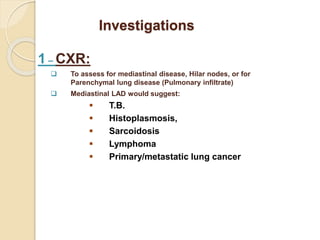
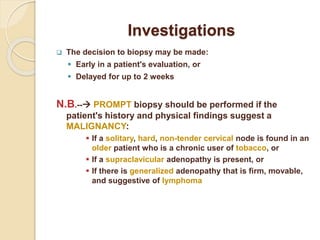
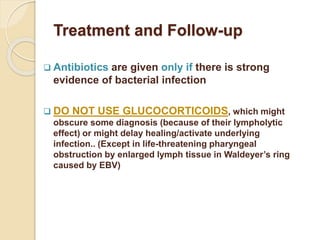
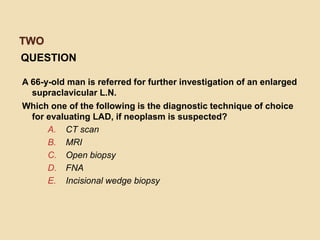
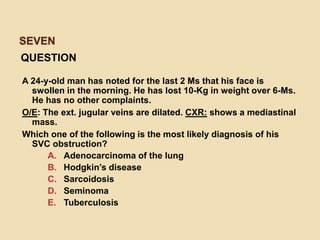
Lymphadenopathy refers to abnormal lymph nodes in size, number, or consistency. It can be generalized, involving two or more non-contiguous lymph node groups, or localized to a single group. Common causes include infections, cancers, autoimmune diseases, and medications. A thorough history and physical exam are important to evaluate potential causes and symptoms. Red flags suggesting possible malignancy include supraclavicular adenopathy, hard/tender nodes, matted nodes, and nodes that do not regress after 3 weeks or fever resolution. Careful assessment of lymphadenopathy guides further diagnostic workup and management.