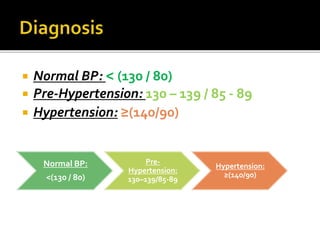
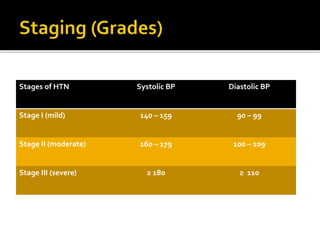
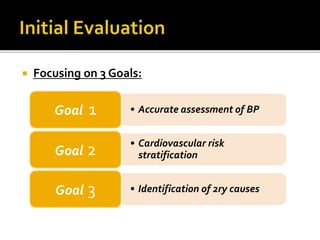
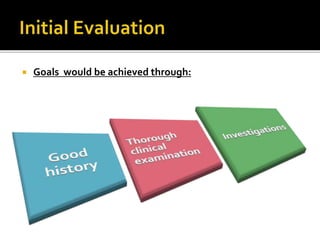
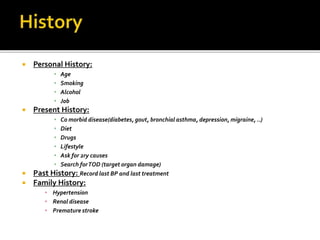
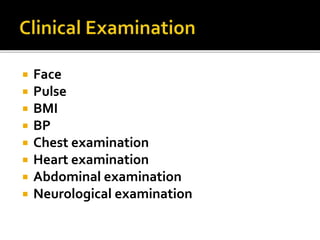
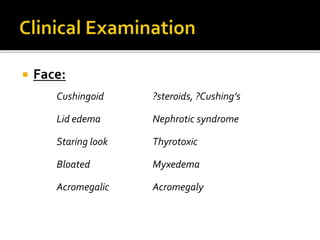
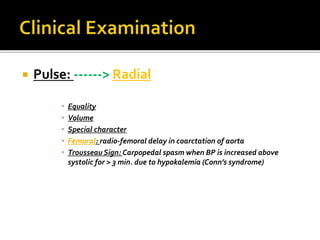
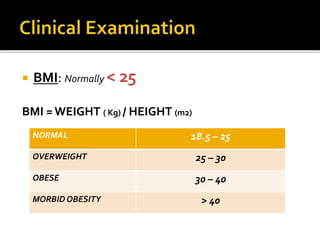
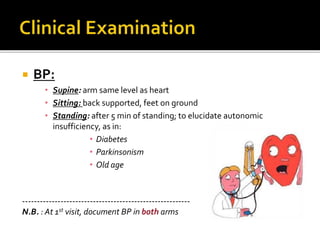
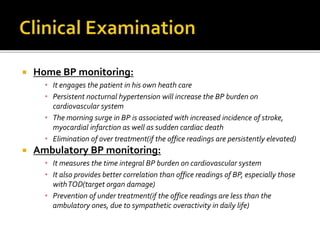
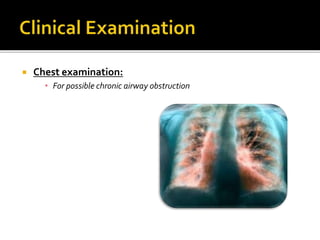
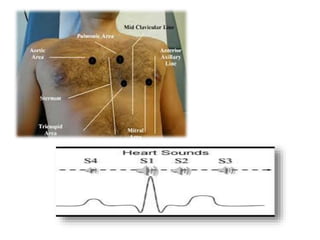
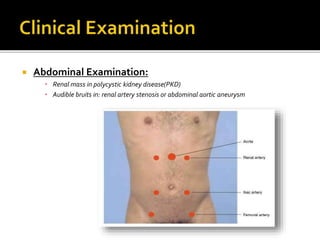
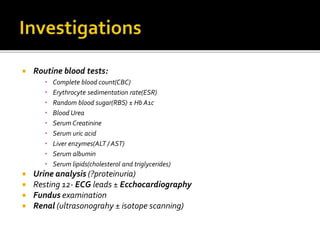
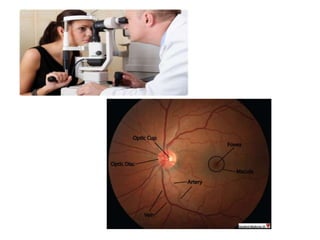
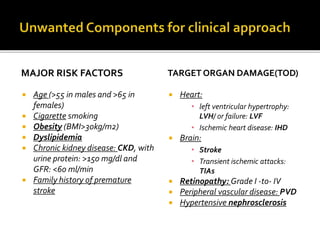
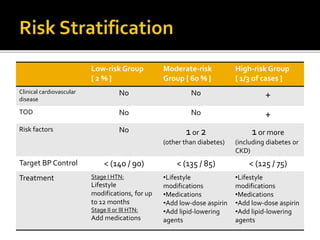
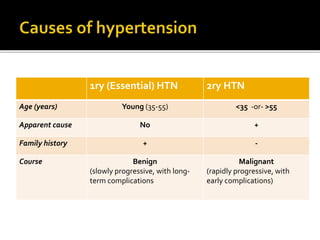
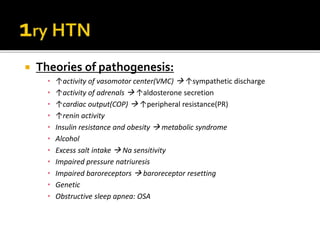
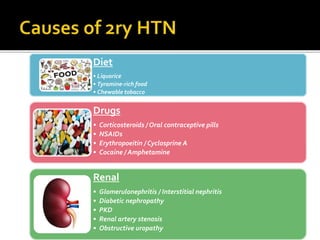
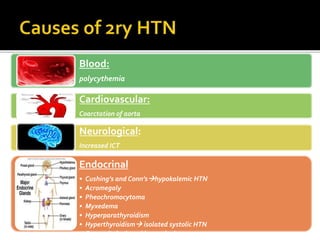
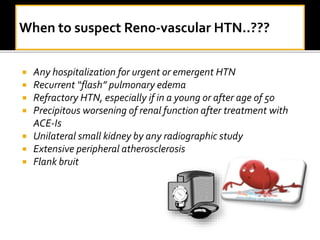
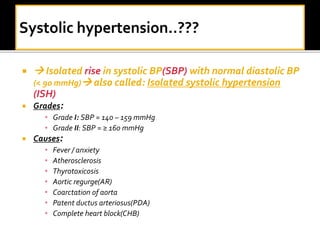
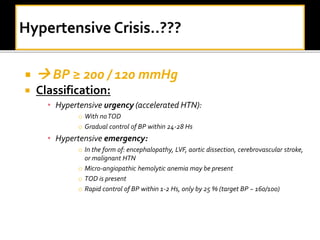
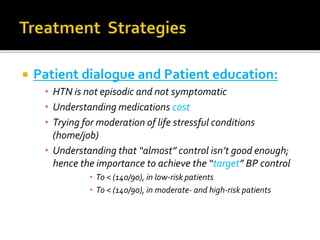
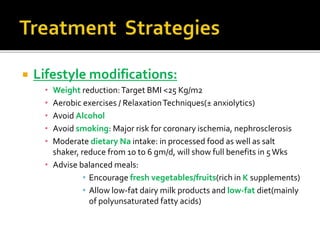
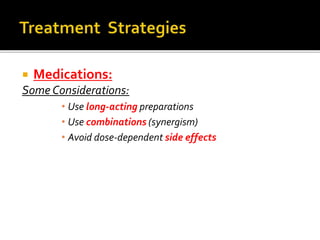
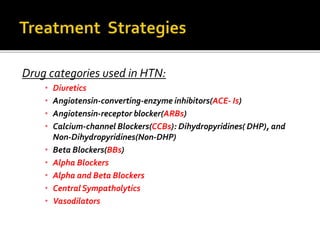
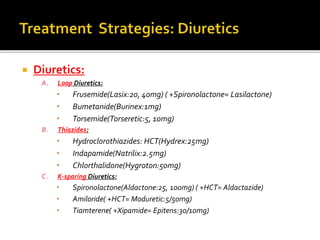
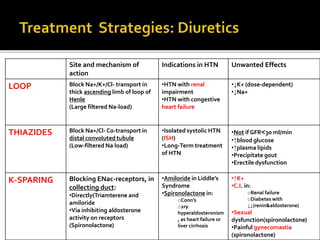
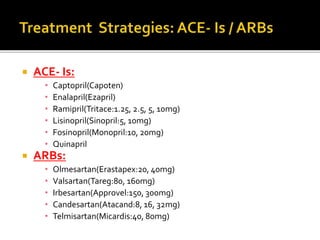
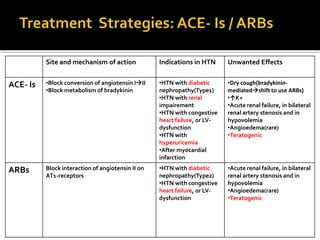
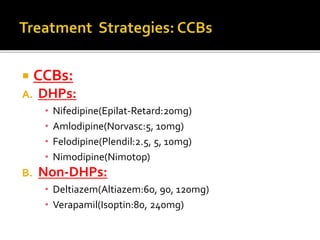
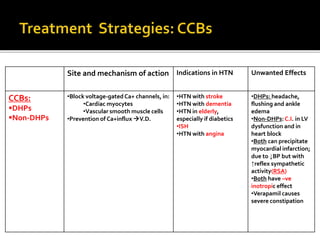
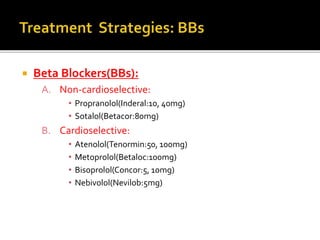
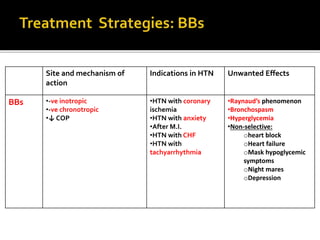
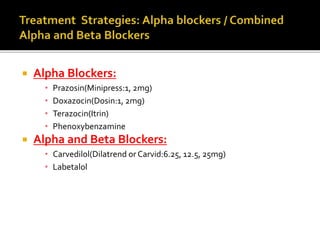
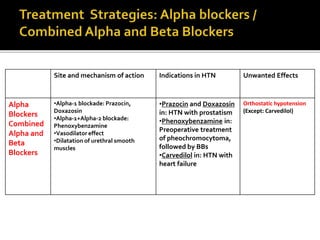
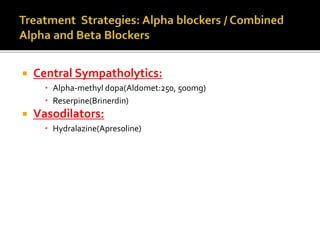
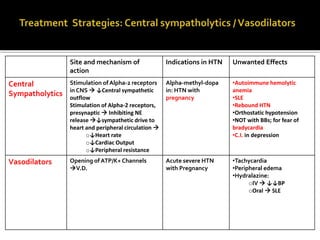
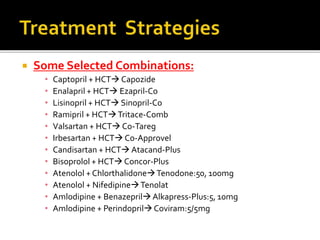
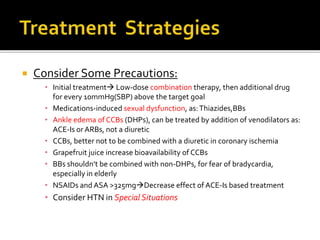
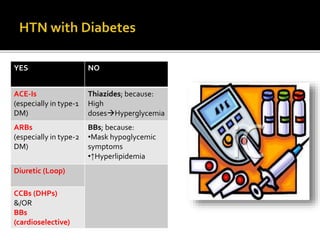
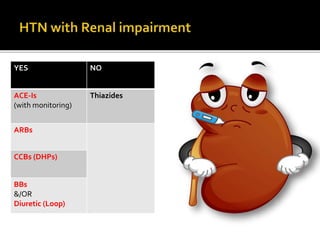
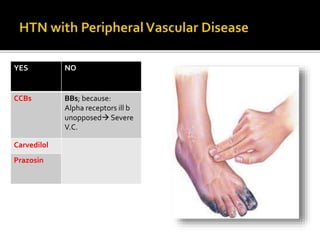
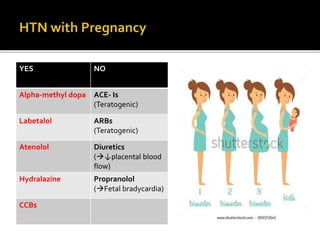
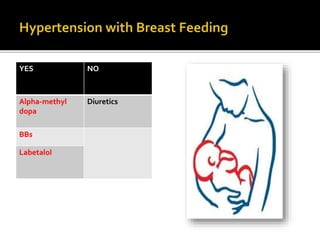
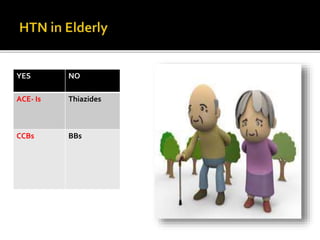
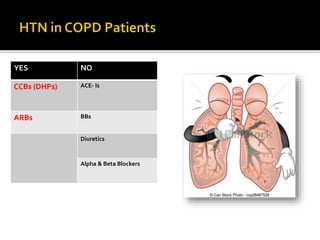
This document outlines the classification and management of hypertension (HTN), including definitions, stages, and treatment protocols. It emphasizes the importance of accurate blood pressure assessment, risk stratification, and identifying secondary causes, while also detailing lifestyle modifications and medication options for treatment. The document serves as a comprehensive guide for healthcare professionals in managing patients with high blood pressure.