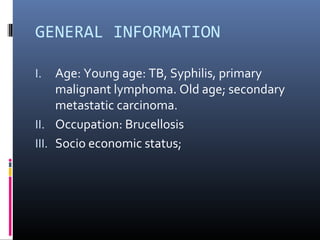
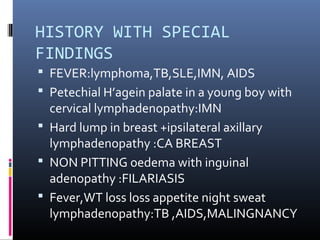
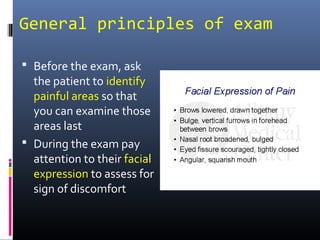
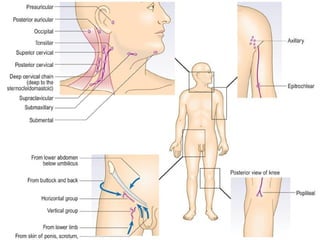
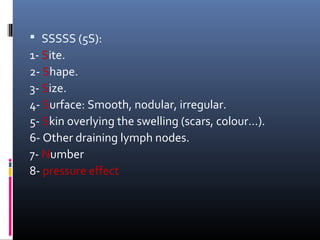
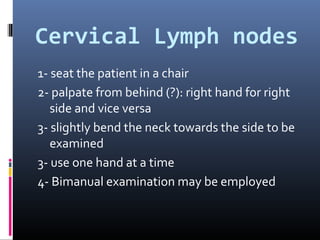
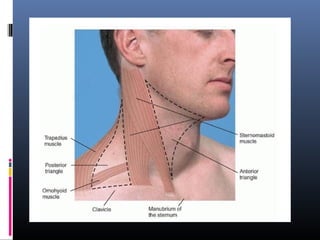
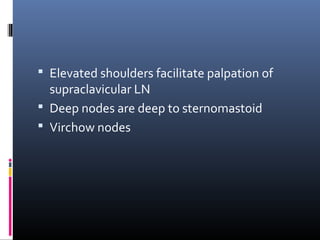
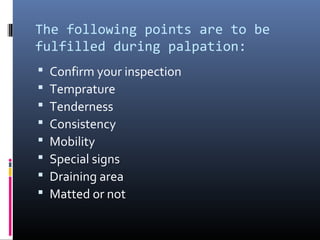
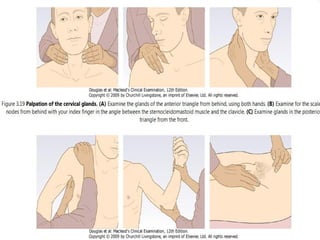
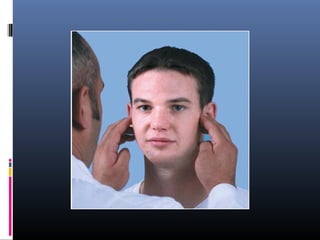
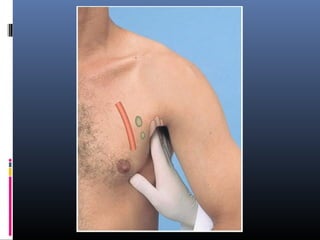
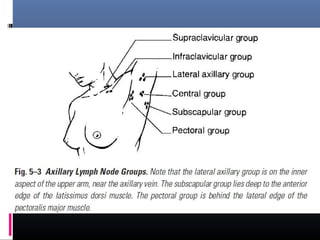
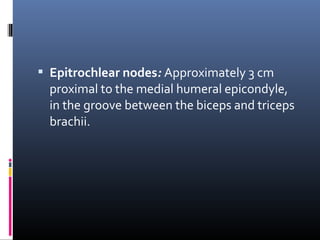
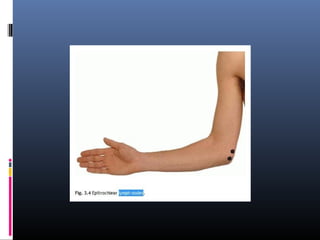
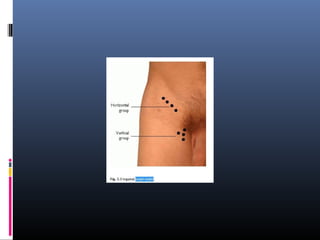
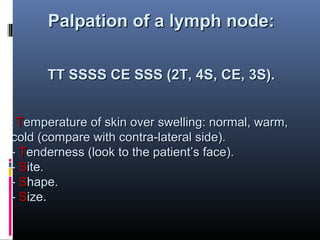
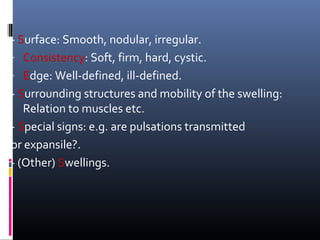
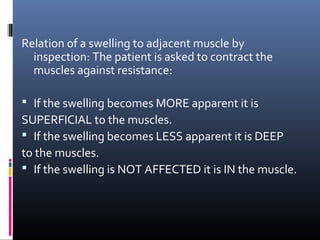
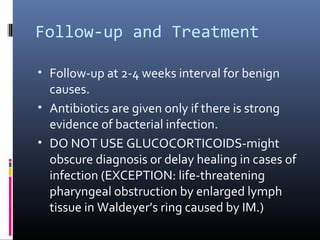
Lymphadenopathy refers to the enlargement of lymph nodes. This document provides information on evaluating lymphadenopathy through medical history, physical examination, and potential diagnostic tests and procedures. The medical history focuses on symptoms, risk factors, exposures, and family history that could indicate the cause. The physical examination describes palpating lymph nodes in the cervical, axillary, inguinal, and other areas to assess characteristics like size, shape, texture, and tenderness. Potential causes of lymphadenopathy include infections, inflammatory conditions, and cancers. Follow-up may involve repeated examinations or diagnostic tests and procedures like biopsy to identify benign versus malignant causes.