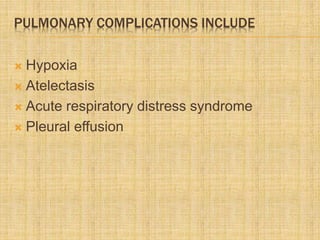
- Pulmonary complications are common in acute pancreatitis and include hypoxia, atelectasis, ARDS, and pleural effusions.
- Inflammatory mediators released during pancreatitis like trypsin, phospholipase A2, and TNF-α can damage the lungs and impair oxygenation.
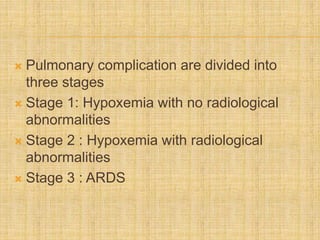
- Pulmonary complications occur in three stages - stage 1 involves hypoxia with no radiological abnormalities, stage 2 adds radiological findings like pleural effusions or infiltrates, and stage 3 is ARDS which has a high mortality rate. Aggressive management of oxygenation and underlying pancreatitis is important.