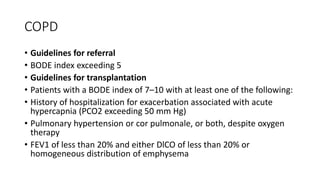
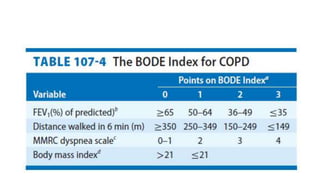
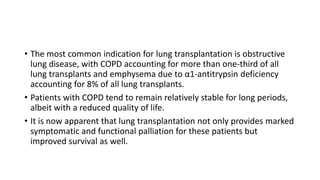
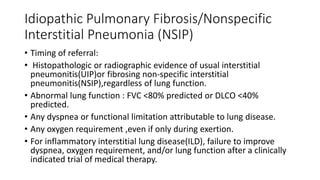
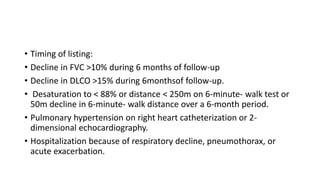
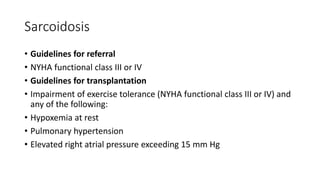
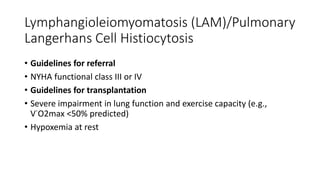
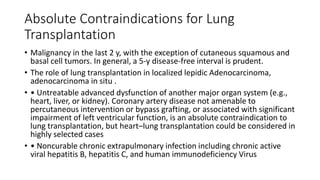
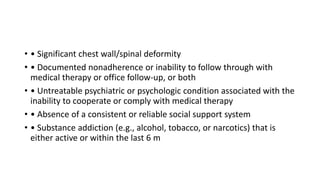
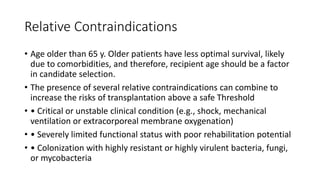
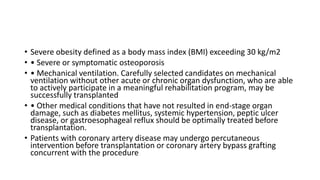
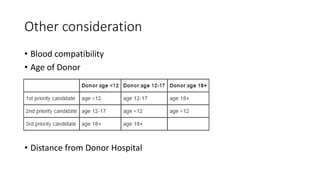
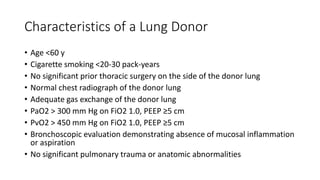
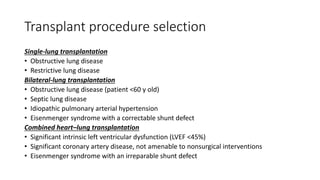
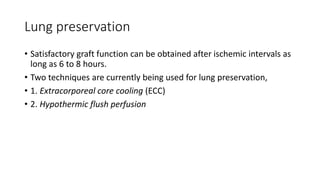
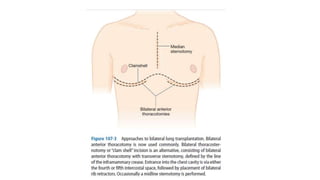
This document discusses lung transplantation, including indications, contraindications, recipient selection, donor selection, and surgical considerations. The most common indications for lung transplantation are COPD, idiopathic pulmonary fibrosis, cystic fibrosis/bronchiectasis, and PAH. Absolute contraindications include recent malignancy or uncontrolled infection/disease. Recipient selection involves evaluating cardiopulmonary function and psychosocial status. Donor lungs should be from donors under age 60 with less than 20-30 pack-years smoking history and adequate gas exchange.