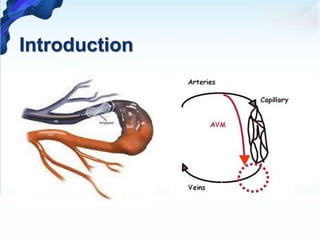
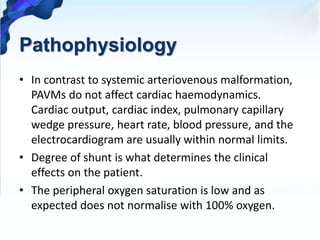
1. Pulmonary arteriovenous malformations (PAVMs) are rare vascular anomalies where abnormal dilated vessels provide a right-to-left shunt between the pulmonary artery and vein.
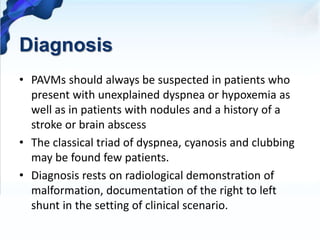
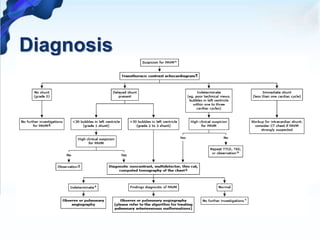
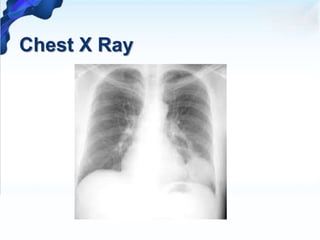
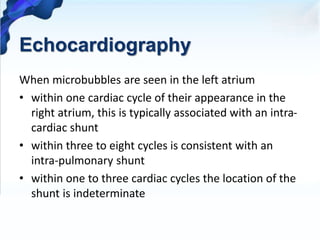
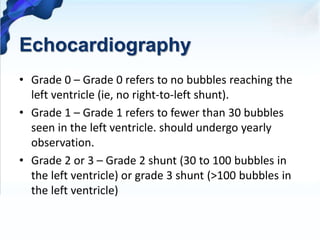
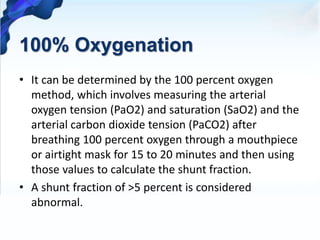
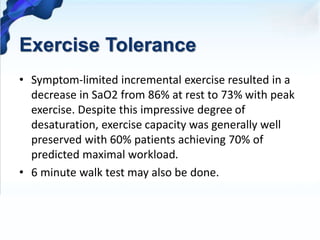
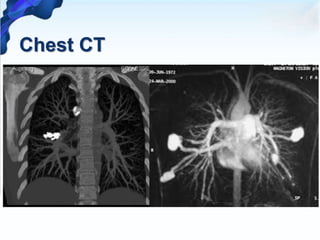
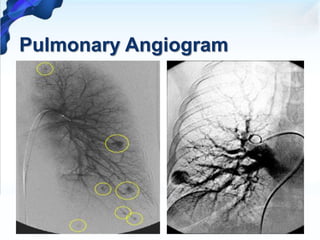
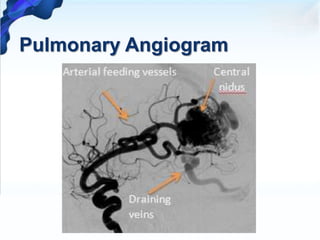
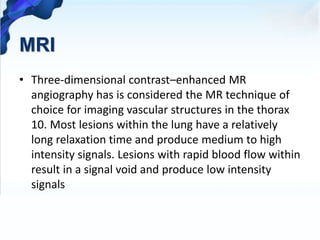
2. PAVMs are usually diagnosed through imaging like chest X-ray, CT, or MRI which show dilated vessels. Right-to-left shunting can be detected using echocardiography, oxygen studies, or pulmonary angiography.
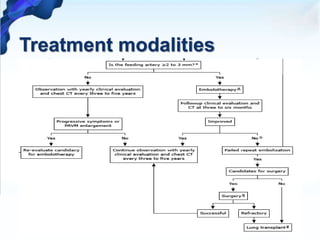
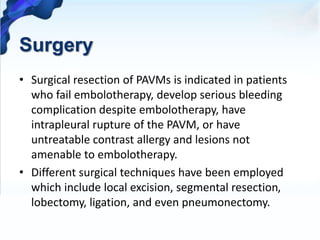
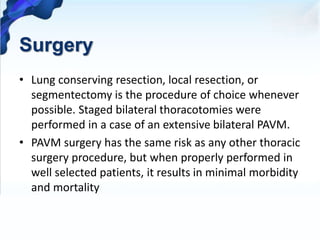
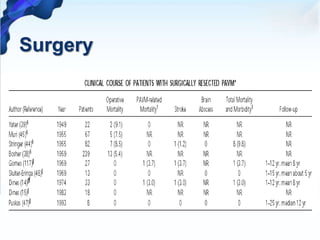
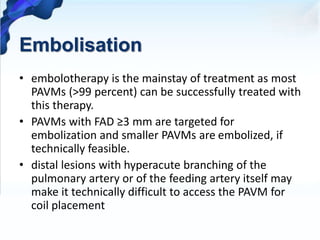
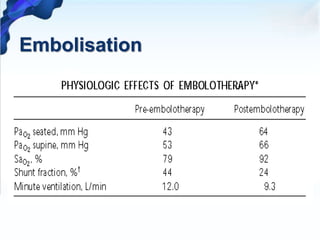
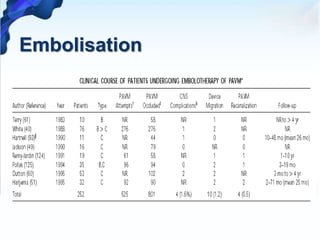
3. Treatment involves embolization to occlude the abnormal vessels which successfully treats over 99% of PAVMs. Surgery is an alternative for cases that cannot be embolized or if embolization fails.