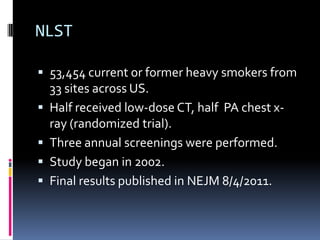
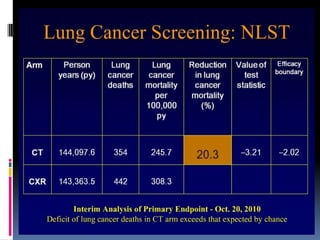
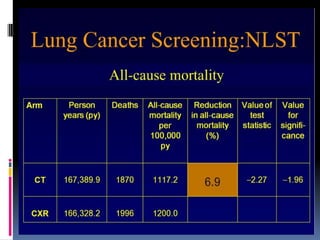
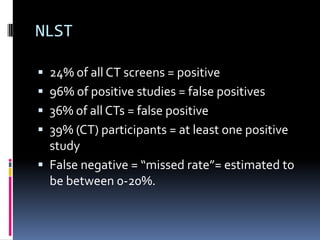
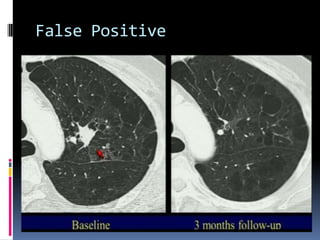
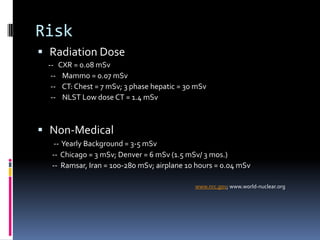
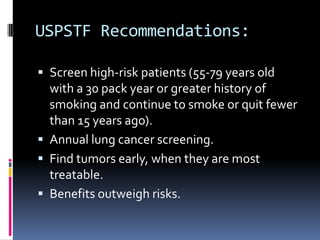
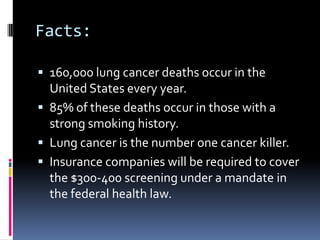
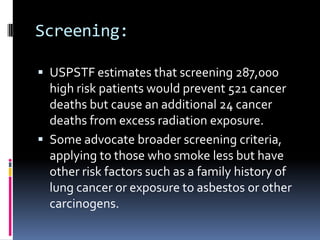
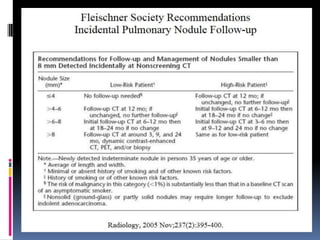
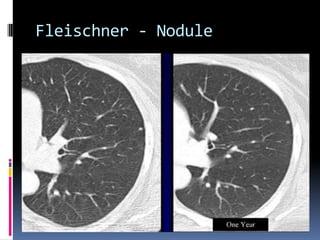
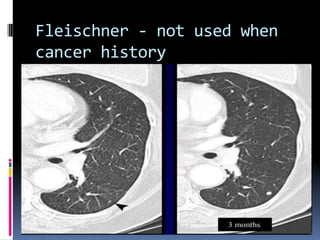
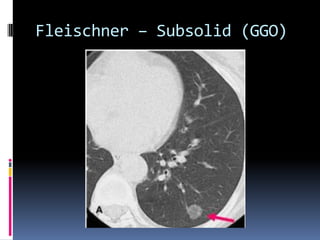
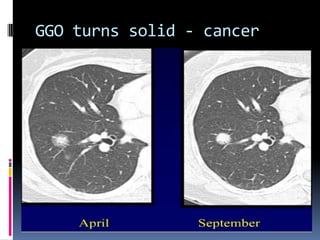
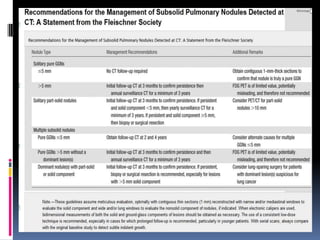
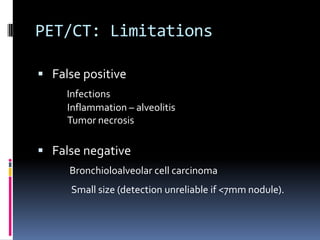
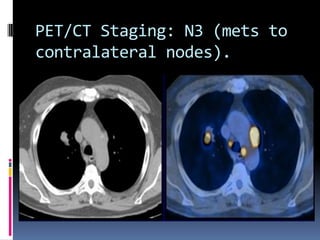
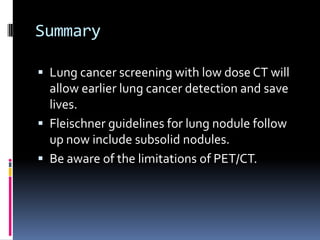
The document reviews current topics in lung cancer imaging, including updates on lung cancer screening, management of small lung nodules, and the limitations of PET/CT for staging. It emphasizes the importance of low-dose CT screening for high-risk patients, the statistics from the NLST study, and the necessity for insurance coverage for screenings. Additionally, it discusses the challenges of overdiagnosis and radiation exposure while outlining the Fleischner guidelines for follow-up care of lung nodules.