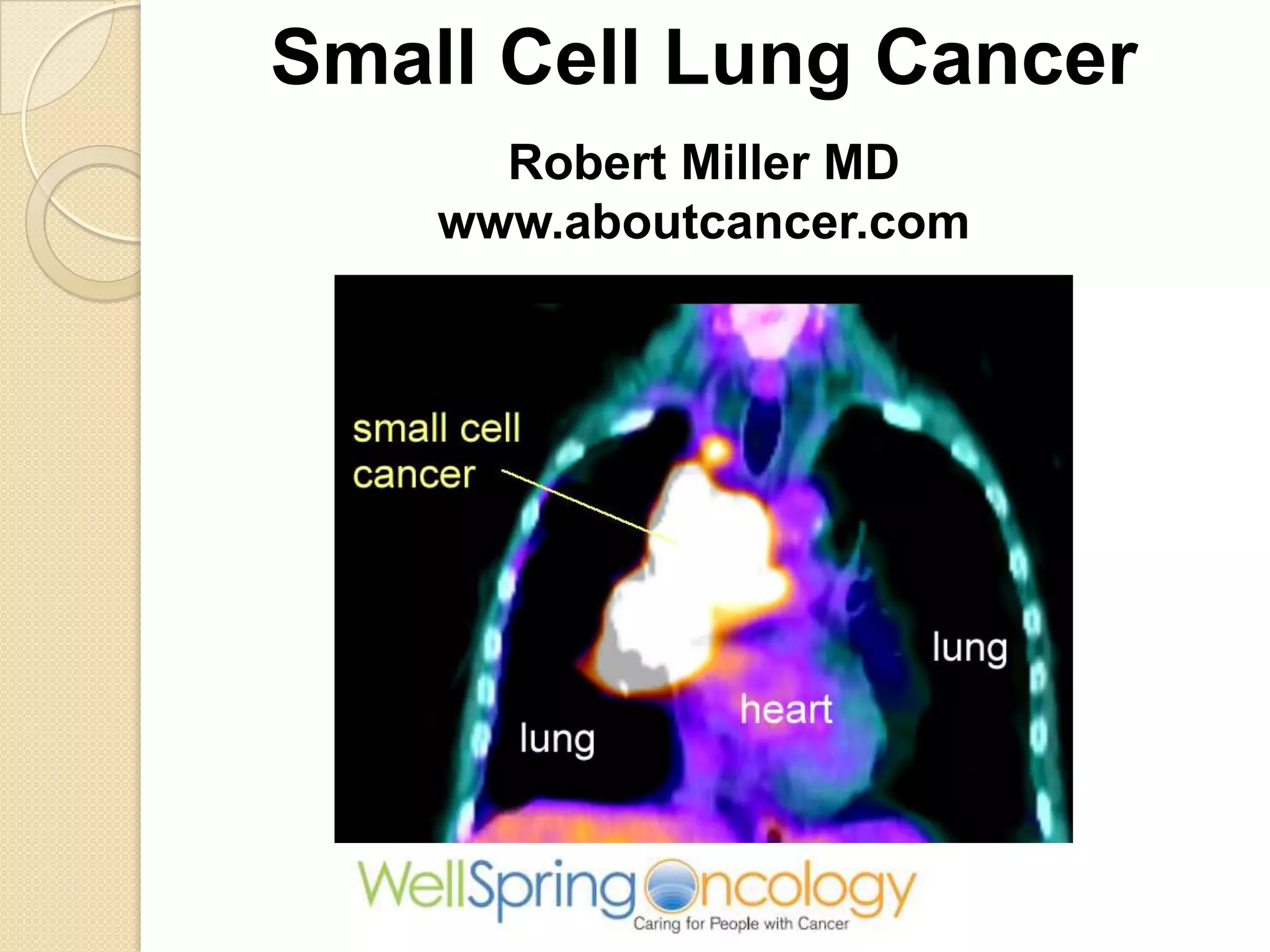
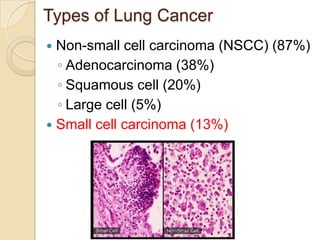
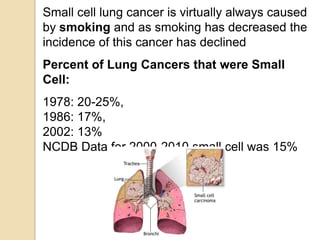
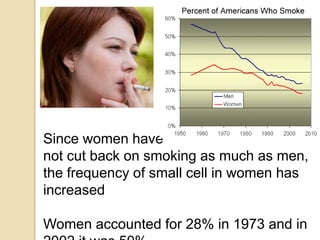
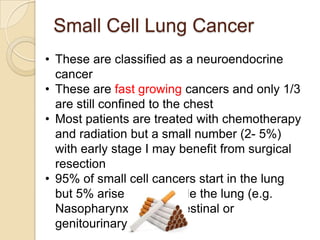
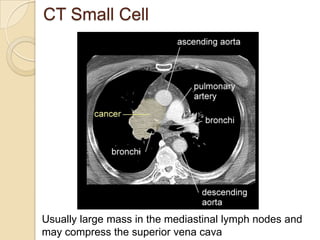
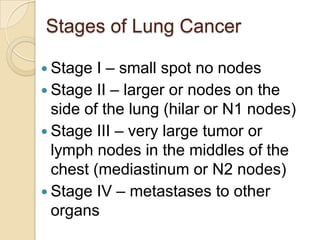
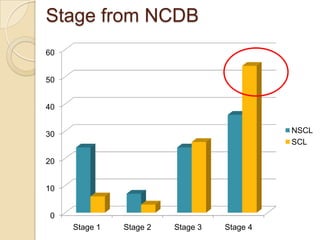
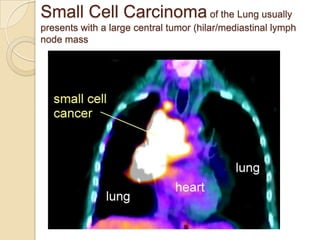
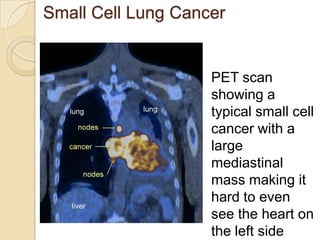
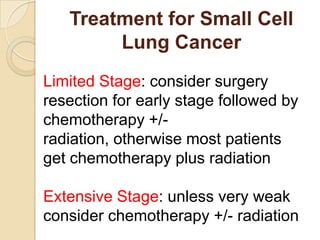
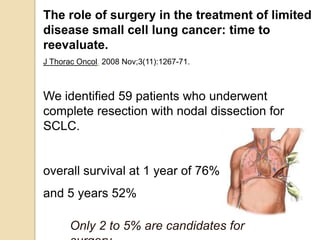
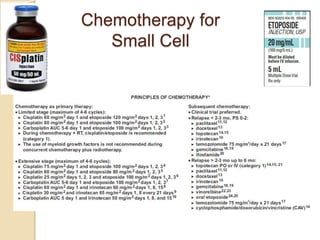
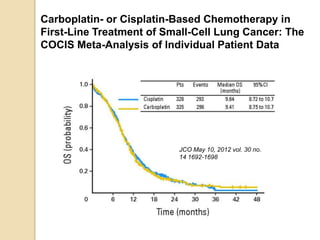
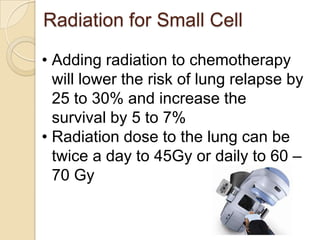
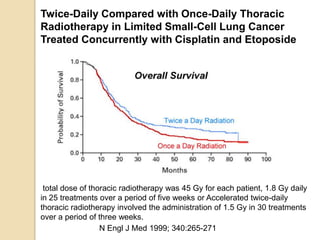
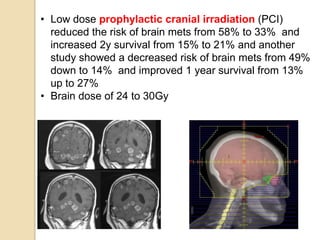
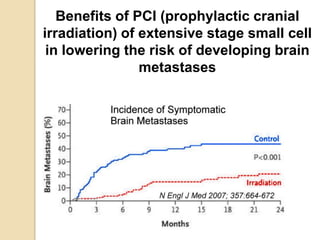
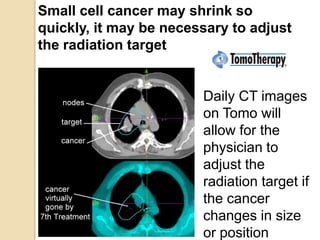
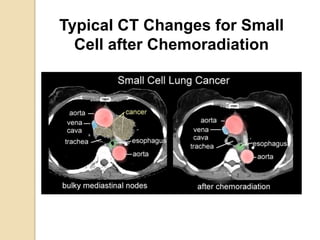
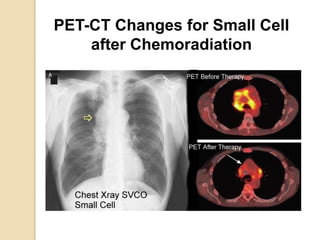
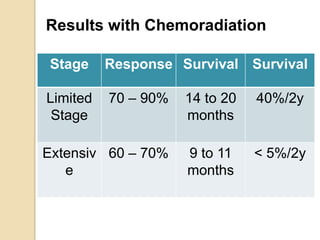
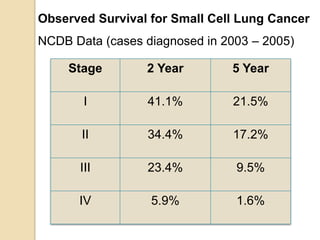
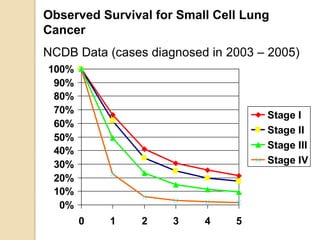
Small cell lung cancer (SCLC) accounts for 13% of lung cancers and is strongly linked to smoking. SCLC typically presents as a large mass in the mediastinal lymph nodes. It is classified as limited stage, confined to one lung, or extensive stage with distant metastases. Treatment involves chemotherapy with cisplatin and etoposide, and sometimes radiation therapy. For limited stage SCLC, surgery may be an option for early tumors. While initial response rates are high, most patients experience relapse. Prophylactic cranial irradiation can reduce the risk of brain metastases. Even with optimal treatment, the 5-year survival rate remains low at 5-10% for extensive stage and 30-40% for limited stage disease