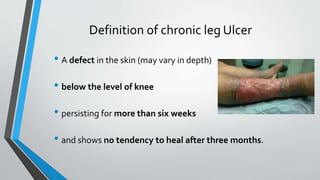
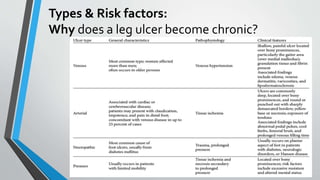
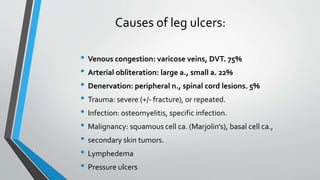
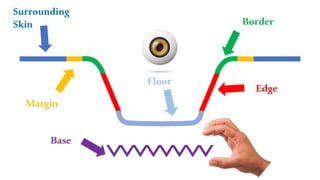
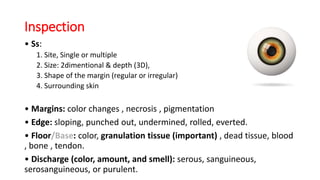
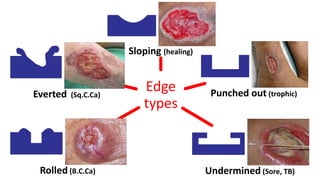
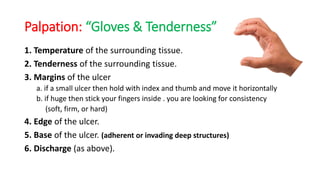
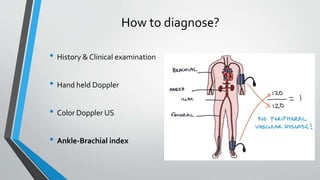
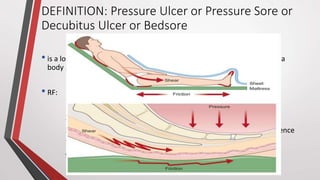
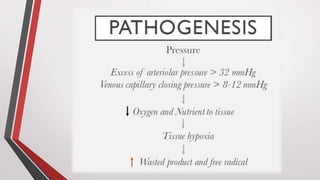
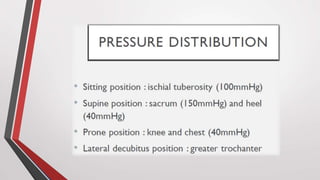
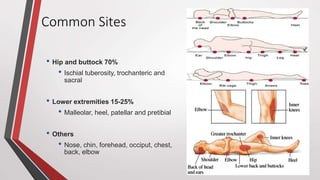
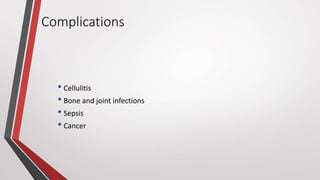
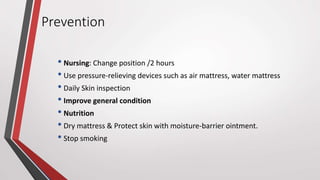
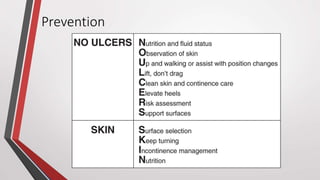
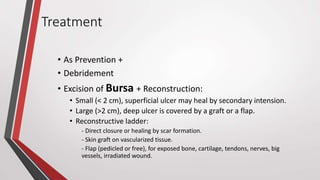
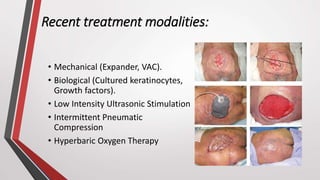
The document provides a comprehensive overview of chronic leg ulcers and pressure sores, detailing their definitions, causes, types, and risk factors. It emphasizes the importance of proper diagnosis, management, and treatment strategies including dressing, debridement, and surgical options. Additionally, it discusses the prevention of pressure sores through nursing interventions and recent treatment modalities.