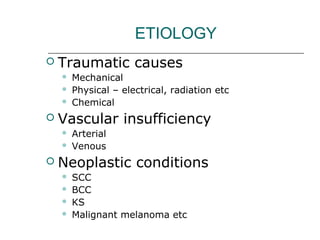
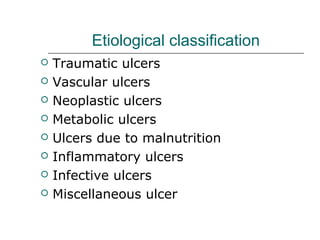
The document discusses various types of ulcers, detailing their definitions, etiologies, classifications, pathophysiology, clinical presentations, workup, and treatments. It categorizes ulcers based on causes including traumatic, vascular, neoplastic, metabolic, and infective factors, and outlines three phases of ulcer development: extension, transition, and repair. Additionally, it emphasizes both conservative and surgical treatment approaches tailored to the underlying causes of the ulcers.