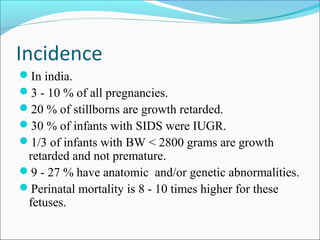
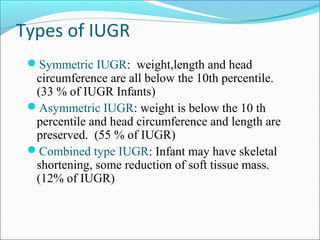
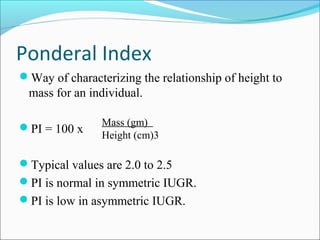
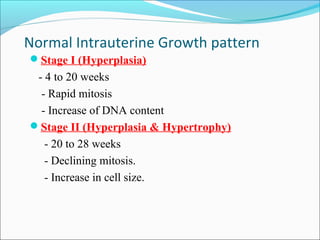
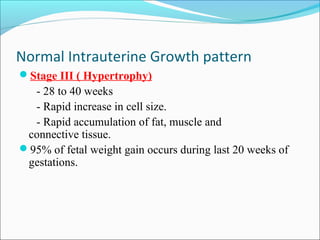
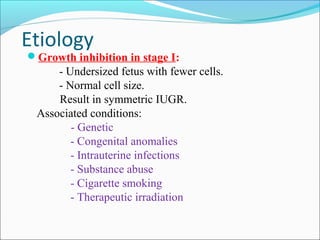
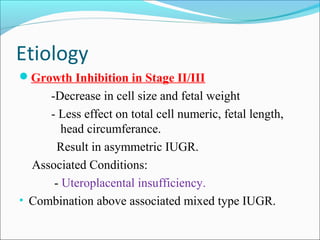
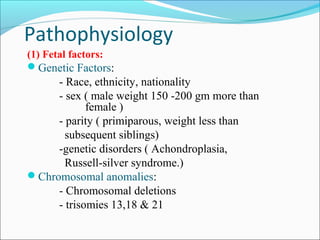
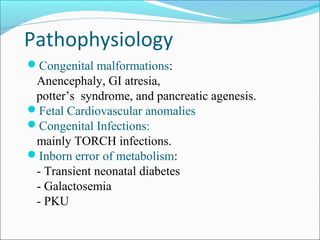
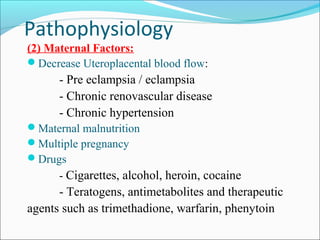
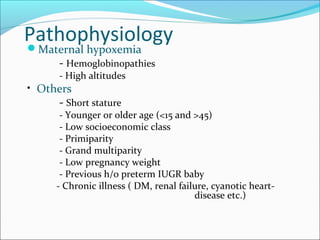
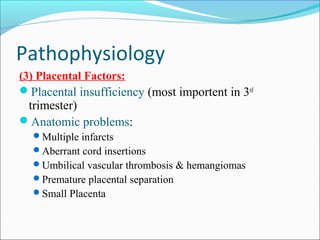
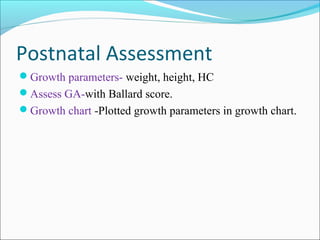
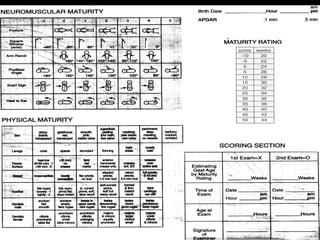
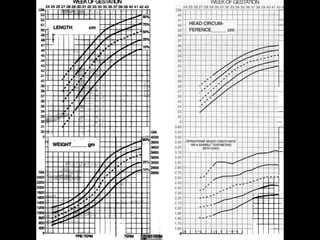
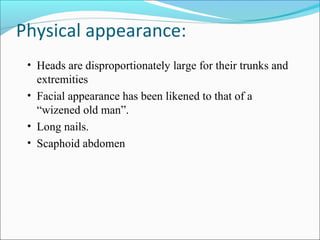
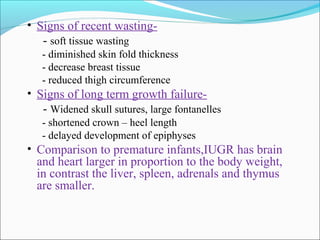
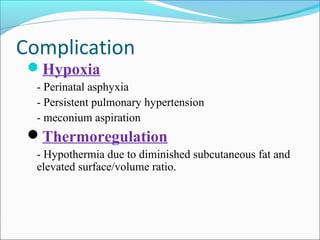
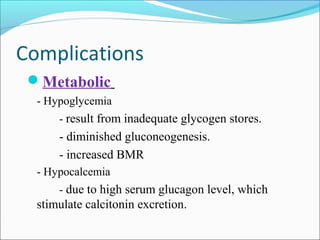
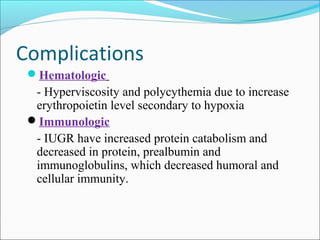
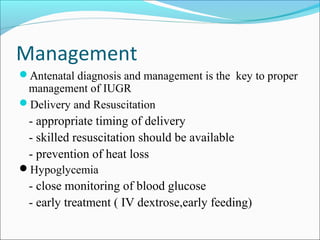
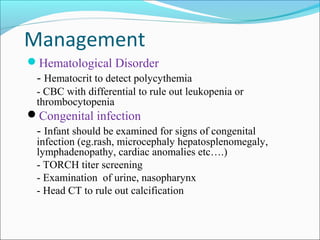
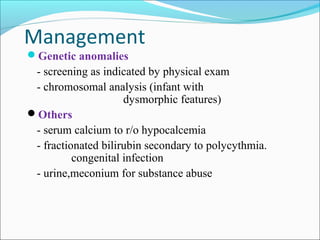
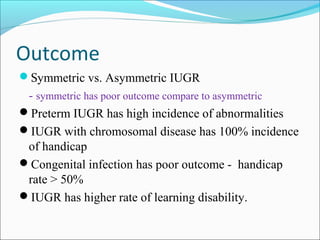
This document discusses intrauterine growth restriction (IUGR) and small for gestational age (SGA) infants. It defines IUGR as impaired fetal growth and SGA as weight below the 10th percentile. IUGR incidence in India is 3-10% of pregnancies and is associated with higher stillbirth and infant mortality rates. IUGR can be symmetric, asymmetric, or combined based on effects on weight, length, and head circumference. Etiologies include placental insufficiency, genetic factors, infections, and maternal health conditions. Complications include hypoglycemia, hypothermia, and immune dysfunction. Proper management involves antenatal diagnosis, skilled delivery and resuscitation, glucose monitoring, screening for