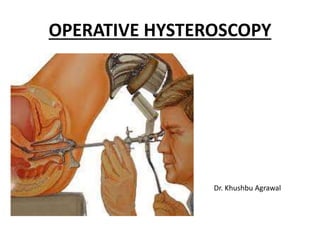
This document provides information on operative hysteroscopy, including therapeutic indications, instruments used, specific procedures, complications, and techniques. Some key points:
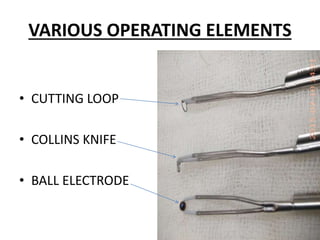
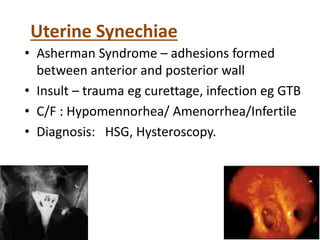
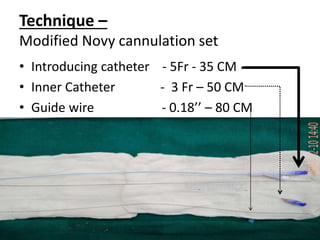
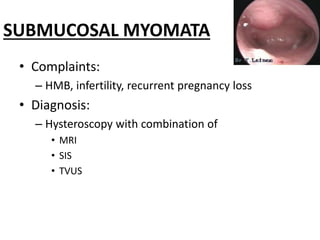
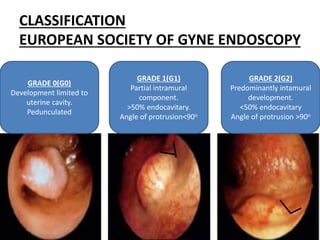
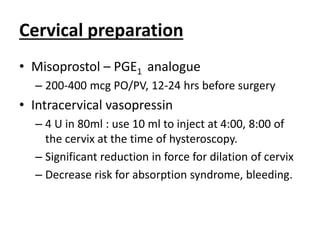
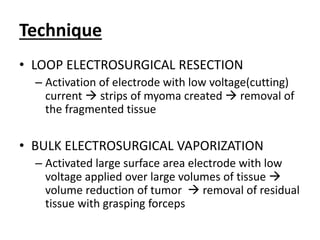
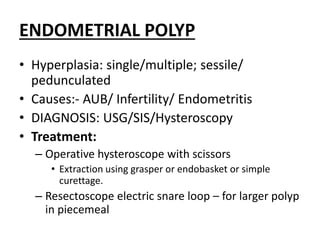
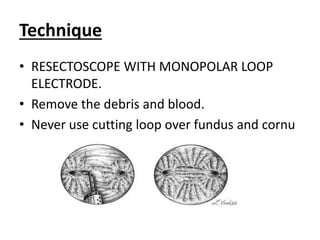
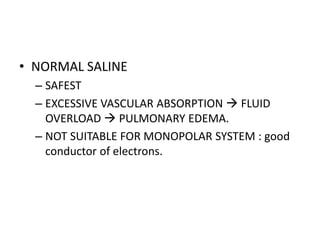
- Operative hysteroscopy is used to treat conditions like uterine septum, synechiae, polyps, and myomas. Instruments include a resectoscope, cutting loops, and electrodes.
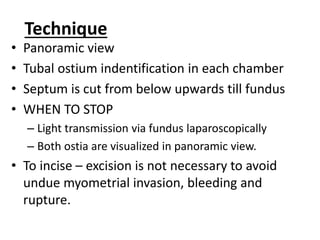
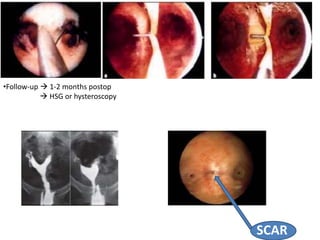
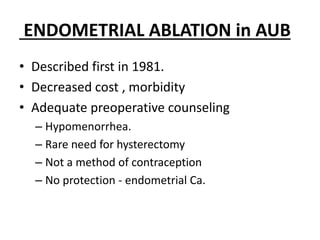
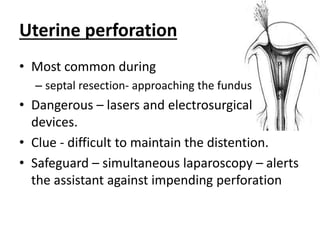
- Specific procedures discussed include hysteroscopic metroplasty for septate uterus, adhesiolysis for synechiae, transcervical resection of submucous myomas, and endometrial ablation.
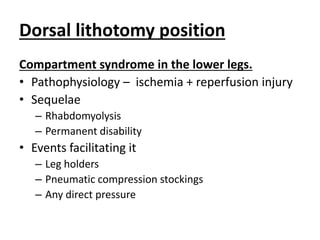
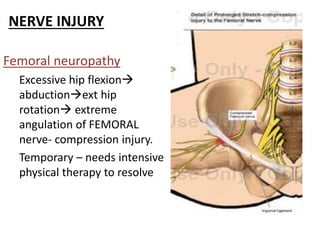
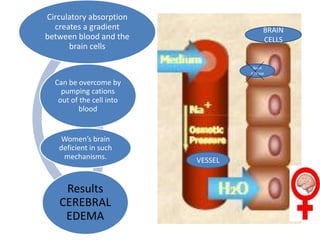
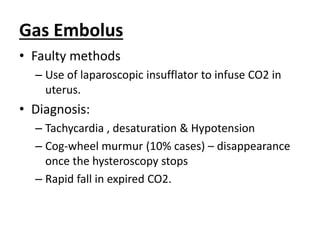
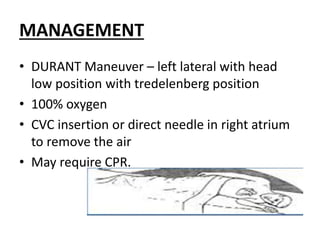
- Complications can be perioperative like bleeding, perforation, or fluid absorption syndrome, or postoperative like adhesions or