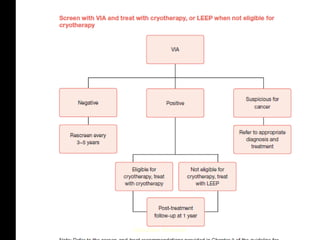
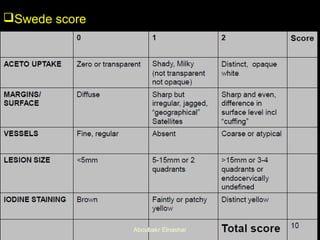
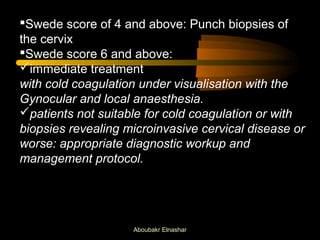
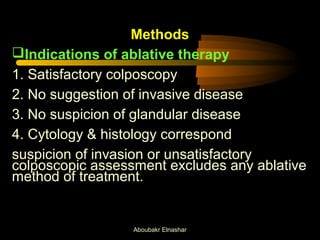
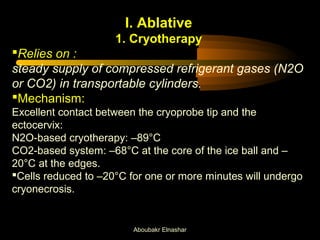
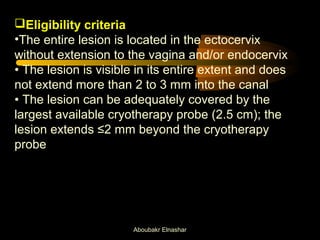
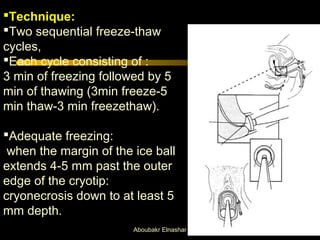
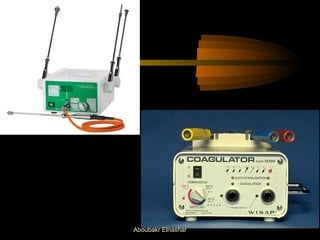
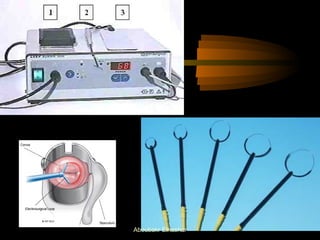
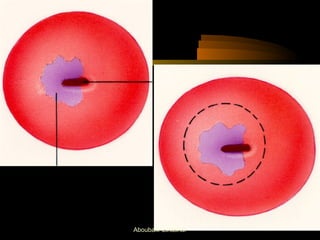
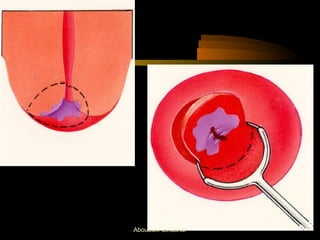
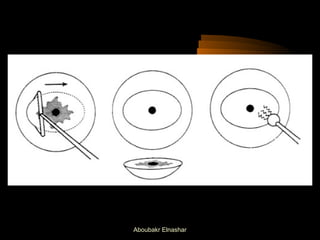
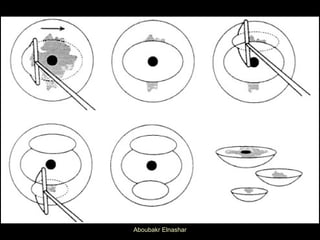
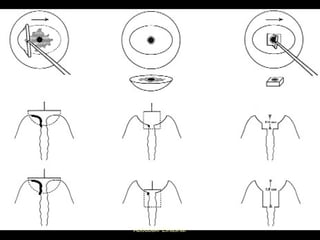
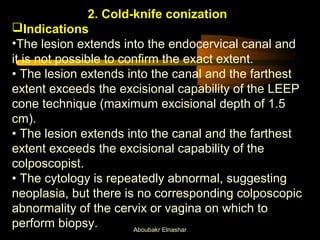
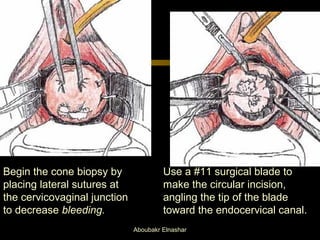
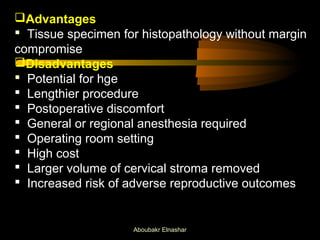
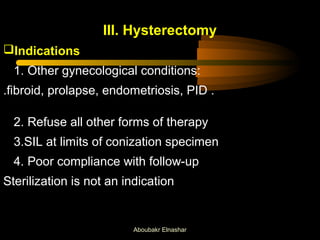
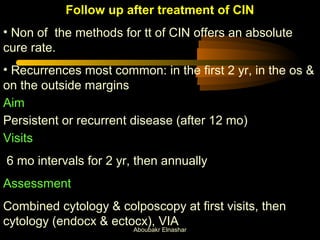
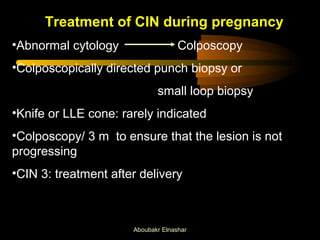
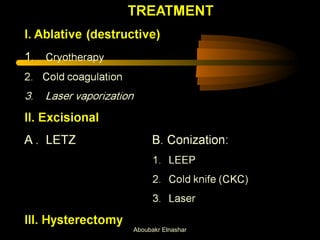
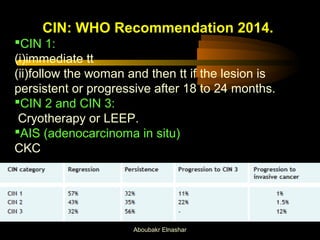
This document discusses screening and treatment strategies for cervical intraepithelial neoplasia (CIN). It recommends a see-and-treat single visit approach using cryotherapy, cold coagulation, or LEEP for lesions suggestive of significant CIN. Ablative treatments like cryotherapy are preferred for lesions entirely in the ectocervix while excisional treatments like LEEP are used for endocervical lesions or when histology is needed. Cold coagulation and LEEP have high success rates of over 95% for treating CIN while maintaining low risks. The document provides details on techniques, eligibility criteria, advantages, and disadvantages of different screening, diagnostic and treatment approaches for CIN.
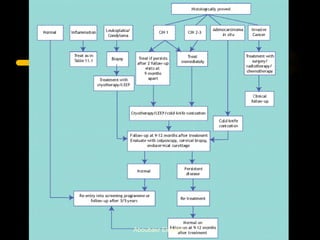
![Strategy
Three visits strategy
one for screening
one for colposcopy,
one for treatment: poor compliance, especially
among rural women.
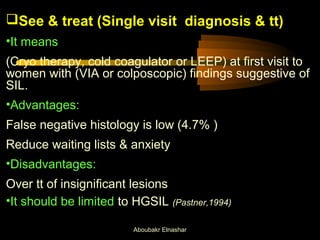
Single visit: see-and-treat strategy
satisfactory results
no significant extra morbidity
[Emam et al, 2009].
Aboubakr Elnashar](https://image.slidesharecdn.com/cintreatment-141114020637-conversion-gate01/85/CIN-treatment-4-320.jpg)