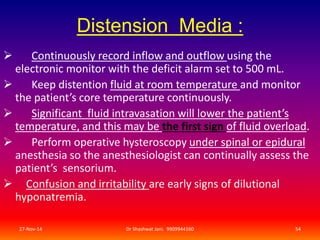
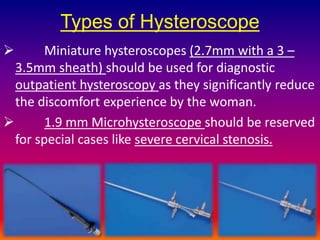
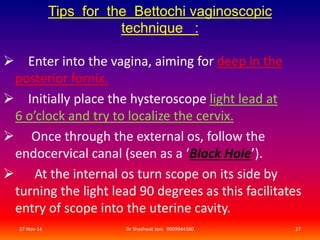
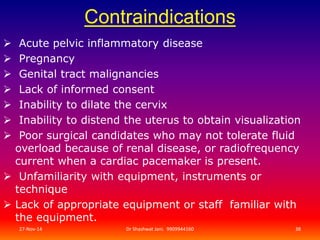
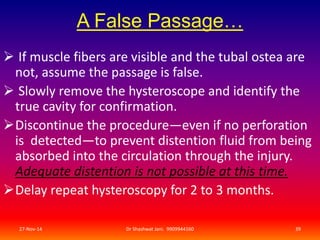
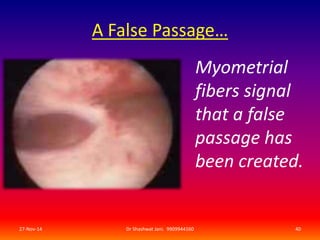
This document provides evidence-based practical tips for office hysteroscopy. It discusses appropriate patient selection, instrumentation, techniques such as the vaginoscopic approach, use of distension media, and tips for managing complications. Key recommendations include using the smallest possible hysteroscope, considering NSAIDs for analgesia, and addressing any contraindications to minimize risks. Office hysteroscopy is presented as a generally safe procedure that can provide diagnostic and some operative capabilities when performed properly.





![To achieve hemostasis
1 ) Insert a Foley catheter with a 30-cc balloon into
the uterine cavity, inject 15 to 20 mL (or more for a
larger cavity) of fluid into the balloon, and observe
the patient.
2 ) Pack the uterus.
1/2-inch–gauge packing that has been soaked in a
dilute vasopressin solution.
(20 U [1 mL] in 60 mL Normal Saline).
27-Nov-14 Dr Shashwat Jani. 9909944160 48](https://image.slidesharecdn.com/evidencebasedpracticaltipsforofficehysteroscopybydrshashwatjani-141127033612-conversion-gate02/85/EVIDENCE-BASED-PRACTICAL-TIPS-FOR-OFFICE-HYSTEROSCOPY-BY-DR-SHASHWAT-JANI-48-320.jpg)
![Benefits of Vasopressin :
Before balloon tamponade or Packing the uterus,
Inject very dilute vasopressin :
(4 U [0.2 mL] in 60 mL normal saline)
directly into the cervix 2 cm deep,
at the 4 and 8 o’clock positions.
27-Nov-14 Dr Shashwat Jani. 9909944160 49](https://image.slidesharecdn.com/evidencebasedpracticaltipsforofficehysteroscopybydrshashwatjani-141127033612-conversion-gate02/85/EVIDENCE-BASED-PRACTICAL-TIPS-FOR-OFFICE-HYSTEROSCOPY-BY-DR-SHASHWAT-JANI-49-320.jpg)