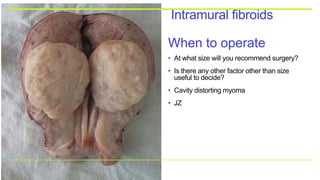
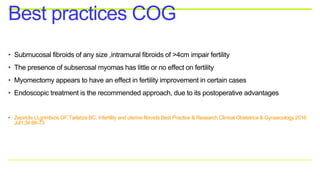
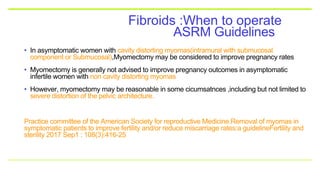
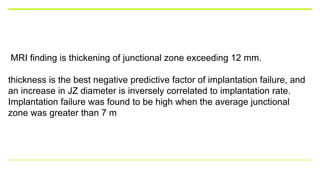
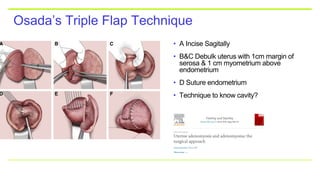
The panel discussion focused on fertility-enhancing laparoscopic surgeries, particularly addressing the role of myomas and adenomyomas in infertility. Key recommendations included considering myomectomy for cavity-distorting myomas and careful evaluation of adenomyosis, with evidence suggesting different impacts on pregnancy rates depending on surgical techniques and preoperative treatments. The discussion emphasized the need for tailored surgical approaches, balancing benefits and risks related to ovarian reserve and potential complications.