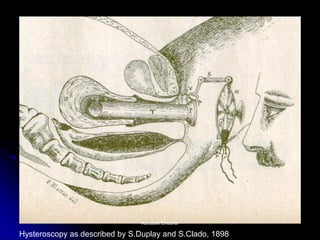
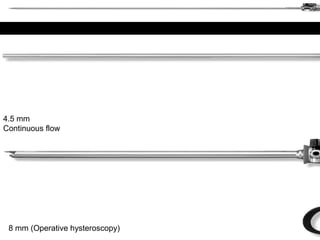
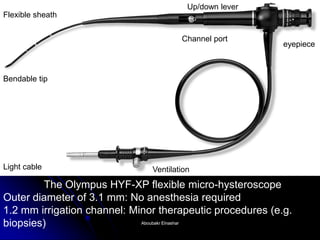
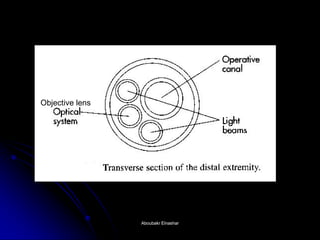
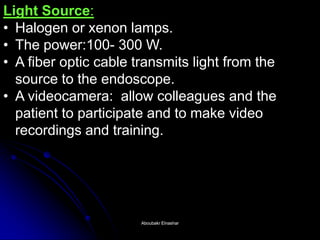
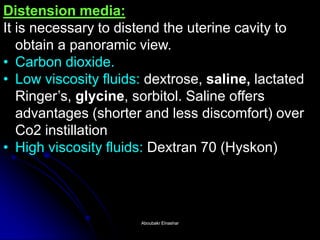
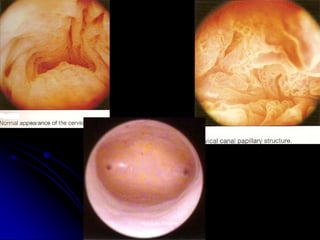
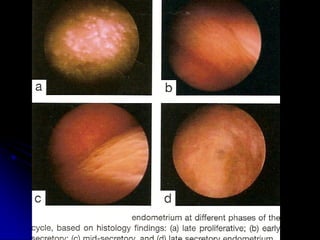
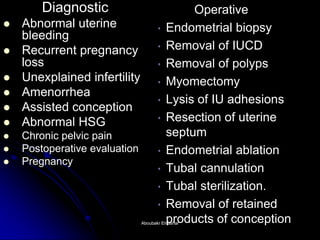
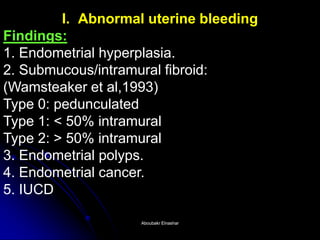
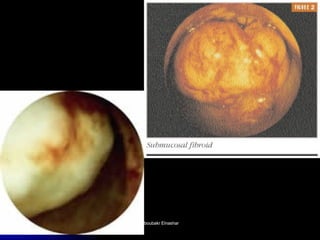
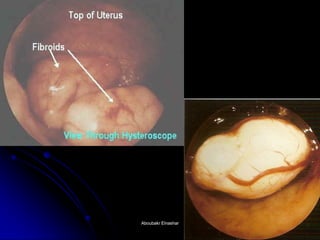
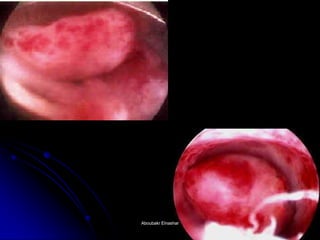
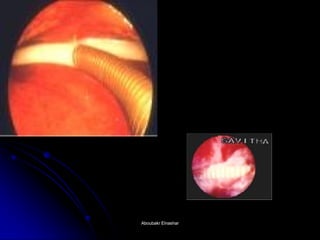
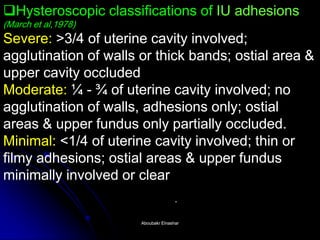
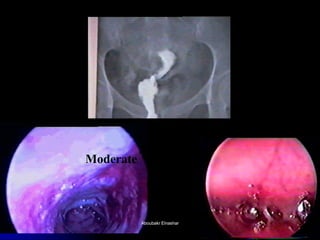
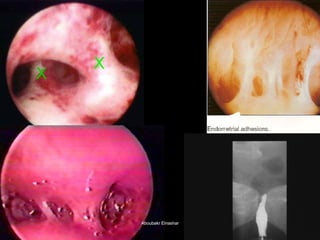
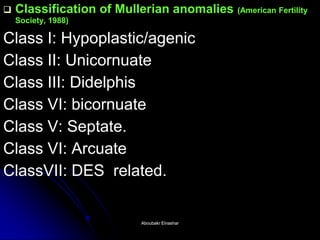
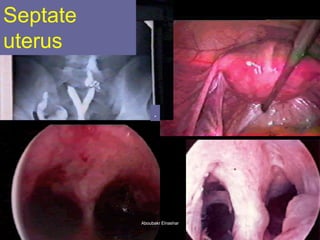
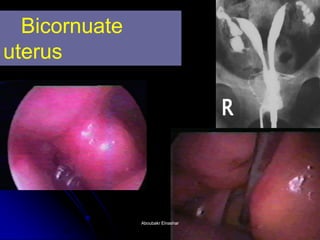
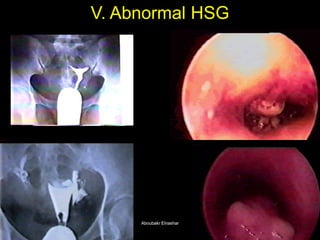
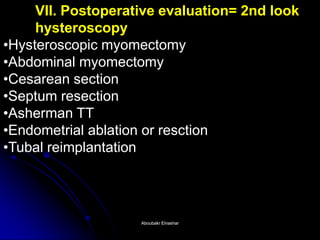
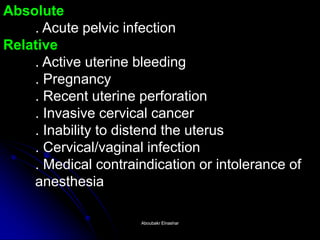
The document discusses the history and development of hysteroscopy. It began in 1869 but did not achieve routine use until improvements to optics, distension media, lighting and instruments in the 1970s-1990s allowed for office procedures without anesthesia. Today, many hysteroscopic procedures have replaced older, more invasive techniques. The document then provides details on rigid and flexible hysteroscopes, lighting sources, distension media, and diagnostic and operative uses of hysteroscopy for conditions like abnormal bleeding, infertility, uterine anomalies and assisted conception. Contraindications are also outlined.