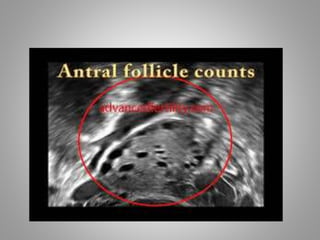
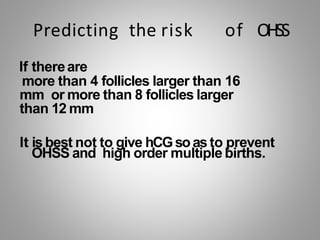
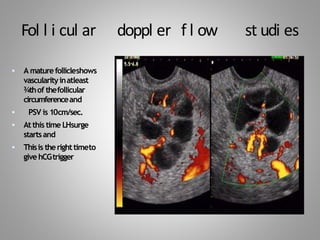
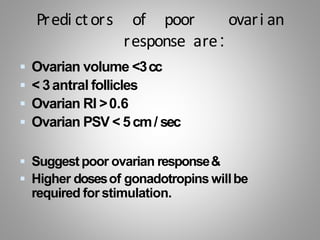
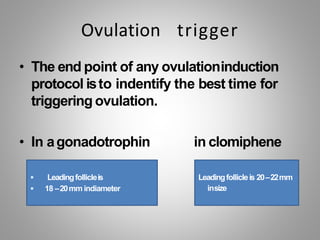
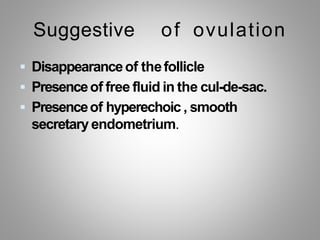
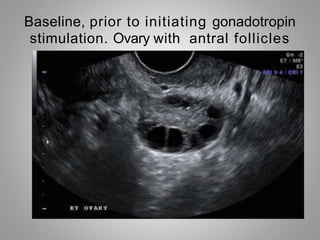
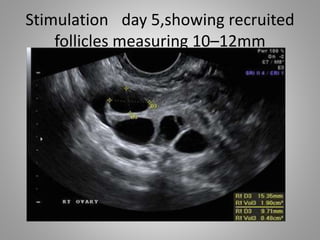
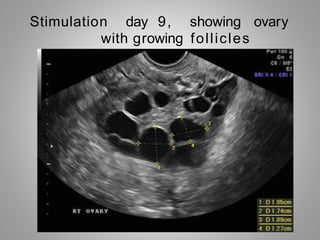
This document discusses follicular monitoring, which is used to track the growth of ovarian follicles using ultrasound. It is a vital part of assessing IVF and IUI cycles. Regular monitoring allows doctors to evaluate response to medication, adjust doses as needed, and time ovulation or procedures. Early in the cycle, several follicles are recruited and a dominant follicle is selected, growing larger each day. Monitoring involves tracking follicle size and number as well as blood flow. It helps determine when to trigger ovulation or collect eggs and can identify patients at risk for overstimulation.