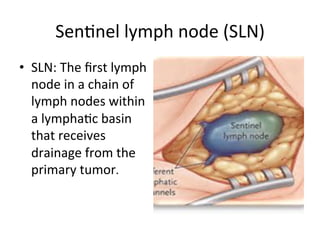
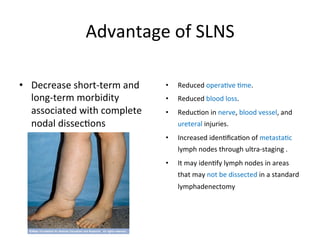
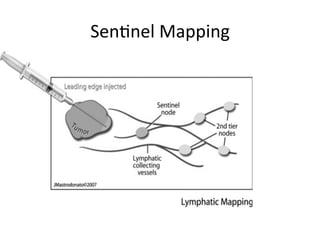
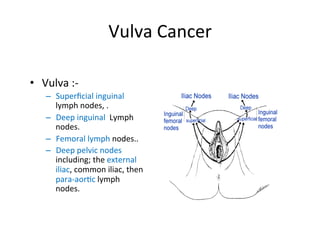
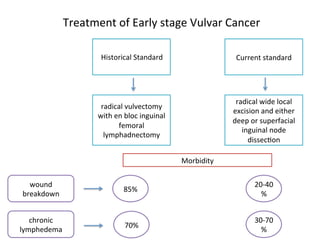
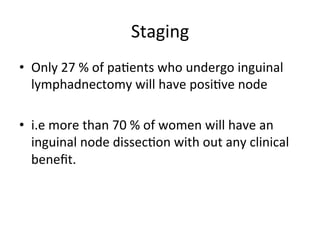
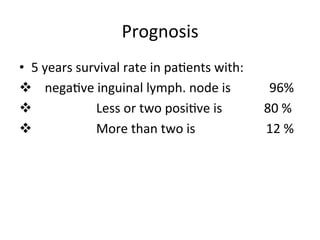
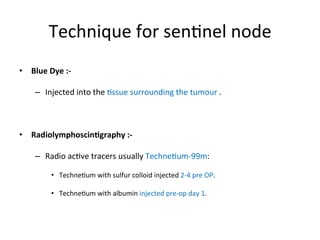
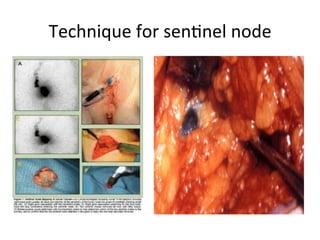
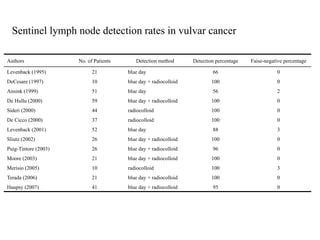
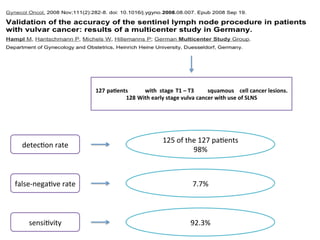
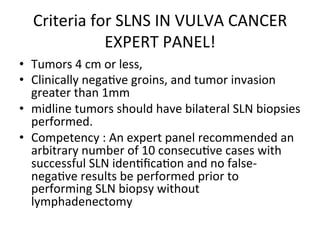
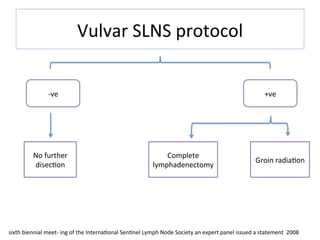
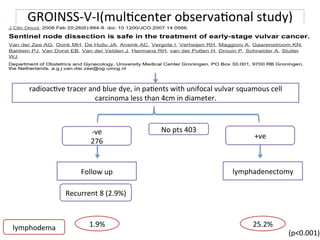
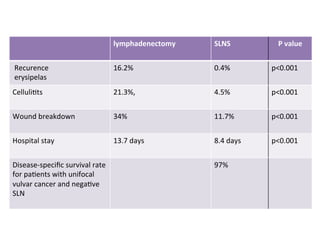
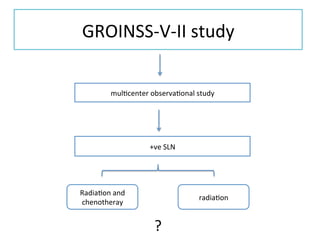
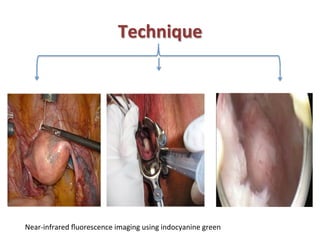
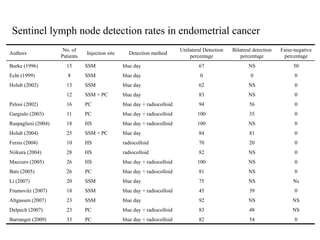
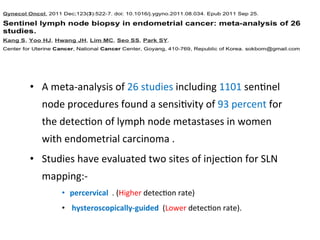
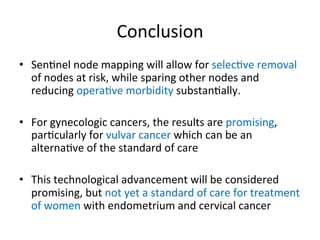
This document summarizes the use of sentinel lymph node biopsy (SLNB) in gynecological malignancies, specifically vulvar cancer. It discusses how SLNB can help stage and predict prognosis in vulvar cancer patients, with a lower morbidity than traditional inguinal lymphadenectomy. Several studies demonstrated high detection rates of over 95% and low false negative rates of less than 10% when using radiotracer and blue dye to map sentinel lymph nodes in vulvar cancer patients. Larger multicenter trials provide further support for the accuracy and reduced complications of SLNB compared to lymphadenectomy in early stage vulvar cancer.