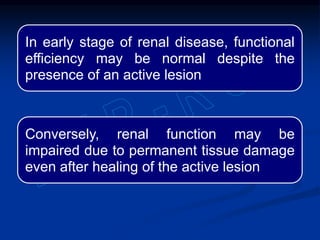
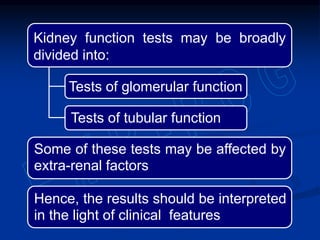
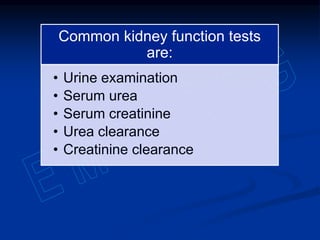
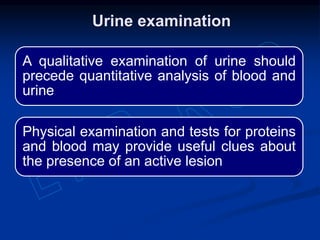
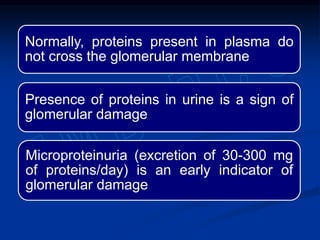
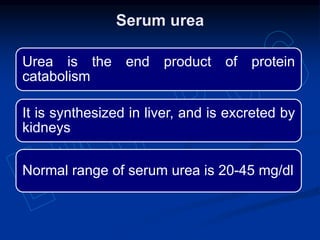
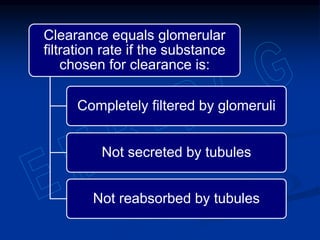
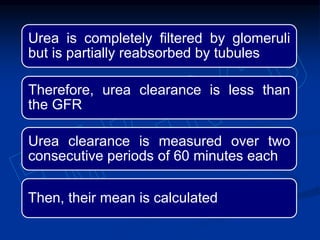
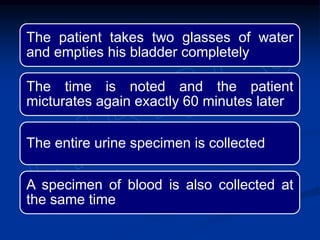
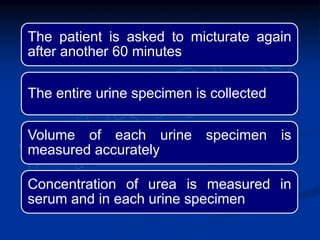
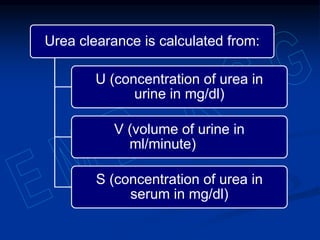
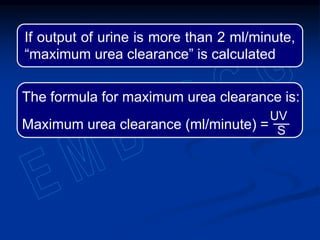
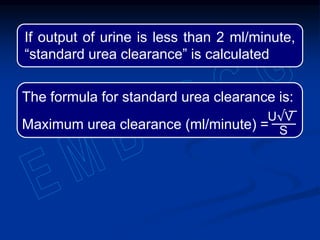
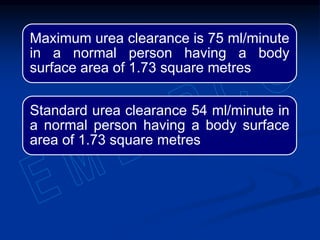
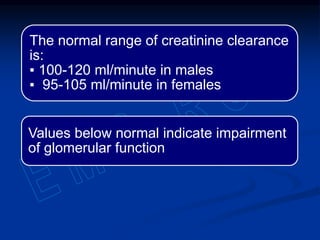
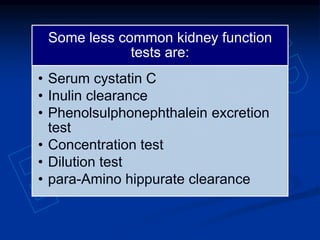
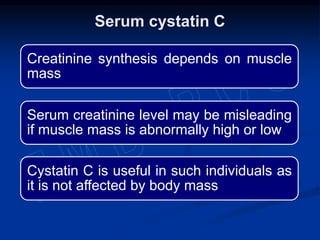
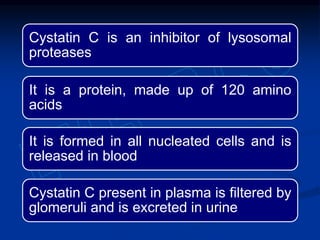
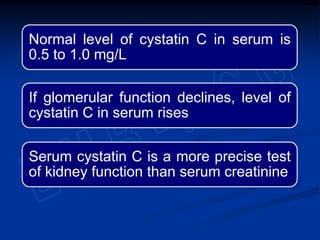
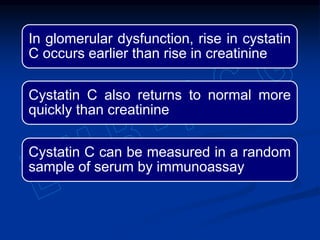
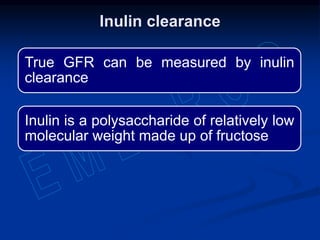
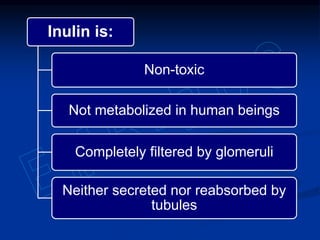
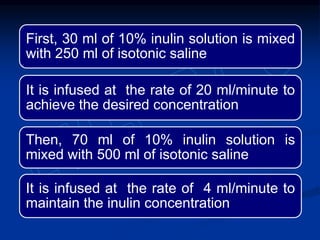
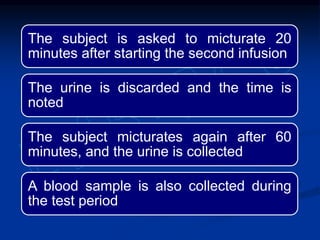
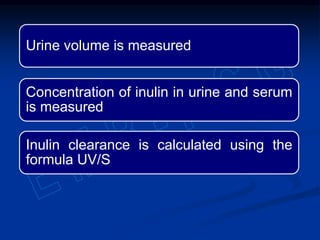
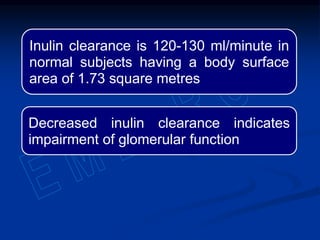
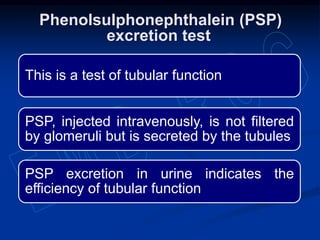
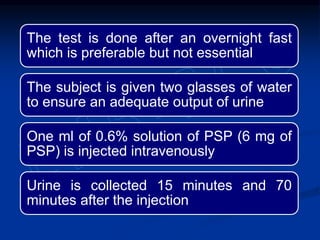
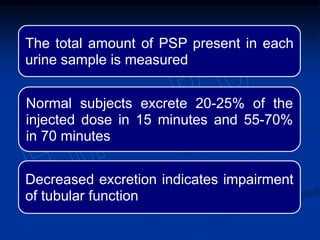
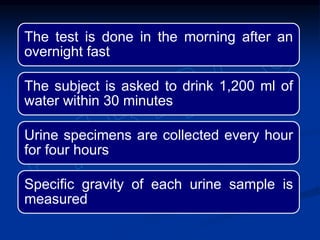
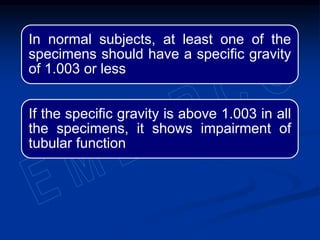
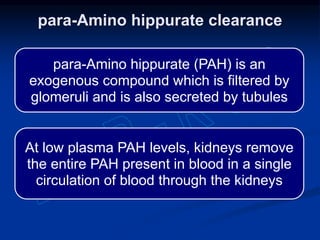
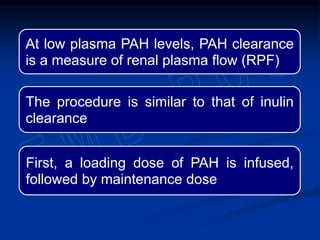
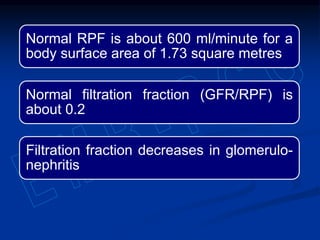
This document discusses various kidney function tests, including their purpose, methodology, and normal ranges. It describes tests of glomerular function like serum urea, serum creatinine, urea clearance, and creatinine clearance. It also covers tests of tubular function such as phenolsulphonephthalein excretion, concentration test, and dilution test. Less common tests like serum cystatin C and inulin clearance are also summarized. The document emphasizes interpreting results in light of clinical findings and notes factors that can influence certain test outcomes.